The origin of blood-borne tissue factor (TF) is a highly debated topic that is filled with controversy. In this issue of Blood, Panes and colleagues report that activated human platelets synthesize functional TF.
Expression of TF around blood vessels is thought to initiate clotting after vessel injury. However, in 1999, Giesen et al1 demonstrated that TF was present in blood, and that this so called blood-borne TF contributed to thrombus formation ex vivo. TF was found on microparticles (MPs), which are small membrane fragments derived from activated or apoptotic cells. Positive staining was also observed on platelets and was presumably due to the adsorption of TF-positive MPs. This bred a popular concept that TF present in blood was derived from MPs. Indeed, P-selectin glycoprotein-1 expressed by leukocyte-derived MPs can dock to P-selectin present on the surface of activated platelets.2
Whether or not platelets intrinsically express TF has been controversial. In 2001, Zillman et al3 identified TF on the surface of platelets in collagen-stimulated whole blood. This observation was generally confirmed by others, and in a subsequent study, TF protein was localized to platelet α-granules. This suggested that platelets store TF, but did not distinguish between TF that was preformed in megakaryocytes and packaged into platelets versus the endocytosis of TF-positive MPs. These studies also did not take into account de novo protein synthesis, a mechanism of control used by platelets to generate new proteins.4
The studies by Panes and coworkers provide further insight into these issues and demonstrate that activated human platelets synthesize TF. They show that unstimulated platelets express low levels of TF protein, which is enhanced in response to cellular activation. TF mRNA, the template for protein synthesis, is absent or expressed at low levels in unstimulated platelets. In response to activation, however, platelets from every subject express TF mRNA. The differential expression of TF mRNA in anucleate platelets can be explained by studies from our group demonstrating that resting platelets contain TF pre-mRNA that is spliced into mature mRNA upon platelet activation.5 One limitation of the study by Panes and colleagues is that it is unclear if resting platelets express low basal levels of TF in vivo, or if these levels are due to postisolation activation of the platelets. This is a critical question to resolve, because constitutive versus inducible expression of platelet TF may have distinct functions in the initiation, propagation, and stabilization of a thrombus. It also raises the possibility that TF protein expression patterns in platelets may vary in human disease.
The fact that activated platelets express TF may have important implications for the therapeutic use of recombinant factor VIIa (NovoSeven, Clayton, NC) in the treatment of patients with bleeding disorders. High-dose recombinant factor VIIa has been proposed to restore hemostasis by binding to activated platelets in a TF-independent manner. However, low levels of TF generated by platelets may play a role in the hemostatic effects of recombinant factor VIIa. Further studies are also required to sort out the physiological relevance of platelet-derived TF and the mechanism by which TF is activated on the surface of the platelets. Answers to these types of questions will go a long way in determining whether platelet-derived TF truly comes of age.
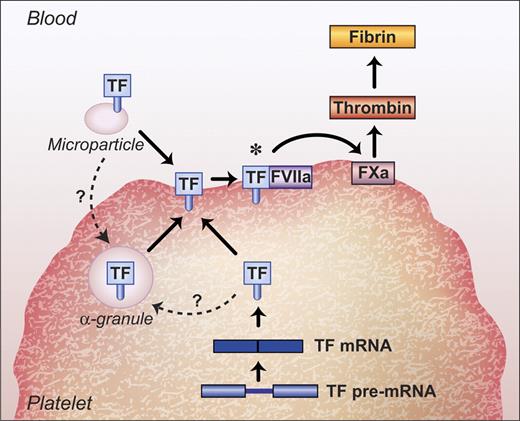
Regulation of TF in platelets. TF on the surface of activated platelets may be derived from (i) binding of TF-positive MPs, (ii) TF stored in α-granules, and (iii) splicing of TF pre-mRNA and translation of the mature mRNA into protein. Once at the cell surface, TF may require activation to reveal its procoagulant activity (*). The dashed lines with question marks identify possible sources of α-granular TF in platelets that require further investigation.
Regulation of TF in platelets. TF on the surface of activated platelets may be derived from (i) binding of TF-positive MPs, (ii) TF stored in α-granules, and (iii) splicing of TF pre-mRNA and translation of the mature mRNA into protein. Once at the cell surface, TF may require activation to reveal its procoagulant activity (*). The dashed lines with question marks identify possible sources of α-granular TF in platelets that require further investigation.
Conflict-of-interest disclosure: The authors declare no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal