Abstract
Severe aplastic anemia (sAA) is a bone marrow failure disorder which is mostly a consequence of immunologically mediated stem cell destruction. Stem cell transplantation (SCT) from a histocompatible sibling is a treatment of choice for this disease but major obstacles in success of allogeneic SCT include graft-versus-host disease (GVHD), graft rejection and treatment related toxicities.
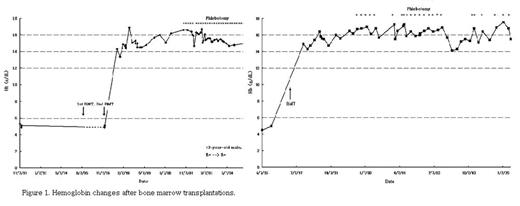
We describe two cases of post-transplant erythrocytosis in severe aplastic anemia. About 5 years later, following HLA-matched sibling transplantation, the patients (45-year-old male and 43-year-old male) developed a sustained increase in hemoglobin (>17 g/dL) and hematocrit (> 50%), an increase in the frequency of headache, and new onset of dizziness and malaise. Laboratory findings demonstrated normal ranges of other blood components and serum erythropoietin level, and they did not have smoking or other drugs. Also, they did not have a hepatosplenomegaly or other organ diseases. We initiated a therapeutic phlebotomy program (400 ml q 2–4 weeks and then q 2–3 months for 5 years) in order to lower the hematocrit to available values (Hb < 14.5 g/dL), and to induce iron deficiency (Fig 1). Repeated phlebotomy resulted in a decrease in symptoms and a total volume of blood venesection is about 9,200 – 11,200 ml so far.
Hemoglobin change after bone marrow transplantations.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal