Abstract
Cladribine (2-chlorodeoxyadenosine, 2-CdA) treatment-associated infections may shorten potentially long-term survival in hairy cell leukemia (HCL). In search of the optimal mode of 2-CdA administration, 132 patients with untreated HCL were randomized to receive either standard 5-day 2-CdA protocol or a novel schedule of 6 weekly 2-CdA infusions suggested to be less toxic. Analysis of treatment response confirmed similar complete remission rates, overall response rates, progression-free survival, and overall survival in both 2-CdA protocols. However, we did not observe lower toxicity in the weekly schedule. Of special interest, no significant differences were found in the rate of grade 3/4 infections (18% for daily and 26% for weekly protocol, difference −8.2%; 95% confidence interval [CI] −23.2% to 6.9%; P = .28) and the rate of septic deaths (3% for daily and 2% for weekly protocol, difference 1.4%; 95% CI −4.3% to 7.0%; P = .64). In conclusion, HCL treatment with weekly 2-CdA infusions is equally effective but no safer than the standard 5-day 2-CdA protocol.
Introduction
Cladribine (2-chlorodeoxyadenosine, 2-CdA) belongs to standard therapeutic options for hairy cell leukemia (HCL). In chemotherapy-naive HCL, one course of 2-CdA induces complete response (CR) and long-term survival in the vast majority of patients.1–5 Given this considerable clinical efficacy, the major challenge regarding 2-CdA therapy is reduction of side effects, especially severe infections that may lead to septic death. Lauria et al6 suggested that a novel schedule based on 6 weekly 2-hour 2-CdA infusions could be as effective as the standard 7-day and 5-day protocols but associated with less neutropenia and fewer life-threatening infections. To test the potential clinical benefit of the weekly schedule, in 1998 the Polish Adult Leukemia Group (PALG) initiated a prospective multicenter, randomized comparison with 5-day 2-CdA infusion that is the standard treatment of active HCL in Poland
Patients, materials, and methods
The study was carried out at 14 hematology centers, with central randomization and data management performed in the Department of Hematology at the Medical University of Lodz. The study was approved by the ethics committee of the Medical University of Lodz, and all patients gave informed consent in accordance with the Declaration of Helsinki.
Eligibility criteria
Patients with untreated, active HCL, World Health Organization (WHO) scale performance status better than grade 4, normal liver and renal function, without secondary neoplasm, and age 18 years or older were considered eligible. The diagnosis of HCL and the criteria of activity of disease were defined as previously reported.7
Treatment
Patients were randomly assigned to one of the following 2-CdA schedules: 2-CdA at 0.12 mg/kg in 2-hour intravenous infusion for 5 days (further referred to as the daily schedule); or 2-CdA at 0.12 mg/kg in 2-hour intravenous infusion once a week for 6 weeks (further referred to as the weekly schedule). In patients who achieved CR after the first cycle, treatment was stopped. In patients with partial response (PR), treatment could be continued until maximal response or stopped according to the decision of the treating physician, and in the case of no response (NR) or progression of the disease the treatment was changed. No antibiotic or hematopoietic growth factor prophylaxis was given.
Study end points
The study objective was to verify the hypothesis that the 2-CdA weekly schedule has similar efficacy but lower early toxicity than the daily schedule. The primary end points were CR at 3 months after completion of the 2-CdA therapy and treatment-related grade 3/4 infections during 4 months from the start of 2-CdA. The secondary end points included overall response rate (ORR), progression-free survival (PFS), overall survival (OS), and other grade 3/4 side effects. Criteria for response were defined according to Grever et al8 and National Cancer Institute (NCI) guidelines,9 and toxicity according to WHO criteria.10 Deaths that occurred during 4 months from the start of 2-CdA were defined as early deaths (EDs).
Statistical analysis
Calculation of sample size was based on previous reports indicating that an identical CR rate of 75%, but different major infection rates of 289% and of 8% may be expected with the daily and weekly 2-CdA schedules, respectively.5,11 Fifty-four patients were required to be assigned to each treatment arm to detect a decrease of 25% from a 75% CR rate, with error levels of α = 0.05 and β = 0.2 for a 2-sided test. Taking into account possible drop-outs, accrual was increased by 20%, resulting in a requirement of 65 patients per arm. Treatment groups were compared using the Mann-Whitney test for continuous data, and the Chi-squared test for categorical data. Difference between proportions, and associated confidence intervals, were calculated by standard methods. OS was defined as time from randomization to death, and PFS was defined as time from randomization to progression or death. PFS and OS curves were plotted using the Kaplan-Meier method and probabilities of PFS and OS were compared by the log-rank test.12,13 P < .05 was considered statistically significant.
Results and discussion
Between January 1, 1998, and September 31, 2005, 132 patients with untreated, active HCL from 14 centers were randomized to receive either the daily (68 patients) or weekly (64 patients) 2-CdA protocol. Sixteen patients were excluded from analysis due to misdiagnosis (4 patients), not meeting eligibility criteria (6 patients), withdrawal of consent (3 patients), and dropping out before beginning the treatment (2 patients). Baseline characteristics of 116 patients assessed for response, toxicity, and survival are shown in Table 1.
Comparison of baseline characteristics and grade 3/4 treatment-related side effects in patients randomized to daily and weekly schedules of 2-CdA administration 2-CdA indicates 2-chlorodeoxyadenosine
| Parameter . | 2-CdA daily, n = 62 . | 2-CdA weekly, n = 54 . | P . |
|---|---|---|---|
| Patient characteristics | |||
| Median age, y (range) | 53 (27-78) | 57 (25-86) | .33 |
| Male, no. (%) | 41 (66) | 37 (68) | .74 |
| Median time from diagnosis, mo (range) | 0.4 (0-37.8) | 0.1 (0-13.4) | .21 |
| Median white cell count, × G/L (range) | 2.2 (0.7-30.0) | 2.8 (0.7-34.0) | .09 |
| Median absolute neutrophil count, × G/L (range) | 0.42 (0.0-4.5) | 0.66 (0.1-2.0) | .48 |
| Median hemoglobin level, g/L (range) | 9.9 (3.7-15.2) | 10.8 (4.3-16.4) | .42 |
| Median platelet count, × G/L (range) | 66 (1-301) | 86 (2-238) | .02 |
| Lymphadenopathy, no. (%) | 8 (13) | 8 (15) | .76 |
| Splenomegaly, no. (%) | 38 (63) | 31 (57) | .68 |
| Hepatomegaly, no. (%) | 5 (8) | 12 (22) | .03 |
| Treatment side effects | |||
| Progression of neutropenia, no. (%) | 29 (47) | 25 (47) | .97 |
| Neutropenia below 0.5 G/L, no. (%) | 36 (58) | 28 (52) | .27 |
| Neutropenia below 1.0 G/L, no. (%) | 38 (61) | 28 (52) | .20 |
| Progression of thrombocytopenia, no. (%) | 10 (16) | 9 (17) | .93 |
| Platelet transfusions, U | 47 | 39 | .21 |
| Progression of anemia, no. (%) | 9 (15) | 10 (19) | .58 |
| Red cell transfusions, U | 47 | 40 | .82 |
| All infections, including fever of unknown origin, no. (%) | 11 (18) | 14 (26) | .28 |
| Pneumonia, no. (%) | 5 (8) | 4 (7) | .87 |
| Urinary tract infections, no. (%) | 1 (2) | 2 (4) | .49 |
| Other infections, no. (%) | 3 (5) | 5 (9) | .37 |
| Fever of unknown origin, no. (%) | 2 (3) | 5 (9) | .18 |
| Time to infection, d (range) | 6 (1-14) | 11 (3-28) | .09 |
| Duration of infection, d (range) | 5 (1-60) | 13 (3-28) | .27 |
| Septic deaths, no. (%) | 2 (3) | 1 (2) | .64 |
| Allergic symptoms, no. (%) | 1 (2) | 2 (4) | .49 |
| Second malignancies, no. (%) | 4 (6) | 3 (6) | .50 |
| Parameter . | 2-CdA daily, n = 62 . | 2-CdA weekly, n = 54 . | P . |
|---|---|---|---|
| Patient characteristics | |||
| Median age, y (range) | 53 (27-78) | 57 (25-86) | .33 |
| Male, no. (%) | 41 (66) | 37 (68) | .74 |
| Median time from diagnosis, mo (range) | 0.4 (0-37.8) | 0.1 (0-13.4) | .21 |
| Median white cell count, × G/L (range) | 2.2 (0.7-30.0) | 2.8 (0.7-34.0) | .09 |
| Median absolute neutrophil count, × G/L (range) | 0.42 (0.0-4.5) | 0.66 (0.1-2.0) | .48 |
| Median hemoglobin level, g/L (range) | 9.9 (3.7-15.2) | 10.8 (4.3-16.4) | .42 |
| Median platelet count, × G/L (range) | 66 (1-301) | 86 (2-238) | .02 |
| Lymphadenopathy, no. (%) | 8 (13) | 8 (15) | .76 |
| Splenomegaly, no. (%) | 38 (63) | 31 (57) | .68 |
| Hepatomegaly, no. (%) | 5 (8) | 12 (22) | .03 |
| Treatment side effects | |||
| Progression of neutropenia, no. (%) | 29 (47) | 25 (47) | .97 |
| Neutropenia below 0.5 G/L, no. (%) | 36 (58) | 28 (52) | .27 |
| Neutropenia below 1.0 G/L, no. (%) | 38 (61) | 28 (52) | .20 |
| Progression of thrombocytopenia, no. (%) | 10 (16) | 9 (17) | .93 |
| Platelet transfusions, U | 47 | 39 | .21 |
| Progression of anemia, no. (%) | 9 (15) | 10 (19) | .58 |
| Red cell transfusions, U | 47 | 40 | .82 |
| All infections, including fever of unknown origin, no. (%) | 11 (18) | 14 (26) | .28 |
| Pneumonia, no. (%) | 5 (8) | 4 (7) | .87 |
| Urinary tract infections, no. (%) | 1 (2) | 2 (4) | .49 |
| Other infections, no. (%) | 3 (5) | 5 (9) | .37 |
| Fever of unknown origin, no. (%) | 2 (3) | 5 (9) | .18 |
| Time to infection, d (range) | 6 (1-14) | 11 (3-28) | .09 |
| Duration of infection, d (range) | 5 (1-60) | 13 (3-28) | .27 |
| Septic deaths, no. (%) | 2 (3) | 1 (2) | .64 |
| Allergic symptoms, no. (%) | 1 (2) | 2 (4) | .49 |
| Second malignancies, no. (%) | 4 (6) | 3 (6) | .50 |
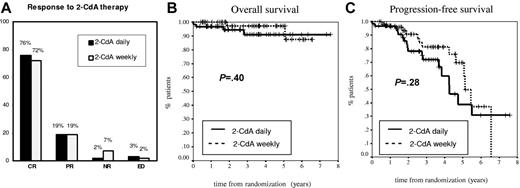
We found that response to chemotherapy was comparable in both treatment arms (Figure 1A). The response was assessed after a similar total number of administered treatment courses in both cohorts, with 97 (84%) patients who received only one 2-CdA course. In the group of daily 2-CdA, there were 47 (76%) patients with CR, 12 (19%) patients with PR, 1 patient (2%) with NR, and 2 EDs, compared with 39 patients (72%) with CR, 10 patients (19%) with PR, 4 patients (7%) with NR, and 1 ED (2%) in the weekly schedule. Therefore, daily and weekly protocols gave similar high CR rates (P = .86) and ORRs (95% vs 91%, P = .41). Moreover, survival analysis did not produce significant differences between the 2-CdA protocols (Figure 1B-C). The estimated 6.5-year OS rates were 91% and 88% (P = .40) and median PFS rates were 4.3 years (95% CI 3.3-5.2 years) and 5.1 years (95% CI 4.7-5.6 years) (P = .28) for the daily and weekly schedules, respectively. Our findings on equivalent efficacy of these 2-CdA schedules are in accordance with retrospective nonrandomized comparison on 37 patients for whom data were previously published.14 Pentostatin (deoxycoformycin; DCF), another purine nucleoside analog used in the treatment of HCL, seems to have similar efficacy and toxicity as 2-CdA, although direct randomized comparison of the 2 agents has not yet been performed.8,15,16
Comparison of clinical activities of 2 schedules of 2-CdA administration in newly diagnosed patients with hairy cell leukemia tested in the study. (A) Response to 2-CdA therapy. (B) Overall survival analysis. (C) Progression-free survival analysis.
Comparison of clinical activities of 2 schedules of 2-CdA administration in newly diagnosed patients with hairy cell leukemia tested in the study. (A) Response to 2-CdA therapy. (B) Overall survival analysis. (C) Progression-free survival analysis.
In contrast to previous suggestions,6,11,14 our work did not confirm reduced toxicity of the weekly 2-CdA schedule. A total of 25 grade 3/4 infections were observed in 24 patients including one subject treated with the weekly protocol who developed 2 separate infectious episodes (acute bronchitis and fever of unknown origin [FUO]). Most importantly, the prevalence of grade 3/4 infections did not differ regarding treatment arm (18% for daily and 26% for weekly 2-CdA protocol, difference −8.2%; 95% CI −23.2% to 6.9%; P = .28; Table 1). The time to the infection onset and the time of infection duration were comparable in the 2 schedules (Table 1). Also, the rates of major types of grade 3/4 infections were similar in both protocols (Table 1). Moreover, daily and weekly 2-CdA schedules gave comparable prevalence of severe infections even if analyses were restricted to patients with pretreatment neutropenia below 1.0 G/L (17% vs 26%, difference −9.8%; 95% CI −24.6% to 5.0%; P = .32) and below 0.5 G/L (21% vs 26%, difference −5.0%; 95% CI 20.4% to 10.5%; P = .56). This similar risk of severe infections is in line with identical rates of progression of neutropenia on treatment (47% for both treatment arms, difference 0.48%; 95% CI −17.7% to 18.7%; P = .97) and comparable rates of neutropenia below 0.5 G/L and 1.0 G/L (Table 1). The comparison of other grade 3/4 side effects following 2-CdA therapy, including thrombocytopenia and anemia, as well as transfusion requirements, did not show significant differences (Table 1).
Secondary neoplasia is a major complication that can be related to both the biology of HCL and immunosupression caused by chemotherapy. In this study, 7 second cancers were diagnosed, including acute myeloid leukemia (AML), renal cell cancer, ovarian cancer, and skin carcinoma basocellullare in the daily 2-CdA schedule, and breast cancer, prostate cancer, and unknown primary adenocarcinoma in the weekly schedule. The median time to the diagnosis of the second cancer reached 2.3 years (range 0.2-4.2 years).
Special attention was paid to the analysis of causes of mortality in the study. A total of 6 deaths were recorded during the follow-up period, including 4 deaths in the daily and 2 in the weekly 2-CdA protocol groups. Three deaths were classified as EDs, including 2 (3%) in the daily and 1 (2%) in weekly 2-CdA schedule, difference 1.4% (95% CI −4.3% to 7.0%; P = .64). The cause of all EDs was infectious complications (pneumonia in 1 patient and sepsis in 2 other patients). The time from the first day of 2-CdA treatment to death was 3, 31, and 60 days. All 3 patients had neutropenia below 0.25 G/L during infection onset, which did not improve to the last blood count analysis. Systematic blood cultures revealed infection with Hafnia alvei in 1 patient, and were negative in the other 2 patients. Among 3 deaths that occurred late in observation, 2 were related to infections during HCL progression and 1 to secondary AML. Therefore, our study confirms that septic deaths are a major cause of early mortality in HCL treated with 2-CdA, although decrease in therapy density does not seem to solve this problem. However, it should be noted that the total dose of 2-CdA was higher in the weekly than in the daily schedule (6 vs 5 infusions), which could influence the observed results.
In conclusion, the results of our randomized trial indicate that weekly 2-CdA infusions for 6 weeks used in the treatment of active HCL are equally effective, but not less toxic than the standard 5-day 2-CdA protocol. Further studies in search of strategies to decrease the risk of life-threatening infections complicating the treatment of HCL with 2-CdA are required.
Authorship
Contribution: T.R. designed and supervised the trial and wrote the report; K.J. performed statistical analysis and wrote the report;J.G.-T. was monitored the trial, managed the data at the coordinating center, and wrote the report; J.Z.B., M.K., J.D.-T., E.W., A.Z., J.D., A.D., M.W., B.Z., M.C., A.K., A.H., K.L., B.S.-H., K.S., K.G., A.B.S., W.N., K.Z., L.M.-P., J.K., J.S., K.W., I.S., L.K., and B.C. were responsible for patients' accrual and monitoring, and management of the clinical data at their referring centers. A complete list of the members of the Polish Adult Leukemia Group appears as a data supplement to the online version of this article.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Tadeusz Robak, Department of Hematology, Medical University of Lodz, 93-513 Lodz, Pabianicka 62, Poland; e-mail: robaktad@csk.umed.lodz.pl.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Dr Richard Szydlo (Imperial College and Hammersmith Hospital, London, United Kingdom) for statistical advice.
This work was supported by a grant from the Ministry of Science (no. 2P05B01828).

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal