Abstract
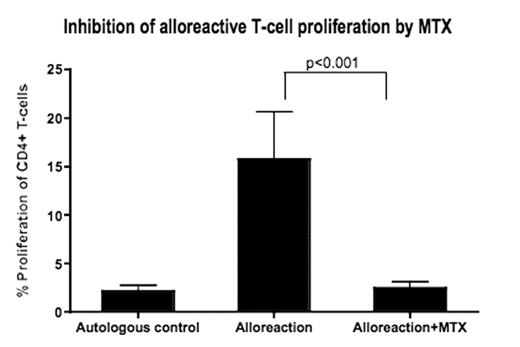
Graft-versus-Host Disease (GvHD) remains a major cause of transplant-related morbidity and mortality in recipients of allogeneic hematopoietic stem cell transplantation (AHSCT). Selective depletion of alloreactive T-cells may alleviate GvHD, while still maintaining other advantages conferred by donor T-cells, such as graft survival, antiviral immunity and graft-versus-leukemia effect. While several strategies for in vitro allodepletion have been proposed, their transition from pre-clinical studies to clinical use is sometimes hindered due to choice of reagent or technique. In this study, we evaluated the potential use of methotrexate (MTX), an FDA-approved drug known to inhibit T-cell proliferation, as an agent for specific in vitro allodepletion. Using a sensitive, flow cytometry-based proliferation assay, we first evaluated the effect of MTX on CD4+ and CD8+ T-cell proliferation in an HLA-mismatched one-way MLR. Addition of MTX resulted in significant inhibition of both CD4+ and CD8+ T-cell proliferation in MLR as well as superantigen-stimulated control reactions (n=14; p<0.001). We next evaluated whether this exposure to MTX resulted in selective allodepletion. Thus, live cells isolated from MTX-exposed MLR cultures were re-exposed to multiple stimuli, including the same allostimulus, a third-party allostimulus, cytomegalovirus (CMV) antigen and the superantigen SEB. We observed that CD4+ and CD8+ T-cell responses to same allo-stimulus were significantly abrogated, whereas T-cell responses to third-party stimuli, CMV and SEB were all preserved (n=12; p<0.01). These results provide strong pre-clinical evidence that in vitro treatment with MTX, a practical FDA-approved agent, results in specific allodepletion and may be used as an effective approach for preventing or minimizing GvHD.
Inhibition of alloreactive T-cell proliferation by MTX
Loss of response to same allostimulus with preservation of “third party” and anti-viral responses in MTX-treated T-cells
Loss of response to same allostimulus with preservation of “third party” and anti-viral responses in MTX-treated T-cells
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal