Comment on Bäumer et al, page 4754
Characterization of mouse embryos deficient in the endothelial cell–specific phosphotyrosine phosphatase, VE-PTP, reveal the critical role of this protein in the process of vasculogenesis.
Several receptor tyrosine kinases (RTKs) and their ligands are known to be critical for the process of vasculogenesis, including the RTKs Flk-1/VEGFR2, Flt-1/VEGFR1, Tie2/TEK, and Eph receptors and the ligands, VEGF, angiopoietins and ephrins.1 Activation of these RTKs is a driving force for vascular morphogenesis, including assembly of nascent blood vessels and their maturation. Prominent among these RTKs is Flk-1, whose activation by VEGF is essential for the generation of sufficient numbers of endothelial cells to build the primitive vascular networks of the early embryo. Excessive Flk-1 activation leads to vascular dysmorphogenesis that includes abnormally enlarged blood vessels. One means by which RTKs are controlled is via phosphotyrosine phosphatases (PTPs). In this issue of Blood, Baumer and colleagues report a phenotypic characterization of mice homozygous for a targeted truncation of vascular endothelial cell–specific phosphotyrosine phosphatase (VE-PTP).FIG1
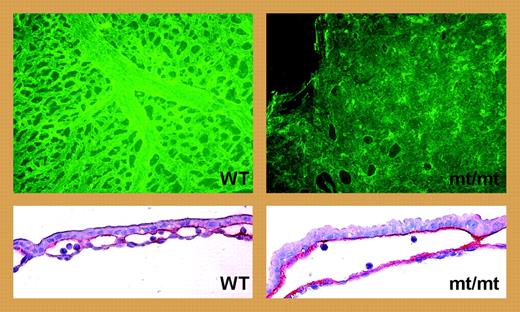
VE-PTP deficiency leads to enlarged yolk sac blood vessels. See the complete figure in the article beginning on page 4754.
VE-PTP deficiency leads to enlarged yolk sac blood vessels. See the complete figure in the article beginning on page 4754.
The vascular phenotype of mutant VE-PTP embryos is strikingly similar to that of mice homozygous for deletion of another endothelial cell PTP gene, CD148/DEP-1.2 Both mutants exhibit enlarged yolk-sac blood vessels that fail to undergo remodeling (see figure). They also display intraembryonic vascular defects that include discontinuities of the endocardium and dorsal aortae. Similar anomalies of the yolk sac and endocardium have been attributed to augmentation in VEGF levels.3,4 Indeed, VEGF-A mRNA levels increase 5- to 10-fold in yolk sacs of CD148/DEP-1–null embryos 9 to 9.5 days after coitus (dpc), and there is a greater than 50% increase in the number of endothelial cells. These findings suggested that abnormal vascular enlargement is a consequence of increased endothelial cell numbers that result from increased tyrosine kinase signaling, presumably via Flk-1.
By contrast, Bäumer et al report that there are no changes in either VEGF mRNA levels or endothelial cell numbers in VE-PTP mutants. To account for the anomalous enlargement of yolk sac blood vessels, they propose a model involving weakening of interendothelial cell contacts or sites of attachment between the endothelium and mesothelial or endodermal cells leading to dilation and fusion with adjacent vessels. Mechanistically, such effects may relate to decreased VE-cadherin–mediated endothelial cell interactions, because VE-PTP decreases the tyrosine phosphorylation level of VE-cadherin.5 The ability to dephosphorylate VE-cadherin may be a distinction between VE-PTP and CD148/DEP-1.
The VE-PTP and CD148/DEP-1 mutant mouse studies clearly demonstrate the importance of these PTPs in normal vasculogenesis, in which they act to prevent pathologic enlargement and instability of embryonic blood vessels. The apparently distinct mechanisms underlying the common phenotypic vascular anomalies of each mutant are most intriguing. The findings by Bäumer et al raise many interesting questions that will need to be addressed in follow-up studies. For instance, how can deficiency of VE-PTP promote weakening of cell-cell contacts, as the authors observe, yet leave tight junctions intact? Another important question left open is whether the VE-PTP ectodomain, which is expressed as a soluble protein in the VE-PTP mutants as a result of the gene-targeting strategy, is producing a neomorphic effect. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal