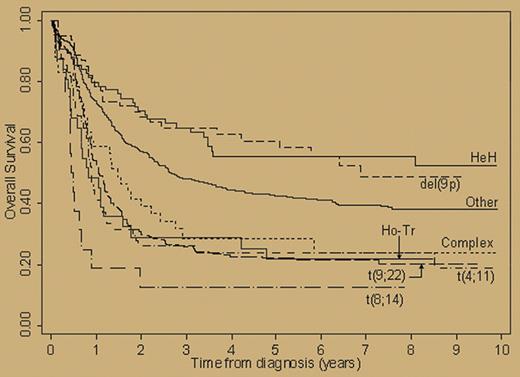
In this issue, Moorman and colleagues demonstrate that acute lymphoblastic leukemia (ALL) with del(9q) or high hyperdiploidy has a relatively favorable outcome, while disease with the Ph chromosome, t(4;11), t(8;14), low hypodiploidy/near triploidy, or complex karyotype carries a poor prognosis (see figure).
Overall survival by cytogenetic subgroup of patients registered on MRC UKALLXII/ECOG 2993. See the complete figure in the article beginning on page 3189.
Overall survival by cytogenetic subgroup of patients registered on MRC UKALLXII/ECOG 2993. See the complete figure in the article beginning on page 3189.
Cytogenetics is the most powerful single prognostic factor in acute myeloid leukemia (AML), and virtually all clinical trials of de novo AML rely on cytogenetics at least for stratification and often for treatment assignment. Except for defining Ph-positive ALL as a separate entity, the application of cytogenetics to the clinical study of ALL has lagged behind its use in AML, largely because of the rarity of ALL and each specific cytogenetic subgroup. Indeed, the Medical Research Council (MRC)/Eastern Cooperative Oncology Group (ECOG) clinical trial from which the data of this report were derived took more than 10 years to complete and required 1522 patients to have sufficient power to distinguish these separate cytogenetic risk categories. Previous reports of the impact of karyotype on outcome of adult ALL provided some insights, but also reported a number of inconsistencies, particularly in rarer subgroups.1-3 While few of the findings of the current study are truly novel, the study has the advantage of size (it is the largest study conducted to date) and its use of mostly contemporary treatments.
The study strengthens the view that ALL associated with high hyperdiploidy and del(9q) carries a favorable prognosis.1,3 These 2 categories of disease, which represent 10% and 9% of non-Ph+ cases, respectively, occur in younger patients and based on some, but not all previous reports, appear to be associated with a decreased probability of relapse. The increased risk associated with Ph positivity and t(8;14) may change with newer therapeutic approaches. Current trials using tyrosine kinase inhibitors for Ph+ disease and lymphoma-like approaches including rituximab for mature B-cell ALL appear to be yielding results superior to those achieved in the standard chemotherapy arm of this trial. The negative impact reported here with t(4;11), seen in 7% of non-Ph+ patients, is entirely consistent with previous reports. The low hypodiploidy/near triploidy category is a recently recognized entity in which the 2 ploidy groups lose or gain the same chromosomes, suggesting that they are 2 manifestations of the same disease. The current study supports the poor prognosis originally reported for this category of patients.4 The poor outcome seen with complex karyotypes is a novel observation and mirrors the association seen in AML.
A major clinical question addressed in the MRC/ECOG trial was the comparative outcome of allogeneic hematopoietic cell transplantation from a matched sibling versus that seen with chemotherapy for adult ALL in first remission. The results, which were presented at the plenary session of this year's American Society of Hematology meeting, demonstrate a statistically significant survival advantage associated with allogeneic transplantation.5 Whether patients with high-risk cytogenetics disproportionately benefit from transplantation is of clinical interest. If so, then matched unrelated donor transplantation during first remission would be worthy of study in this population. Unfortunately, according to the authors, there were too few patients in the high-risk cytogenetic subgroups to answer this question. As the authors suggest, a meta-analysis addressing this issue is sorely needed.
The author declares no competing financial interests. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal