Abstract
Defective regulation of platelet activation/aggregation is a predominant cause for arterial thrombosis, the major complication of atherosclerosis triggering myocardial infarction and stroke. A central regulatory pathway conveying inhibition of platelet activation/aggregation is nitric oxide (NO)/cyclic GMP (cGMP) signaling by cGMP-dependent protein kinase I (cGKI). However, the regulatory cascade downstream of cGKI mediating platelet inhibition is still unclear. Here, we show that the inositol-1,4,5-trisphosphate receptor–associated cGMP kinase substrate (IRAG) is abundantly expressed in platelets and assembled in a macrocomplex together with cGKIβ and the inositol-1,4,5-trisphosphate receptor type I (InsP3RI). cGKI phosphorylates IRAG at Ser664 and Ser677 in intact platelets. Targeted deletion of the IRAG-InsP3RI interaction in IRAGΔ12/Δ12 mutant mice leads to a loss of NO/cGMP-dependent inhibition of fibrinogen-receptor activation and platelet aggregation. Intracellular calcium transients were not affected by DEA/NO or cGMP in mutant platelets. Furthermore, intravital microscopy shows that NO fails to prevent arterial thrombosis of the injured carotid artery in IRAGΔ12/Δ12 mutants. These findings reveal that interaction between IRAG and InsP3RI has a central role in NO/cGMP-dependent inhibition of platelet aggregation and in vivo thrombosis.
Introduction
Platelet activation and aggregation at foci of vascular injury is essential for primary hemostasis, but it also initiates arterial thrombosis, the leading cause of myocardial infarction and stroke.1 The gaseous molecule nitric oxide (NO) is an endogenous platelet antagonist and inhibits platelet activation and aggregate formation both in vitro and in vivo.2-4 NO activates soluble guanylyl cyclases that initiate a subsequent rise in platelet cyclic GMP (cGMP).2,3 Several mechanisms have been proposed by which NO/cGMP signaling abolishes platelet activation and aggregation, including inhibition of G-protein–coupled receptors and rearrangement of the cytoskeleton.3,5 In addition, NO/cGMP prevents inositol-1,4,5-trisphosphate (InsP3)–mediated intracellular calcium release,3,5 the critical step in the signal transduction pathway that leads to full platelet activation.6 The cGMP-dependent protein kinase type I (cGKI) is strictly required for inhibition of platelet activation by NO/cGMP.2,7 Although cGKI has been reported to inhibit intracellular Ca2+ release in platelets,8-10 the exact molecular targets downstream of cGKI involved in NO/cGMP-dependent inhibition of platelet activation have not been defined.
In smooth muscle cells, we have identified the cGKI substrate IRAG (inositol-1,4,5-trisphosphate [InsP3] receptor–associated cGKI substrate protein), a 125-kDa protein which copurifies in a macrocomplex together with cGKI and the InsP3 receptor type I (InsP3RI).11 IRAG is essential for NO/cGMP-dependent smooth muscle cell relaxation, because it negatively regulates InsP3-induced calcium release.11,12 Because of the importance of cGKI signaling in platelets, we studied here the expression and cGKI-dependent phosphorylation of IRAG in platelets and the physiologic relevance of the IRAG-InsP3RI interaction for the regulation of platelet function. We provide first evidence that the IRAG-InsP3RI interaction mediates NO/cGMP-dependent inhibition of thrombin-induced increases in [Ca2+]i in platelets and is the major determinant of NO/cGMP-dependent prevention of platelet aggregation in vitro and arterial thrombosis in vivo.
Materials and methods
Materials
We used 8-pCPT-cGMP, Rp-8-Br-PET-cGMPS, Sp-5,6-DCl-cBIMPS (cBIMPS), 8-AET-cGMP-agarose, ethanolamine-agarose (Biolog, Bremen, Germany), forskolin (Calbiochem, Darmstadt, Germany), prostacyclin (Sigma, Deisenhofen, Germany), iloprost (Axxora, San Diego, CA), DEA/NO (Axxora), NO-spermine (Axxora), GEA-NO 3162 (Axxora), sodium nitroprusside (Sigma), protein A-sepharose (Sigma), 33 P-H3PO4 (ICN), [γ-32 P]ATP (Amersham Biosciences, Uppsala, Sweden), secondary antibodies (Dianova, Hamburg, Germany), pSer239-VASP antibody, and InsP3RI antibody (Axxora). Standard chemicals were purchased from Sigma.
Preparation of human platelets
Blood from healthy volunteers was collected in ACD-buffer and then centrifuged twice (20 minutes, 300g, room temperature [RT]). The obtained platelet-rich plasma was centrifuged (15 minutes 1500g), and the resulting platelet pellet was resuspended in HEPES buffer (10 mM HEPES, pH 7.4, 137 mM NaCl, 2.7 mM KCl, 5.5 mM glucose, 1 mM EDTA). Human platelet membranes and cytosol were isolated as described and stored at −80°C.13 Approval was obtained from the ethics committee of the faculty of medicine of the Technical University Munich for these studies. Informed consent was provided in accordance with the Declaration of Helsinki.
Phosphorylation in intact platelets
Human platelets were incubated with either HEPES buffer alone or HEPES buffer containing either 33 P-H3PO4 (1 mCi [37 MBq]/mg platelets) or 10 mM sodium phosphate and 2 mM MgCl2 (1.5 hour, 37°C) and then stimulated with diverse agents as indicated. Platelets were lysed with SDS buffer (50 mM Tris/HCl, pH 8.0, 17.3 mM SDS, 1 mM DTT) (5 minutes, 95°C). After centrifugation (30 minutes, 20 000g, 4°C) the supernatant was diluted in buffer (final concentration, 10 mM Tris/HCl, pH 7.2, 1.7 mM SDS, 24.1 mM sodium deoxycholate, 150 mM NaCl, 1.6 mM EDTA, 0.2 mM DTT, 10 mM sodium phosphate, 1% Nonidet P-40), including phosphatase inhibitors (50 mM NaF, 0.12 mM okadaic acid, 0.2 mM sodium vanadate) and protease inhibitors (0.3 mM PMSF, 1 mM benzamidine, 0.42 nM leupeptin), and then incubated with IRAG-specific antibodies bound to protein A–sepharose beads (2 hours, 4°C). Proteins were eluted with Laemmli-buffer, analyzed by SDS–polyacrylamide gel electrophoresis and Western blot followed by autoradiography, immunodecoration, or both with IRAG- or pSer677-IRAG–specific antibodies. For detection of Ser664-IRAG phosphorylation platelets were stimulated, lysed, and then analyzed by immunoblotting with pSer664-specific antibody. Mass spectrometric analysis of phosphorylated IRAG, generation of pSer664-IRAG– or pSer677-IRAG–specific antibodies, and phosphorylation of IRAG mutants in COS-7 cells is described in Document S1 (available on the Blood website; see the Supplemental Materials link at the top of the online article).
Isolation of the cGKI complex
Platelets were lysed in RIPA buffer (20 mM Tris/HCl, pH 7.4, 24.1 mM sodium deoxycholate, 150 mM NaCl, 0.5 mM EDTA, 1% Triton X-100), including protease and phosphatase inhibitors (20 minutes, 0°C). After lysis, the cGKI complex was isolated by cGMP-agarose and analyzed as described.11 As negative control, the precipitation reaction was performed with ethanolamine agarose.
Measurement of platelet aggregation
Blood from WT or IRAGΔ12/Δ12 mice14 anesthetized by diethylether inhalation was collected by cardiac puncture into 200 μL Alsever buffer (Sigma) containing 5 mM acetyl salicylic acid and 200 U/mL refludan (Schering, Berlin, Germany), mixed with 500 μL buffer B (20 mM HEPES, pH 6.2, 138 mM NaCl, 2.9 mM KCl, 1 mM MgCl2, 0.36 mM NaH2PO4) and centrifuged (15 minutes, 70g). Platelet-rich plasma was incubated with 0.3 U/mL apyrase for 5 minutes and centrifuged (5 minutes, 600g). Platelets were resuspended in buffer B (pH 7.4) at 1.5 × 105 platelets/μL containing apyrase and 5 mM glucose (1 hour, RT). For thrombin-induced aggregation, blood was drawn from isoflurane-anesthetized mice, and the use of acetylic acid, refludan, and apyrase was omitted during the isolation of platelets.
Platelets from wild-type or IRAGΔ12/Δ12 mice were preincubated (5 minutes, 37°C) and then incubated with or without 8-pCPT-cGMP (200 μM) for 10 minutes, DEA/NO (300 nM to 30 μM) for 1 minute, SNP (5-10 μM) for 2 minutes, cBIMPS (30 μM) for 5 minutes, or with prostacyclin (5 μM) for 1 minutes at 37°C. Aggregation was started by collagen (5-10 μg/mL) or thrombin (0.1 U/mL) and measured by an optical aggregometer (Chronolog, Havertown, PA) using Aggro/Link Software 5.1 (aggregation, maximal slope; Chronolog) and a pen recorder (shape change, area under the curve). All procedures performed on mice were approved by the German legislation on protection of animals.
Measurement of intracellular calcium
Platelets were isolated from isoflurane-anesthetized mice, loaded at 1 × 108 platelets/mL with Fura-2 AM (1 μM) for 45 minutes, washed, incubated with DEA/NO (10 μM in NaOH) or vehicle (100 μM NaOH) for 1 to 5 minutes or with 8-pCPT-cGMP (100-200 μM) for 10 to 30 minutes and then treated with mouse thrombin (0.4 U/mL). The ratio of the emission at 510 nm on excitation at 340 nm and 380 nm wavelength (ratio F340/380) was measured as an indicator of [Ca2+]i using the Fluostar Optima Fluorometer (BMG Labtech, Offenburg, Germany).
Platelet preparation for intravital microscopy
Donor mice of either genotype were anesthetized by inhalation of isoflurane, and 850 μL whole blood was collected by cardiac puncture into syringes containing 150 μL citrate buffer. Thereafter, 1 mL Tyrode buffer (10 mM HEPES, 1.4 M NaCl, 26 mM KCl, 121 mM NaHCO3, 0.1% BSA, 0.1% glucose, pH 6.5) was added, and the sample was centrifuged for 20 minutes at 92g. The platelet-rich plasma was further incubated with 5-carboxy-fluorescein diacetate succidinimyl ester (10 μg/mL) for 3 minutes, followed by centrifugation for 10 minutes at 1277g. Labeled platelets were then resuspended in Tyrode buffer (pH 7.4) and adjusted to a final concentration of 1.5 × 105 platelets in 250 μL.
Intravital imaging of platelet aggregation during arterial thrombosis
For fluorescence microscopy WT or IRAG mutant mice were anesthetized by intraperitoneal injection of a solution of midazolam (5 mg/kg body weight; Ratiopharm, Ulm, Germany), medetomidine (0.5 mg/kg body weight; Pfizer, New York, NY), and fentanyl (0.05 mg/kg body weight; CuraMED Pharma, Karlsruhe, Germany). A polyethylene catheter was implanted into the right jugular vein for infusion of drugs and 5-carboxy-fluorescein diacetate succidinimyl ester–labeled platelets, respectively, and the left common carotid artery was gently exposed. Subsequently, all animals received an intravenous bolus of NO-spermine (50 μM in NaOH), iloprost (50 μM), or vehicle (50 μM NaOH), as indicated. Fluorescent donor platelets of either genotype were preincubated for 2 minutes with either NO-spermine (50 μM in NaOH), iloprost (50 μM), or vehicle (50 μM NaOH) and subsequently infused intravenously. Thereafter, endothelial disruption of the carotid artery was initiated by ligation of the common carotid artery near the carotid bifurcation for 5 minutes as described in detail elsewhere.15
To directly visualize in vivo platelet aggregation in the injured carotid artery we used an intravital high-speed widefield Olympus BX51WI fluorescence microscope with a long-distance condenser and a 20 × (NA 0.95) water-immersion objective. The system is equipped with Olympus MT 20 monochromator for excitation and an F-View CCD camera (Olympus, Melville, NY). Platelet aggregation was determined using the Cap image 7.1 analysis program (Dr. Zeintl, Heidelberg, Germany) as previously described15 and is given in μm2 thrombus area.
Alexa 488–fibrinogen binding
Platelets were isolated from mice anaesthetized by isoflurane inhalation, incubated at 2 × 106 platelets/mL with DEA/NO (100 nM) or iloprost (10 μM) for 2 minutes, 8-pCPT-cGMP (200 μM) or cBIMPS (30 μM) for 10 minutes at RT and then treated with mouse thrombin (0.1 U/mL) or PBS and Alexa 488–labeled fibrinogen (12.5 μg/mL) for 10 minutes at RT. The samples were fixed with 1% paraformaldehyde. Fluorescence was measured using a fluorescence-activated cell sorting (FACS)Calibur flow cytometer (BD Biosciences, Heidelberg, Germany) (excitation, 488 nm; emission, 520 nm).
Regulation of GPIIb-IIIa activation
Platelets were isolated from isoflurane-anesthetized WT or IRAGΔ12/Δ12 mice, incubated at 5 × 107 platelets/mL with DEA-NO (100 μM in NaOH) or vehicle (100 μM NaOH) for 2 minutes or with 8-pCPT-cGMP (200 μM) for 10 minutes at RT, and then treated with mouse thrombin (0.05 U/mL) or PBS for 10 minutes at RT. Expression of the activation-dependent high-affinity conformation of GPIIb-IIIa (αIIbβ3 integrin) was determined using PE-labeled JON/A antibody (Emfret, Würzburg, Germany).16,17 Fluorescence was measured on a FACSCalibur flow cytometer (BD Biosciences). Data are given as absolute increase in mean fluorescence intensity compared with resting platelets.
Calculation and statistics
All data are expressed as mean ± SEM. (Error bars in figures indicate SEM.) For the calculation of statistical differences between 2 means the unpaired Student t test was used. The significance of P value was indicated by asterisks (*P < .05; **P < .01; ***P < .001; NS, not statistically significant); n indicates the number of experiments.
Results
Assembly of the cGKI macrocomplex in platelets
IRAG is expressed abundantly in the membrane fraction of platelets together with cGKIβ (Figure 1A). In human platelets only the β-isoform of cGKI is present (Figure 1A), whereas murine platelets contain in addition a small amount of cGKIα (Figure S1A). In both human and murine platelets, IRAG copurifies with InsP3RI and cGKIβ on a cGMP agarose column (Figure 1B; Figure S1C), whereas these proteins were not precipitated by the negative control column ethanolamine agarose (data not shown), indicating that platelet IRAG is assembled in a stable macrocomplex consisting of InsP3RI, IRAG, and cGKIβ. The vasodilator-stimulated phosphoprotein (VASP), a cGKI substrate associated with the cytoskeleton, was not found in the purified complex, suggesting that VASP is not stably associated with cGKIβ (Figure 1B).
cGKI macrocomplex and IRAG phosphorylation in human platelets. (A) Identification of IRAG and cGKIβ in human platelets (P-M indicates platelet membranes; P-C, platelet cytosol) by immunoblot analysis with specific antibodies directed against IRAG, cGKIα, or cGKIβ. (B) Isolation and phosphorylation of the ternary complex of IRAG, cGKI, and InsP3RI in human platelets. The complex was isolated using cGMP agarose beads and then phosphorylated by the addition of 8-pCPT-cGMP (3 μM) and [γ-32 P]ATP. 32 P-phosphorylation was analyzed by autoradiography (AR), and immunoblot analysis (IB) was performed with specific antibodies. The positions of molecular weight markers are indicated. Note that the cGKI substrate VASP was not assembled in the cGKI complex. (C) 33 P-phosphorylation of IRAG in intact human platelets stimulated with the cGMP analog 8-pCPT-cGMP (100 μM) for 1 to 30 minutes. (D) Stimulation of human platelets with the nitric oxide donor GEA-NO (100 μM). As control, in each experiment the phosphorylation of IRAG was compared with that of Ser239-VASP, determined by immunoblot analysis with pSer239-VASP–specific antibodies. Equal amounts of total IRAG or VASP in the different lanes were checked by immunoblotting with IRAG- and VASP-specific antibodies (C-D). (E) Statistics of phosphorylation with 8-pCPT-cGMP.
cGKI macrocomplex and IRAG phosphorylation in human platelets. (A) Identification of IRAG and cGKIβ in human platelets (P-M indicates platelet membranes; P-C, platelet cytosol) by immunoblot analysis with specific antibodies directed against IRAG, cGKIα, or cGKIβ. (B) Isolation and phosphorylation of the ternary complex of IRAG, cGKI, and InsP3RI in human platelets. The complex was isolated using cGMP agarose beads and then phosphorylated by the addition of 8-pCPT-cGMP (3 μM) and [γ-32 P]ATP. 32 P-phosphorylation was analyzed by autoradiography (AR), and immunoblot analysis (IB) was performed with specific antibodies. The positions of molecular weight markers are indicated. Note that the cGKI substrate VASP was not assembled in the cGKI complex. (C) 33 P-phosphorylation of IRAG in intact human platelets stimulated with the cGMP analog 8-pCPT-cGMP (100 μM) for 1 to 30 minutes. (D) Stimulation of human platelets with the nitric oxide donor GEA-NO (100 μM). As control, in each experiment the phosphorylation of IRAG was compared with that of Ser239-VASP, determined by immunoblot analysis with pSer239-VASP–specific antibodies. Equal amounts of total IRAG or VASP in the different lanes were checked by immunoblotting with IRAG- and VASP-specific antibodies (C-D). (E) Statistics of phosphorylation with 8-pCPT-cGMP.
Phosphorylation of IRAG by cGKI
We show here that platelet IRAG is phosphorylated in an NO/cGMP-dependent manner in vitro and in intact platelets. Activated cGKI phosphorylated IRAG, InsP3RI, and cGKIβ in the isolated complex from platelets (Figure 1B). IRAG was also phosphorylated by cGKI when intact human platelets were preincubated with 8-pCPT-cGMP (Figure 1C) or the NO donor GEA-NO (Figure 1D). Within 1 to 5 minutes after addition of 8-pCPT-cGMP or GEA-NO, IRAG phosphorylation increased up to 2.5-fold (Figure 1C-E; data not shown). The kinetics of IRAG phosphorylation were similar to that of VASP.18
Previously, we have identified several in vitro phosphorylation sites of IRAG isolated from bovine tracheal smooth muscle membranes.11 To define which of these sites was phosphorylated in platelets in response to NO/cGMP, IRAG (approximately 2 μg) was purified from 8-pCPT-cGMP–treated or nontreated human platelets and analyzed by mass spectrometry using nanoelectrospray-based ion scanning (data not shown). Three phosphorylated serine residues were identified, Ser374, Ser664, and Ser677. Although Ser664 was phosphorylated only in response to cGMP, Ser374 showed constitutive phosphorylation in both nontreated and treated platelets. In contrast, phosphorylation of Ser677 was observed in resting platelets (1 peptide peak) with a substantial increase in the presence of cGMP (3 peptide peaks).
We then determined the phosphorylation kinetics of the individual IRAG phosphorylation sites. We generated antibodies that specifically detect pSer664 or pSer677 phosphorylation using chemically synthesized phosphorylated peptides as immunogens (Figure S2). These antibodies showed that both cGMP and NO strongly increase the phosphorylation at Ser664 and Ser677 in human platelets (Figure 2A-B; Figure S2C). The cGKI inhibitor Rp-8-Br-PET-cGMPS prevented NO/cGMP-induced phosphorylation (Figure 2A-B; data not shown) of Ser664 and Ser677, suggesting that both serines were in fact phosphorylated by cGKI. The specificity of Rp-8-Br-PET-cGMPS on NO signaling was demonstrated previously because Rp-8-Br-PET-cGMPS inhibited NO/cGMP-induced VASP phosphorylation19 and reversed NO-mediated inhibition of platelet aggregation.20 Consistently, we detected that Rp-8-Br-PET-cGMPS (200 μM, 20 minutes of preincubation) suppressed the effect of DEA/NO (300 nM, 1 minute of preincubation) on collagen (10 μg/mL)–induced platelet aggregation in human platelet-rich plasma, whereas Rp-8-Br-PET-cGMPS alone did not significantly affect platelet aggregation. (Aggregation: +NO, 35.1% ± 5.8% of control [n = 7]; +NO/Rp, 78.2% ± 2.8% of control [n = 7]; Rp, 90.7% ± 1.7% of control [n = 4]).
Analysis of IRAG phosphorylation in intact human platelets with pSer664-IRAG and pSer677-IRAG antibodies. (A-B) Phosphorylation of IRAG stimulated in human platelets by 8-pCPT-cGMP (100 μM, 30 minutes) or by DEA/NO (10 μM, 1 minute). Reactions were preincubated with the cGMP kinase inhibitor Rp-8-Br-PET-cGMPS (200 μM, 20 minutes) where indicated. IRAG phosphorylation was analyzed by pSer664-IRAG antibody (A) or pSer677-IRAG antibody (B). Control conditions were performed for 8-pCPT-cGMP by adding H2O and for DEA/NO by adding a final concentration of 1 mM NaOH to the reaction. (C, top) Kinetics of IRAG phosphorylation in human platelets by 8-pCPT-cGMP or by DEA/NO. IRAG phosphorylation was analyzed by pSer664-IRAG antibody. (C, bottom) Statistics of phosphorylation results in percentage of maximal Ser664 phosphorylation. Phosphorylation of VASP analyzed by the phosphospecific pSer239-VASP antibody and immunodecoration with IRAG- and VASP-specific antibodies are shown for comparison.
Analysis of IRAG phosphorylation in intact human platelets with pSer664-IRAG and pSer677-IRAG antibodies. (A-B) Phosphorylation of IRAG stimulated in human platelets by 8-pCPT-cGMP (100 μM, 30 minutes) or by DEA/NO (10 μM, 1 minute). Reactions were preincubated with the cGMP kinase inhibitor Rp-8-Br-PET-cGMPS (200 μM, 20 minutes) where indicated. IRAG phosphorylation was analyzed by pSer664-IRAG antibody (A) or pSer677-IRAG antibody (B). Control conditions were performed for 8-pCPT-cGMP by adding H2O and for DEA/NO by adding a final concentration of 1 mM NaOH to the reaction. (C, top) Kinetics of IRAG phosphorylation in human platelets by 8-pCPT-cGMP or by DEA/NO. IRAG phosphorylation was analyzed by pSer664-IRAG antibody. (C, bottom) Statistics of phosphorylation results in percentage of maximal Ser664 phosphorylation. Phosphorylation of VASP analyzed by the phosphospecific pSer239-VASP antibody and immunodecoration with IRAG- and VASP-specific antibodies are shown for comparison.
Phosphorylation of Ser664 and Ser677 occurred rapidly, reaching a maximum within 1 to 3 minutes after the addition of NO (Figure 2C; data not shown). Likewise, the stable cGMP analog 8-pCPT-cGMP led to a strong and long-lasting phosphorylation at Ser664. The time course of Ser664 and Ser677 phosphorylation matched that of NO/cGMP-stimulated 33 P-phosphorylation of IRAG (Figure 1C-D) and paralleled the phosphorylation of VASP at Ser239 (Figure 2). These results indicate that IRAG is expressed in platelets and is phosphorylated by cGKI at Ser664 and Ser677 in intact platelets. Ser677 of human IRAG (GenBank accession no. NP_006060) is homologous to the bovine Ser696.11 Phosphorylation of IRAG at the Ser677 homologue is essential for cGKI-induced inhibition of InsP3-stimulated Ca2+ release,12 suggesting that IRAG phosphorylation mediates NO/cGMP-dependent inhibition of agonist-induced Ca2+ release in platelets.8-10,21
Role of IRAG in NO/cGMP-dependent platelet signaling
Next, we investigated the functional relevance of IRAG for NO/cGMP-dependent signaling in platelets. We used murine IRAGΔ12/Δ12 loss-of-function mutants that have a targeted deletion of the N-terminal part of the coiled-coil domain of IRAG required for the interaction with the InsP3RI.14 IRAGΔ12 protein expression was reduced by approximately 80% in homozygous IRAGΔ12/Δ12 platelets, whereas the expression of cGKIβ and cGKIα was not significantly affected (Figure S1A). Furthermore, NO and cGMP-dependent phosphorylation of VASP-Ser239, was identical in WT and mutant platelets, suggesting the same cGKI activity in both types of platelets22,23 (Figure S1B). In IRAGΔ12/Δ12 platelets, the InsP3RI did not copurify with IRAG and cGKI (Figure S1C), indicating that the InsP3RI is not integrated into the IRAGΔ12-cGKI macrocomplex in mutant platelets as previously reported for smooth muscle.14
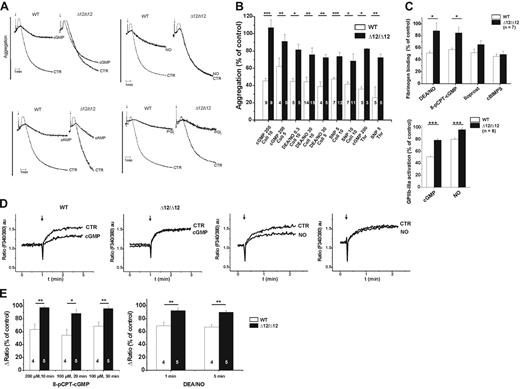
Both WT and IRAGΔ12/Δ12 platelets, which were isolated in the presence of acetyl salicylic acid, the thrombin inhibitor refludan, and the ATP/ADP-degrading enzyme apyrase to prevent prior platelet activation, readily aggregated in response to collagen (Figure 3A). Pretreatment of WT platelets with 8-pCPT-cGMP, DEA/NO, and SNP virtually abolished aggregation (Figure 3A-B). Aggregation of mutant IRAGΔ12/Δ12 platelets was not affected by 8-pCPT-cGMP and was weakly inhibited at low or high concentrations of the 2 different NO donors DEA/NO (300 nM, 30 μM) or SNP (5 μM, 10 μM). However, aggregation of wild-type and mutant platelets was strongly inhibited by the cAMP analog cBIMPS or prostacyclin (Figure 3A-B; Figure S3). Different concentrations of the agonist collagen (5 and 10 μg/mL) were used to exclude the possibility that an altered agonist response of the mutant was responsible for the abolished NO/cGMP-dependent inhibition of platelet aggregation. Furthermore, when crossactivation pathways were not blocked, omitting acetyl salicylic acid, refludan, and apyrase during platelet isolation, NO- and cGMP-mediated inhibition of collagen-induced platelet aggregation was still strongly suppressed in IRAGΔ12/Δ12 platelets in comparison to WT platelets (WT + cGMP [n = 4], 49.3% ± 2.3% of control; WT + SNP [n = 6], 46.6% ± 3.7% of control; Δ12 + cGMP [n = 10], 72.4% ± 4.6% of control; Δ12 + SNP [n = 9], 67.7% ± 2.8% of control; cGMP, 200 μM 8-pCPT-cGMP; SNP, 5 μM SNP). In contrast to aggregation, collagen-induced shape change was only affected by cAMP (Figure S3) but not by NO/cGMP/IRAG (data not shown).
Ex vivo analysis of wild-type and IRAGΔ12/Δ12 platelets. (A) Effect of 8-pCPT-cGMP (200 μM), DEA/NO (30 μM), cBIMPS (30 μM), or prostacyclin (5 μM) on collagen-induced aggregation of wild-type (WT) and IRAGΔ12/Δ12 (Δ12/Δ12) platelets. Representative traces of wild-type and IRAGΔ12/Δ12 platelets are shown. The arrow indicates the addition of collagen (10 μg/mL) (CTR indicates control without addition of 8-pCPT-cGMP, DEA/NO, cBIMPS, or prostacyclin). (B) Statistical evaluation of 8-pCPT-cGMP (200 μM), DEA/NO (0.3 μM, 30 μM), or SNP (5 μM, 10 μM) on platelet aggregation induced by collagen (5 or 10 μg/mL, as indicated) or thrombin (0.1 U/mL). (C, top) Statistical evaluation of fibrinogen binding to wild-type and IRAGΔ12/Δ12 platelets after pretreatment with 8-pCPT-cGMP (200 μM), DEA/NO (100 nM), iloprost (10 μM), or cBIMPS (30 μM) followed by induction of fibrinogen receptor activation with thrombin (0.1 U/mL). (C, bottom) Statistical evaluation of GPIIb-IIIa activation of wild-type and IRAGΔ12/Δ12 platelets after pretreatment with 8-pCPT-cGMP (200 μM) or DEA/NO (100 μM) followed by platelet activation with thrombin (0.05 U/mL). (D) Effect of 8-pCPT-cGMP (200 μM, 10 minutes of preincubation) or DEA/NO (10 μM, 1 minute of preincubation) on thrombin-induced calcium release of Fura-2 AM (1 μM) loaded wild-type and IRAGΔ12/Δ12 platelets. Representative traces of wild-type and IRAGΔ12/Δ12 platelets are shown. The arrow indicates the addition of thrombin (0.4 U/mL) (CTR indicates control without addition of 8-pCPT-cGMP, DEA/NO; au, arbitrary units). (E) Statistical evaluation of thrombin-induced calcium release in wild-type and IRAGΔ12/Δ12 platelets. Fura-2 AM (1 μM) loaded platelets were incubated with DEA/NO (10 μM, 1-5 minutes) or 8-pCPT-cGMP (100-200 μM, 10-30 minutes) and then stimulated with thrombin (0.4 U/mL).
Ex vivo analysis of wild-type and IRAGΔ12/Δ12 platelets. (A) Effect of 8-pCPT-cGMP (200 μM), DEA/NO (30 μM), cBIMPS (30 μM), or prostacyclin (5 μM) on collagen-induced aggregation of wild-type (WT) and IRAGΔ12/Δ12 (Δ12/Δ12) platelets. Representative traces of wild-type and IRAGΔ12/Δ12 platelets are shown. The arrow indicates the addition of collagen (10 μg/mL) (CTR indicates control without addition of 8-pCPT-cGMP, DEA/NO, cBIMPS, or prostacyclin). (B) Statistical evaluation of 8-pCPT-cGMP (200 μM), DEA/NO (0.3 μM, 30 μM), or SNP (5 μM, 10 μM) on platelet aggregation induced by collagen (5 or 10 μg/mL, as indicated) or thrombin (0.1 U/mL). (C, top) Statistical evaluation of fibrinogen binding to wild-type and IRAGΔ12/Δ12 platelets after pretreatment with 8-pCPT-cGMP (200 μM), DEA/NO (100 nM), iloprost (10 μM), or cBIMPS (30 μM) followed by induction of fibrinogen receptor activation with thrombin (0.1 U/mL). (C, bottom) Statistical evaluation of GPIIb-IIIa activation of wild-type and IRAGΔ12/Δ12 platelets after pretreatment with 8-pCPT-cGMP (200 μM) or DEA/NO (100 μM) followed by platelet activation with thrombin (0.05 U/mL). (D) Effect of 8-pCPT-cGMP (200 μM, 10 minutes of preincubation) or DEA/NO (10 μM, 1 minute of preincubation) on thrombin-induced calcium release of Fura-2 AM (1 μM) loaded wild-type and IRAGΔ12/Δ12 platelets. Representative traces of wild-type and IRAGΔ12/Δ12 platelets are shown. The arrow indicates the addition of thrombin (0.4 U/mL) (CTR indicates control without addition of 8-pCPT-cGMP, DEA/NO; au, arbitrary units). (E) Statistical evaluation of thrombin-induced calcium release in wild-type and IRAGΔ12/Δ12 platelets. Fura-2 AM (1 μM) loaded platelets were incubated with DEA/NO (10 μM, 1-5 minutes) or 8-pCPT-cGMP (100-200 μM, 10-30 minutes) and then stimulated with thrombin (0.4 U/mL).
Furthermore, we tested whether induction by another agonist (eg, thrombin), which leads to Gq-activation and thereby stimulation of phospholipase Cβ,24 can be affected by IRAG signaling. Both NO- and cGMP-mediated inhibition of thrombin-induced platelet aggregation was suppressed by the IRAG mutation (Figure 3B). Therefore, it can be concluded that signaling by IRAG is a major pathway of NO/cGMP impeding platelet aggregation.
Previously, we have reported that, apart from preventing platelet aggregation, the NO/cGMP/cGKI cascade negatively regulates agonist-induced activation of the platelet fibrinogen receptor GPIIb-IIIa.7 Both, cGMP and NO significantly attenuated thrombin-induced fibrinogen binding to WT, but not to IRAGΔ12/Δ12 platelets (Figure 3C, left). Correspondingly, direct fibrinogen receptor GPIIb-IIIa activation by thrombin was only slightly reduced by cGMP and NO in mutant platelets in contrast to wild-type platelets (Figure 3C, right). By contrast, prostacyclin or cAMP reduced fibrinogen binding to a similar extent in both WT and IRAGΔ12/Δ12 platelets (Figure 3C, left).
Furthermore, preincubation of mutant platelets with 8-pCPT-cGMP or DEA/NO hardly affected thrombin-induced calcium transients in contrast to wild-type platelets (Figure 3D-E). Together these results indicated that IRAG is specifically involved in the cGMP/cGKI signaling cascade leading to inhibition of platelet activation and aggregation by suppression of intracellular calcium transients, whereas the cAMP/cAK cascade is unaffected by the IRAG mutation.
IRAG function in NO/cGMP-dependent prevention of thrombus formation
To further dissect the biologic role of platelet IRAG, we directly visualized platelet aggregation and thrombus formation following vascular injury using in situ high-speed intravital microscopy of the mouse carotid artery. In the injured carotid artery, WT and IRAGΔ12/Δ12 platelets readily adhered (data not shown) and aggregated to a similar extent at the site of injury leading to local thrombus formation (Figure 4A-B). The stable NO analog NO-spermine abolished platelet aggregate formation in WT mice. In striking contrast, NO did not affect thrombus formation in IRAGΔ12/Δ12 mutants (Figure 4B; Videos S1–S4). Infusion of donor platelets into heteroacceptor mice (IRAGΔ12/Δ12 platelets in WT mice, WT platelets in IRAGΔ12/Δ12 mice) revealed that a defective function of the mutant platelets was responsible for the lack of NO-mediated suppression of arterial thrombus formation (Figure 4C). These results confirm that platelet IRAG is essential for NO/cGMP-dependent inhibition of platelet activation and prevention of arterial thrombosis. The contribution of IRAG is specific for cGMP/cGKI signaling because cAK activation by iloprost prevented platelet aggregation to a similar extent in both IRAGΔ12/Δ12 mutants and WT mice (Figure 4A-B).
In vivo analysis of arterial thrombosis in wild-type and IRAGΔ12/Δ12 mice. (A) Thrombus formation in the injured carotid artery of wild-type (WT) and IRAGΔ12/Δ12 mice in the absence or presence of NO (50 μM NO-spermine) or PGI2 (50 μM iloprost) (arrowheads indicate thrombi; arrows, single, adherent platelets). (B) Statistical evaluation of thrombus formation as measured by the size of platelet aggregates (in μm2) Analysis was performed with n = 6 to 9 PBS-, vehicle (NaOH)–, NO- or PGI2-treated WT or IRAG mutant mice. (C) Thrombus formation after infusion of IRAGΔ12/Δ12 or WT platelets into the injured carotid artery of WT or IRAGΔ12/Δ12 mice (recipient), respectively, in the presence of NO (50 μM NO-spermine) (arrowheads indicate thrombi, n = 4). Representative videoclips of thrombus formation in WT or IRAGΔ12/Δ12 mice from panel A in the presence or absence of nitric oxide are available as Videos S1–S4.
In vivo analysis of arterial thrombosis in wild-type and IRAGΔ12/Δ12 mice. (A) Thrombus formation in the injured carotid artery of wild-type (WT) and IRAGΔ12/Δ12 mice in the absence or presence of NO (50 μM NO-spermine) or PGI2 (50 μM iloprost) (arrowheads indicate thrombi; arrows, single, adherent platelets). (B) Statistical evaluation of thrombus formation as measured by the size of platelet aggregates (in μm2) Analysis was performed with n = 6 to 9 PBS-, vehicle (NaOH)–, NO- or PGI2-treated WT or IRAG mutant mice. (C) Thrombus formation after infusion of IRAGΔ12/Δ12 or WT platelets into the injured carotid artery of WT or IRAGΔ12/Δ12 mice (recipient), respectively, in the presence of NO (50 μM NO-spermine) (arrowheads indicate thrombi, n = 4). Representative videoclips of thrombus formation in WT or IRAGΔ12/Δ12 mice from panel A in the presence or absence of nitric oxide are available as Videos S1–S4.
Discussion
The results of this study clearly establish IRAG as a major player in the inhibition of platelet aggregation by the NO/cGMP signaling cascade. They resolve, at least in part, the signaling cascade downstream of cGKI in platelets. As already shown for smooth muscle,14 IRAG is assembled in a macrocomplex in platelets consisting of IRAG, cGKI, and InsP3RI. IRAGΔ12 mutation inhibits the interaction with the InsP3RI. However, on the basis of in vitro and in vivo aggregation experiments and on calcium measurements there are no indications that mutant IRAGΔ12 results in enhanced IRAG function. Furthermore, the IRAG mutation does not alter cGKIβ function per se, because cGKIβ still interacts with the mutant IRAG and is still active (see Figure S1). However, although our experiments suggest that the functional effect of the deletion mutant results from the defective inhibition of intracellular calcium rise by NO/cGMP in platelets, unknown alternative effects of this deletion mutation cannot be totally excluded.
Other potential cGKI substrates expressed in platelets, including the Rap1-activating GTPase Rap1-GAP2, HSP27, and VASP,5,25,26 did not copurify with cGKI and more importantly did not compensate for the loss of IRAG-dependent signaling. The NO/cGMP-mediated inhibition of platelet aggregation ex vivo and fibrinogen receptor activation was not completely suppressed by the IRAG mutation. Therefore, other cGKI substrates might be involved in different cGKI-signaling pathways which play a minor role in the inhibition of platelet aggregation. Most likely, these additional substrates do not include VASP as suggested by results obtained with an inactivated VASP gene.27,28
NO attenuated thrombin-induced aggregation of wild-type platelets by greater than 70%, whereas thrombin-induced integrin αIIbβ3 activation was reduced by only 26%. This indicates a nonlinear correlation between (1) inhibition of platelet integrin activation (as determined by flow cytometry) and (2) attenuation of platelet aggregation.
Furthermore, IRAG is obviously involved in the NO-dependent prevention of arterial thrombus formation at sites of vascular lesion but does not alter the basal platelet aggregation at the injured artery. Interestingly, inactivation of the cGKI gene increased platelet adherence to the endothelium after ischemia/reperfusion,7 supporting the notion that cGKI may signal through different substrates in platelets as already shown for the situation in smooth muscle.4 The physiologic significance of these additional pathways needs to be established.
IRAG is linked to the InsP3RI in platelets through its coiled-coil domain and is phosphorylated by cGKI at Ser677. Phosphorylation of the Ser677 homologue of human IRAG is responsible for cGKI-induced inhibition of InsP3-stimulated Ca2+ release.12 In IRAG mutant platelets with a defective IRAG-InsP3RI interaction, the NO/cGMP-mediated suppression of intracellular calcium transients was abolished. The present study, therefore, provides the first evidence that modulation of Cai2+ level through NO/cGMP in platelets involves IRAG-InsP3RI signaling. Furthermore, the results support the notion that NO acting through cGMP/cGKI prevented agonist-induced increases of platelet calcium,9 a crucial step in the process of platelet activation.6 The inhibitory function of cGMP on platelet activation was challenged by observations that cGMP might induce a biphasic response of platelets first promoting and later inhibiting platelet aggregation.29 The results of this and other studies30 have been questioned by others.19,31 It is not clear why different groups arrived at contradictory results. The result of this study clearly identifies a possible alternative (ie, the difference in cGMP level that led to phosphorylation of different cGKI targets such as IRAG, VASP, or thromboxane receptor Iα).32 The lack of VASP in the human complex purified by a cGK-specific column supports the notion that phosphorylation of this target might require high concentrations of active cGKI, whereas IRAG could be phosphorylated already at intermediate concentrations of active cGKI.
cGMP-independent mechanisms, including nitrosylation of proteins, activation of ADP-ribosyltransferases, or transactivation of cAMP-dependent protein kinase, were reported to be induced by some NO donors at high concentrations.33-35 Several different NO donors and a cGMP analog, which is established in platelets,7,19 were used in this study to exclude the possibility that cGMP-independent effects of the NO donor or the cGMP analog were responsible for the phosphorylation of IRAG and the deficient NO/cGMP-mediated inhibition of the IRAG mutant platelet function.
In our experiments, the cGK-inhibitor Rp-8-Br-PET-cGMPS does not affect platelet aggregation without exogenous cGMP or NO. However, other groups reported that Rp-8-Br-PET-cGMPS inhibited platelet aggregation in the absence of NO/cGMP-elevating compounds.31,36 It might be that the divergence from our results is based on different platelet reactivity and experimental conditions. Furthermore, it cannot be excluded that Rp-8-Br-PET-cGMPS affected signaling mechanisms independent of cGMP kinase because Marshall et al31 showed an effect of cGMP analogs in the absence of cGKI.
Importantly, we report here that IRAG is dispensable for the inhibition of aggregation through prostacyclin/cAMP which is an important cascade-impeding platelet function.5 Although cAMP-dependent phosphorylation of the InsP3R has been reported,8,37,38 evidence suggests that cAMP-dependent phosphorylation of the InsP3RI may increase the release of Ca2+.39 Therefore, the cascade through which cAMP kinase inhibits platelet activation and aggregation remains to be established.
In conclusion, the present study shows that NO/cGMP acting through IRAG prevents arterial thrombus formation and thereby arterial thrombosis, the major cause of morbidity and mortality in industrialized countries.
The online version of this article contains a data supplement.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisment” in accordance with 18 USC section 1734.
Conflict-of-interest disclosure: the authors declare no competing financial interests.
Contribution: M.A., M.-L.v.B., C.E., I.K., F.H., S.M., and J.S. designed and/or performed research and analyzed data; M.W. was involved in generating the mouse strain; T.K. and M.W. performed the mass spectrometric analysis; and J.S., S.M., and F.H. wrote the paper.
We thank M. Miller, C. Wolf, and S. Kerstan for their excellent technical work. L. Kunz, W. Siess, C. Traidl, and M. Wechsel are acknowledged for their kind support in the experiments.
This work was supported by grants from the Deutsche Forschungsgemeinschaft, Graduate Program 438, Wilhelm Sander-Stiftung, and Fonds der Chemischen Industrie.

![Figure 1. cGKI macrocomplex and IRAG phosphorylation in human platelets. (A) Identification of IRAG and cGKIβ in human platelets (P-M indicates platelet membranes; P-C, platelet cytosol) by immunoblot analysis with specific antibodies directed against IRAG, cGKIα, or cGKIβ. (B) Isolation and phosphorylation of the ternary complex of IRAG, cGKI, and InsP3RI in human platelets. The complex was isolated using cGMP agarose beads and then phosphorylated by the addition of 8-pCPT-cGMP (3 μM) and [γ-32P]ATP. 32P-phosphorylation was analyzed by autoradiography (AR), and immunoblot analysis (IB) was performed with specific antibodies. The positions of molecular weight markers are indicated. Note that the cGKI substrate VASP was not assembled in the cGKI complex. (C) 33P-phosphorylation of IRAG in intact human platelets stimulated with the cGMP analog 8-pCPT-cGMP (100 μM) for 1 to 30 minutes. (D) Stimulation of human platelets with the nitric oxide donor GEA-NO (100 μM). As control, in each experiment the phosphorylation of IRAG was compared with that of Ser239-VASP, determined by immunoblot analysis with pSer239-VASP–specific antibodies. Equal amounts of total IRAG or VASP in the different lanes were checked by immunoblotting with IRAG- and VASP-specific antibodies (C-D). (E) Statistics of phosphorylation with 8-pCPT-cGMP.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/109/2/10.1182_blood-2005-10-026294/4/m_zh80020706690001.jpeg?Expires=1769106135&Signature=Q0hrm-uFaXuMrps5S-emV8phq4Lftqx5IvgVi~zr1hr6lts5~meut6Q99hQU2~qLWfyUxlJQ3R1sP~vhhY2-tw~YCHUnP5wEJIJyCDjHUuzCqhJJoMYpmgiYoPQB1fYMse7k3jR19cd7RO8X8xPM81IP6pknC5CeihTiQ3en6IncCHZ9xSnhpFLTlI0F0Jdk-62c9OFFqFsoYe~O4rL7bEIcIR8AGxSaT45SC7Ro~ZAYeanScmW9fEfRkdY0kXzBxn6EtU0VeCi3ACjycP9OH7lugrbpCZ~l0tIVn6CSUhVfRr6bsjru8Z83fLtxZOu1PTWT49jeCSTgszknMLFzPw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal