Comment on Rezvani et al, page 1291
The relative content of Foxp3+ regulatory T cells in the donor marrow inoculum correlates with the risk of developing graft-versus-host disease after HLA-matched allogeneic stem cell transplantation.
Allogeneic stem cell transplantation has often proven a useful therapy for hematologic malignancies and other diseases over the past several decades. The major complication of allogeneic bone marrow or hematopoietic stem cell transplantation is the development of graft-versus-host disease (GVHD), in which the alloreactive T cells in the marrow inoculum respond to antigenic differences expressed on the host tissues resulting in the pathologic damage of normal host tissues. It was initially thought that GVHD was primarily due to the recognition of major histocompatibility antigen differences between donor and host. To circumvent this problem, donors and recipients were selected from sibling family members who were matched for the antigens of the major histocompatibility complex (MHC). Although the incidence of this post-transplantation complication was reduced, GVHD still occurred and required the administration of potent immunosuppressive drugs. The severity of GVHD after hematopoietic stem cell transplantation between MHC-matched siblings ranged from mild to very severe and was often life threatening. Moreover, not all patients developed GVHD. Many hypotheses have been proposed to explain the occurrence of GVHD in this setting as well as differences in incidence and severity. GVHD was attributed to recognition of minor histocompatibility antigens, minor variations in MHC antigens that could be recognized by the immune system, and the autoimmune recognition of MHC antigens.FIG1
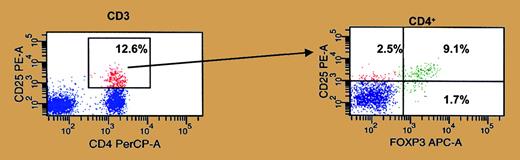
Flow cytometric identification of CD4+Foxp3+ regulatory T cells. The relative content of CD4+Foxp3+ regulatory T cells in the donor hematopoietic stem cell graft can modify the development of GVHD. See the complete figure in the article beginning on page 1291.
Flow cytometric identification of CD4+Foxp3+ regulatory T cells. The relative content of CD4+Foxp3+ regulatory T cells in the donor hematopoietic stem cell graft can modify the development of GVHD. See the complete figure in the article beginning on page 1291.
In this issue of Blood, a major factor that contributes to whether a patient receiving an MHC-matched hematopoietic stem cell transplant develops GVHD is provided by the studies by Rezvani and colleagues. The results from these studies demonstrate that the incidence and severity of GVHD correlates with the relative numbers of CD4+Foxp3+ regulatory T cells (Figure 1) contained in the marrow. Patients receiving stem cell grafts with relatively high numbers of CD4+Foxp3+ regulatory T cells had a significantly lower incidence of GVHD compared with patients receiving grafts that had low numbers of regulatory T cells. Of additional interest is the finding that the regulatory population recovers rapidly and is not affected by either treatment with the immunosuppressive drug cyclosporine A or the infusion of donor lymphocytes.
The transfer of regulatory T cells along with the marrow graft appears to prevent the subsequent development of GVHD, limiting one of the major complications of allogeneic bone marrow transplantation. The studies of Rezvani et al set the foundation for the development of strategies to engineer the hematopoietic stem cell graft expanding the CD4+Foxp3+ regulatory population ex vivo/in vitro prior to transplantation. One caveat still remains, however: will the transfer of high numbers of regulatory T cells compromise the antitumor efficacy of hematopoietic stem cell transplantation? ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal