Abstract
Background
It is widely recognized that advanced age and prior thrombosis predict recurrent thrombosis in essential thrombocythemia (ET) and are used to risk-stratify patients. However, the paucity of large sample size and long-term follow-up has limited the development of similar prognostic models for survival and leukemic transformation (LT).
Methods
Data was abstracted from the medical records of a consecutive cohort of patients with WHO-defined ET seen at the Mayo Clinic. Cox proportional hazards was used to determine the impact of clinical and laboratory variables on survival and LT. Overall survival and leukemia-free survival was estimated by Kaplan-Meier plots.
Results
i. Patient characteristics and outcome
The study cohort included 605 patients of which 399 (66%) were females (median age, 57 years; range 5–91). Median follow-up was 84 months (range; 0–424). During this period, 155 patients (26%) have died and LT was documented in 20 patients (3.3%) occurring at a median of 138 months (range; 23–422) from ET diagnosis.
ii. Prognostic variables for overall survival
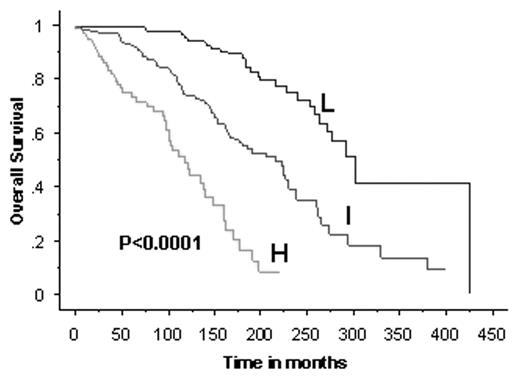
Univariate analysis of parameters at diagnosis identified age ≥ 60 years, hemoglobin less than normal (defined as < 12 g/dL in females and < 13.5 g/dL in males), leukocyte count ≥ 15 x 109/L, tobacco use, diabetes mellitus, thrombosis, male sex, and the absence of microvascular symptoms as independent predictors of inferior survival. All of the above except the last two (i.e. male sex and the absence of microvascular symptoms) sustained their prognostic significance on multivariate analysis. Based on the first three prognostic variables: age, hemoglobin level, and leukocyte count, we constructed a prognostic model for survival: low-risk (none of the risk factors), intermediate-risk (1of 3 risk factors), and high-risk (≥ 2 risk factors). The respective median survivals were 278, 200, and 111 months (p<0.0001; Figure 1)
iii. Prognostic variables for leukemic transformation
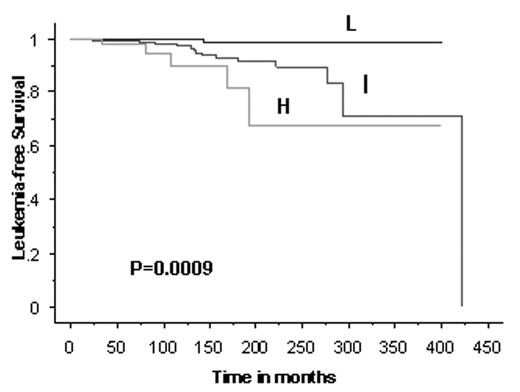
On univariate analysis of parameters at ET diagnosis, LT was significantly associated with platelet count ≥ 1000 x 109/L, hemoglobin less than normal, and exposure to P-32. However, on multivariate analysis, only hemoglobin less than normal and platelet count ≥ 1000 x 109/L maintained independent prognostic value. Accordingly, we utilized these two variables, to construct a prognostic model for LT: low-risk (none of the risk factors), intermediate-risk (1 risk factor), and high-risk (both risk factors). Only 1 of the 239 patients (0.4%) in the low-risk group vs. 14 of the 289 (4.8%) in the intermediate-risk and 5 of the 77 (6.5%) in the high-risk group underwent LT (p=0.0009; Figure 2).
Conclusion
The current study provides clinician-friendly prognostic models for both survival and LT in ET.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal