We compared the treatment-related mortality, relapse rate, disease-free survival (DFS), and overall survival (OS) by cytogenetic risk group of 261 patients with acute myeloid leukemia in first complete remission (CR1) and 299 patients in CR2 in undergoing matched unrelated donor hematopoietic stem cell transplantation (HSCT). For patients in first CR, the DFS and OS at 5 years were similar for the favorable, intermediate, and unfavorable risk groups at 29% (95% confidence interval [CI], 8%-56%) and 30% (22%-38%); 27% (19%-39%) and 29% (8%-56%); and 30% (95% CI, 22%-38%) and 30% (95% CI, 20%-41%), respectively. For patients in second CR, the DFS and OS at 5 years were 42% (95% CI, 33%-52%) and 35% (95% CI, 28%-43%); 38% (95% CI, 23%-54%) and 45% (95% CI, 35%-55%); and 37% (95% CI, 30%-45%) and 36% (95% CI, 21%-53%), respectively. Cytogenetics had little influence on the overall outcome for patients in first CR. In second CR, outcome was modestly, but not significantly, better for patients with favorable cytogenetics. The graft-versus-leukemia effect appeared effective, even in patients with unfavorable cytogenetics. However, treatment-related mortality was high. Matched unrelated donor HSCT should be considered for all patients with unfavorable cytogenetics who lack a suitable HLA-matched sibling donor.
Introduction
Matched unrelated donor (MUD) hematopoietic stem cell transplantation (HSCT) is a potentially curative treatment for patients with acute myeloid leukemia (AML).1,,,–5 The outcome appears more favorable if such treatment is carried out in first complete remission (CR1) compared with more advanced phases of the disease.4,6,7 The graft-versus-leukemia (GVL) effect induced may be sufficient to overcome the otherwise poor prognosis often associated with AML. The GVL generated in the setting of HLA-matched sibling donor HSCT has been shown to be potent enough to cure some patients with unfavorable cytogenetics, a group with a particularly poor prognosis, in some, but not all, reports.8,9 Theoretically, the GVL associated with MUD HSCT should be more potent than that associated with HLA-matched sibling HSCT. However, the efficacy of this strategy for patients with unfavorable cytogenetics, the most important prognostic factor in AML,10,11 is uncertain. To test this hypothesis, we analyzed data on the outcome by cytogenetic risk group in patients with AML in CR1, and second complete remission (CR2) undergoing MUD HSCT facilitated by the National Marrow Donor Program (NMDP) and reported to the Center for International Blood and Marrow Transplant Research (CIBMTR).
Materials and methods
Data sources
The NMDP provides unrelated donor marrow to facilitate transplants throughout the world and maintains a longitudinal outcomes database on the transplantations it facilitates. A formal affiliation of the research division of the NMDP, the International Bone Marrow Transplant Registry, and the Autologous Blood and Marrow Transplant Registry led to the establishment of the CIBMTR in 2004. The CIBMTR is a working group of more than 500 transplant centers worldwide that voluntarily contribute data on allogeneic and autologous transplant recipients to a Statistical Center at the Medical College of Wisconsin or the NMDP Coordinating Center in Minneapolis. Participating centers register and provide basic information on all consecutive transplantations; compliance is monitored by on-site audits. Detailed demographic, disease and transplant characteristics, and outcome data are collected on a sample of registered patients including all unrelated donor transplantations facilitated by the NMDP in the United States. Patients are followed longitudinally, with yearly follow-up. Computerized error checks, physician review of submitted data, and on-site audits of participating centers ensure data quality. Observational studies conducted by the CIBMTR are done so with a waiver of informed consent and in compliance with HIPAA regulations as determined by the institutional review board and the Privacy Officer of the Medical College of Wisconsin.
Patients
This study included patients with AML in either CR1 or CR2, defined using previously published criteria, undergoing MUD HSCT between 1988 to 2002. All patients received stem cells derived from bone marrow. Five hundred sixty patients met the on-study criteria: 13 patients were classified as favorable risk in CR1, 164 patients as intermediate risk in CR1, and 84 patients as unfavorable risk in CR1. Among the 299 patients in CR2, 97 patients were classified as favorable risk, 165 patients as intermediate risk, and 37 patients were classified as unfavorable risk. Eligible cases came from 96 reporting centers. Median follow-up of survivors among the patients with favorable, intermediate, and unfavorable cytogenetics in CR1 was 61 (range, 24-121) months, 49 (range, 7-144) months, and 54 (range, 6-112) months, respectively. The median follow-up for patients with favorable, intermediate, and unfavorable cytogenetics was 60 (range, 6-155) months, 60 (range, 6-112) months, and 52 (range, 30-133) months, respectively.
Cytogenetics
Based on results of conventional chromosome studies of bone marrow or blood provided by various chromosome laboratories, each patient was assigned to a cytogenetic risk group (favorable, intermediate, or unfavorable), by a cytogeneticist (G.D.). The SWOG/ECOG classification of cytogenetic risk8 was used to classify patients by their cytogenetics. Favorable risk was defined as follows: inv(16)/t(16;16)/del(16q) with or without other chromosome anomalies and t(8;21) without either del(9q) or part of a complex karyotype. Intermediate risk was defined as follows: +8, −Y, +6, del(12p), and normal karyotype. Unfavorable risk was defined as follows: −5/del(5q), −7/del(7q), inv(3q)/t(3,3), abnormal 11q, 20q, or 21q, del(9q), t(6;9), t(9;22), abnormal 17p, and complex karyotype defined as 3 or more anomalies. Unknown risk was defined as follows: all other clonal anomalies with less than 3 anomalies.
End points
Primary end points were transplantation-related mortality (TRM), relapse, disease-free survival (DFS), and overall survival (OS). Treatment-related mortality was defined as death during continuous CR. Relapse was defined as clinical or hematologic recurrence. For analyses of DFS, failures were clinical or hematologic relapses or deaths from any cause; patients alive and in CR were censored at the time of last follow-up. For analyses of OS, failure was death from any cause; surviving patients were censored at the date of last contact.
Statistical analyses
Patient-, disease-, and transplant-related variables for the patient cohorts were described by cytogenetic risk groups. Probabilities of TRM and relapse were calculated using cumulative incidence curves to accommodate competing risks. Univariate probabilities of DFS and OS were calculated using the Kaplan-Meier estimator.12 Estimates of standard error for the survival function were calculated by Greenwood formula and 95% confidence intervals (CIs) were constructed using log-transformed intervals. Multivariate models were built using a stepwise forward selection technique, using a P value of .05 or less as the criterion for inclusion in the final model, separately for patients in CR1 and CR2. The primary objective was to compare outcomes according to cytogenetic risk; this variable was included in all models, except that good-risk patients in CR1 were dropped from the multivariate models because of small sample sizes. The following variables were considered: age at transplantation (≤ 18 y vs 19-35 y vs > 35 y), recipient cytomegalovirus (CMV) status (negative vs positive), Karnofsky performance score (≥ 90 vs > 90), year of transplantation (1988–1995 vs 1996–1999 vs 2000–2002), donor-recipient HLA match (match vs mismatch), sex match (F-F vs F-M vs M-F vs M-M), donor-recipient CMV match (+/+ vs +/− vs −/+ vs −/−), conditioning regimen (cyclophosphamide + total body irradiation [Cy + TBI] ± other vs busulfan [Bu] + Cy ± other vs other), GVHD prophylaxis (CSA + MTX ± other vs FK506 ± other vs T-cell depletion), cell dose (≤ 3 × 108/kg vs > 3 × 108/kg vs missing), time from diagnosis to transplantation (CR1 only: ≤ 6 months vs > 6 months), and duration of CR1 (CR2 only: ≤ 12 months vs > 12 months). All possible risk factors were checked for proportional hazards using a time-dependent covariate approach. Factors found to have nonproportional hazards were adjusted for in subsequent analyses using time-dependent effects. There were no significant interactions between cytogenetic risk and any other variables. All P values are 2-sided. Analyses were completed with the use of PROC PHREG in SAS software, version 9.1 (SAS Institute, Cary, NC).
Results
Patients in CR1
The median age for patients in CR1 with favorable, intermediate, and unfavorable cytogenetics was 24 (range, 2-45) years, 30 (range, 1-58) years, and 32 (range, 1-60) years, respectively (Table 1). Patients with unfavorable cytogenetics were more often CMV seropositive (58%) compared with patients with either favorable (38%) or intermediate (51%) cytogenetics. Among patients with unfavorable cytogenetics, there were fewer CMV-seronegative donor-recipient pairs (20%) compared with patients with either favorable (47%) or intermediate (30%) cytogenetics.
Characteristics of patients who underwent unrelated donor transplantation for AML in first complete remission, by cytogenetics risk group
| Variable . | Favorable . | Intermediate . | Unfavorable . |
|---|---|---|---|
| No. of patients | 13 | 164 | 84 |
| Age at transplantation, median (range), y | 24 (2-45) | 30 (1-58) | 32 (1-60) |
| Age at transplantation, no. (%) | |||
| Younger than 20 y | 5 (39) | 54 (33) | 23 (27) |
| 20 to 40 y | 6 (46) | 58 (35) | 34 (41) |
| Older than 40 y | 2 (15) | 52 (32) | 27 (32) |
| Karnofsky performance score at transplantation, no. (%) | |||
| Less than 90 | 2 (15) | 36 (22) | 15 (18) |
| 90 or more | 10 (77) | 126 (77) | 65 (77) |
| Unknown | 1 (8) | 2 (1) | 4 (5) |
| CMV status, no. (%) | |||
| Positive | 5 (38) | 84 (51) | 49 (58) |
| Negative | 8 (62) | 78 (48) | 35 (42) |
| Unknown | 0 | 2 (1) | 0 |
| Conditioning regimen, no. (%) | |||
| BuCy ± other | 3 (23) | 35 (21) | 9 (11) |
| CyTBI ± other | 10 (77) | 122 (75) | 70 (82) |
| Other | 0 | 7 (4) | 5 (7) |
| Time from diagnosis to transplantation, median (range), mo | 5 (3-17) | 6 (2-21) | 6 (1-17) |
| Nucleated cell dose, median (range), × 108/kg | 3 (< 1-6) | 2 (< 1-52) | 3 (< 1-9) |
| Donor-recipient sex match, no. (%) | |||
| Female-female | 3 (23) | 36 (22) | 18 (21) |
| Female-male | 1 (8) | 38 (23) | 16 (19) |
| Male-female | 3 (23) | 38 (23) | 21 (25) |
| Male-male | 6 (46) | 52 (32) | 29 (35) |
| Donor-recipient CMV match, no. (%) | |||
| +/+ | 3 (23) | 28 (17) | 20 (24) |
| +/− | 2 (15) | 27 (16) | 17 (20) |
| −/+ | 2 (15) | 55 (34) | 29 (35) |
| −/− | 6 (47) | 49 (30) | 17 (20) |
| Unknown | 0 | 5 (3) | 1 (1) |
| Donor-recipient HLA match, no. (%) | |||
| Match | 11 (85) | 121 (74) | 68 (81) |
| Mismatch | 2 (15) | 43 (26) | 16 (19) |
| Year of transplantation, no. (%) | |||
| 1988 to 1993 | 1 (8) | 10 (7) | 4 (5) |
| 1994 to 1997 | 4 (31) | 59 (35) | 29 (34) |
| 1998 to 2002 | 8 (61) | 95 (58) | 51 (61) |
| GVHD prophylaxis, no. (%) | |||
| CsA + MTX ± other | 7 (54) | 78 (47) | 44 (53) |
| FK506 ± other | 2 (15) | 24 (15) | 15 (18) |
| T-cell depletion | 4 (31) | 56 (34) | 23 (27) |
| Other | 0 | 6 (4) | 2 (2) |
| Median follow-up of survivors, mo (range) | 61 (24-121) | 49 (7-144) | 54 (6-112) |
| Variable . | Favorable . | Intermediate . | Unfavorable . |
|---|---|---|---|
| No. of patients | 13 | 164 | 84 |
| Age at transplantation, median (range), y | 24 (2-45) | 30 (1-58) | 32 (1-60) |
| Age at transplantation, no. (%) | |||
| Younger than 20 y | 5 (39) | 54 (33) | 23 (27) |
| 20 to 40 y | 6 (46) | 58 (35) | 34 (41) |
| Older than 40 y | 2 (15) | 52 (32) | 27 (32) |
| Karnofsky performance score at transplantation, no. (%) | |||
| Less than 90 | 2 (15) | 36 (22) | 15 (18) |
| 90 or more | 10 (77) | 126 (77) | 65 (77) |
| Unknown | 1 (8) | 2 (1) | 4 (5) |
| CMV status, no. (%) | |||
| Positive | 5 (38) | 84 (51) | 49 (58) |
| Negative | 8 (62) | 78 (48) | 35 (42) |
| Unknown | 0 | 2 (1) | 0 |
| Conditioning regimen, no. (%) | |||
| BuCy ± other | 3 (23) | 35 (21) | 9 (11) |
| CyTBI ± other | 10 (77) | 122 (75) | 70 (82) |
| Other | 0 | 7 (4) | 5 (7) |
| Time from diagnosis to transplantation, median (range), mo | 5 (3-17) | 6 (2-21) | 6 (1-17) |
| Nucleated cell dose, median (range), × 108/kg | 3 (< 1-6) | 2 (< 1-52) | 3 (< 1-9) |
| Donor-recipient sex match, no. (%) | |||
| Female-female | 3 (23) | 36 (22) | 18 (21) |
| Female-male | 1 (8) | 38 (23) | 16 (19) |
| Male-female | 3 (23) | 38 (23) | 21 (25) |
| Male-male | 6 (46) | 52 (32) | 29 (35) |
| Donor-recipient CMV match, no. (%) | |||
| +/+ | 3 (23) | 28 (17) | 20 (24) |
| +/− | 2 (15) | 27 (16) | 17 (20) |
| −/+ | 2 (15) | 55 (34) | 29 (35) |
| −/− | 6 (47) | 49 (30) | 17 (20) |
| Unknown | 0 | 5 (3) | 1 (1) |
| Donor-recipient HLA match, no. (%) | |||
| Match | 11 (85) | 121 (74) | 68 (81) |
| Mismatch | 2 (15) | 43 (26) | 16 (19) |
| Year of transplantation, no. (%) | |||
| 1988 to 1993 | 1 (8) | 10 (7) | 4 (5) |
| 1994 to 1997 | 4 (31) | 59 (35) | 29 (34) |
| 1998 to 2002 | 8 (61) | 95 (58) | 51 (61) |
| GVHD prophylaxis, no. (%) | |||
| CsA + MTX ± other | 7 (54) | 78 (47) | 44 (53) |
| FK506 ± other | 2 (15) | 24 (15) | 15 (18) |
| T-cell depletion | 4 (31) | 56 (34) | 23 (27) |
| Other | 0 | 6 (4) | 2 (2) |
| Median follow-up of survivors, mo (range) | 61 (24-121) | 49 (7-144) | 54 (6-112) |
BU indicates busulfan; CY, cyclophosphamide; TBI, total body irradiation; CMV, cytomegalovirus; HLA, human leukocyte antigen; GVHD, graft-versus-host disease; CsA, cyclosporine; and MTX, methotrexate.
Patients in CR2
The median age among patients in CR2 with favorable, intermediate, and unfavorable cytogenetics was similar, 25 (range, 2-50) years, 26 (range, 1-58) years, and 21 (range, 2-58) years, respectively (Table 2). More patients with favorable cytogenetics were CMV seronegative (60%) compared with those patients with either intermediate (48%) or unfavorable (43%) cytogenetics. More patients with unfavorable cytogenetics had a Karnofsky score more than 90% (32%) compared with patients with either favorable (19%) or intermediate (27%) cytogenetics. The median duration of CR1 for patients with unfavorable cytogenetics was shorter (8 months) than that of patients with either favorable (11 months) or intermediate (10 months) cytogenetics.
Characteristics of patients who underwent unrelated donor transplantation for AML in second complete remission, by cytogenetics risk group
| Variable . | Favorable . | Intermediate . | Unfavorable . |
|---|---|---|---|
| No. of patients | 97 | 165 | 37 |
| Age at transplantation, median (range), y | 25 (2-50) | 25 (1-58) | 21 (2-58) |
| Age at transplantation, no. (%) | |||
| Younger than 20 y | 41 (42) | 65 (39) | 18 (49) |
| 20 to 40 y | 40 (42) | 56 (34) | 10 (27) |
| Older than 40 y | 16 (16) | 44 (27) | 9 (24) |
| Karnofsky score at transplantation, no. (%) | |||
| Less than 90 | 18 (19) | 44 (27) | 12 (32) |
| 90 or more | 77 (79) | 118 (71) | 24 (65) |
| Unknown | 2 (2) | 3 (2) | 1 (3) |
| CMV status, no. (%) | |||
| Positive | 37 (38) | 84 (51) | 20 (54) |
| Negative | 58 (60) | 79 (48) | 16 (43) |
| Unknown | 2 (2) | 2 (1) | 1 (3) |
| Conditioning regimen, no. (%) | |||
| BuCy ± other | 12 (12) | 24 (15) | 7 (19) |
| CyTBI ± other | 79 (82) | 129 (78) | 30 (81) |
| Other | 6 (6) | 12 (7) | 0 |
| Duration of first CR, median (range), mo | 11 (1-38) | 10 (<1-43) | 8 (< 1-28) |
| Nucleated cell dose, median (range), × 108/kg | 2 (<1-11) | 3 (<1-17) | 3 (< 1-21) |
| Donor-recipient sex match, no. (%) | |||
| Female-female | 17 (18) | 29 (17) | 8 (22) |
| Female-male | 17 (18) | 28 (17) | 8 (22) |
| Male-female | 24 (24) | 44 (27) | 10 (27) |
| Male-male | 39 (40) | 64 (39) | 11 (29) |
| Donor-recipient CMV match, no. (%) | |||
| +/+ | 20 (21) | 33 (20) | 10 (27) |
| +/− | 18 (19) | 27 (16) | 4 (11) |
| −/+ | 17 (17) | 51 (31) | 10 (27) |
| −/− | 39 (40) | 52 (32) | 12 (32) |
| Unknown | 3 (3) | 2 (1) | 1 (3) |
| Donor-recipient HLA match, no. (%) | |||
| Match | 74 (76) | 122 (74) | 27 (73) |
| Mismatch | 23 (24) | 43 (26) | 10 (27) |
| Year of transplantation, no. (%) | |||
| 1988 to 1993 | 6 (6) | 14 (8) | 3 (8) |
| 1994 to 1997 | 36 (37) | 58 (35) | 8 (21) |
| 1998 to 2002 | 55 (57) | 93 (57) | 26 (71) |
| GVHD prophylaxis, no. (%) | |||
| CsA + MTX ± other | 41 (42) | 89 (54) | 16 (43) |
| FK506 ± other | 17 (18) | 35 (21) | 5 (13) |
| T-cell depletion | 36 (37) | 37 (22) | 15 (41) |
| Other | 3 (3) | 4 (3) | 1 (3) |
| Median follow-up of survivors, mo (range) | 60 (6-155) | 60 (6-112) | 52 (30-133) |
| Variable . | Favorable . | Intermediate . | Unfavorable . |
|---|---|---|---|
| No. of patients | 97 | 165 | 37 |
| Age at transplantation, median (range), y | 25 (2-50) | 25 (1-58) | 21 (2-58) |
| Age at transplantation, no. (%) | |||
| Younger than 20 y | 41 (42) | 65 (39) | 18 (49) |
| 20 to 40 y | 40 (42) | 56 (34) | 10 (27) |
| Older than 40 y | 16 (16) | 44 (27) | 9 (24) |
| Karnofsky score at transplantation, no. (%) | |||
| Less than 90 | 18 (19) | 44 (27) | 12 (32) |
| 90 or more | 77 (79) | 118 (71) | 24 (65) |
| Unknown | 2 (2) | 3 (2) | 1 (3) |
| CMV status, no. (%) | |||
| Positive | 37 (38) | 84 (51) | 20 (54) |
| Negative | 58 (60) | 79 (48) | 16 (43) |
| Unknown | 2 (2) | 2 (1) | 1 (3) |
| Conditioning regimen, no. (%) | |||
| BuCy ± other | 12 (12) | 24 (15) | 7 (19) |
| CyTBI ± other | 79 (82) | 129 (78) | 30 (81) |
| Other | 6 (6) | 12 (7) | 0 |
| Duration of first CR, median (range), mo | 11 (1-38) | 10 (<1-43) | 8 (< 1-28) |
| Nucleated cell dose, median (range), × 108/kg | 2 (<1-11) | 3 (<1-17) | 3 (< 1-21) |
| Donor-recipient sex match, no. (%) | |||
| Female-female | 17 (18) | 29 (17) | 8 (22) |
| Female-male | 17 (18) | 28 (17) | 8 (22) |
| Male-female | 24 (24) | 44 (27) | 10 (27) |
| Male-male | 39 (40) | 64 (39) | 11 (29) |
| Donor-recipient CMV match, no. (%) | |||
| +/+ | 20 (21) | 33 (20) | 10 (27) |
| +/− | 18 (19) | 27 (16) | 4 (11) |
| −/+ | 17 (17) | 51 (31) | 10 (27) |
| −/− | 39 (40) | 52 (32) | 12 (32) |
| Unknown | 3 (3) | 2 (1) | 1 (3) |
| Donor-recipient HLA match, no. (%) | |||
| Match | 74 (76) | 122 (74) | 27 (73) |
| Mismatch | 23 (24) | 43 (26) | 10 (27) |
| Year of transplantation, no. (%) | |||
| 1988 to 1993 | 6 (6) | 14 (8) | 3 (8) |
| 1994 to 1997 | 36 (37) | 58 (35) | 8 (21) |
| 1998 to 2002 | 55 (57) | 93 (57) | 26 (71) |
| GVHD prophylaxis, no. (%) | |||
| CsA + MTX ± other | 41 (42) | 89 (54) | 16 (43) |
| FK506 ± other | 17 (18) | 35 (21) | 5 (13) |
| T-cell depletion | 36 (37) | 37 (22) | 15 (41) |
| Other | 3 (3) | 4 (3) | 1 (3) |
| Median follow-up of survivors, mo (range) | 60 (6-155) | 60 (6-112) | 52 (30-133) |
BU indicates bulsulfan; CY, cyclophosphamide; TBI, total body irradiation; CMV, cytomegalovirus; HLA, human leukocyte antigen; GVHD, graft-versus-host disease; CsA, cyclosporine; MTX, methotrexate; CR, complete remission; and FK506, tacrolimus.
Univariate analyses
Patients in CR1.
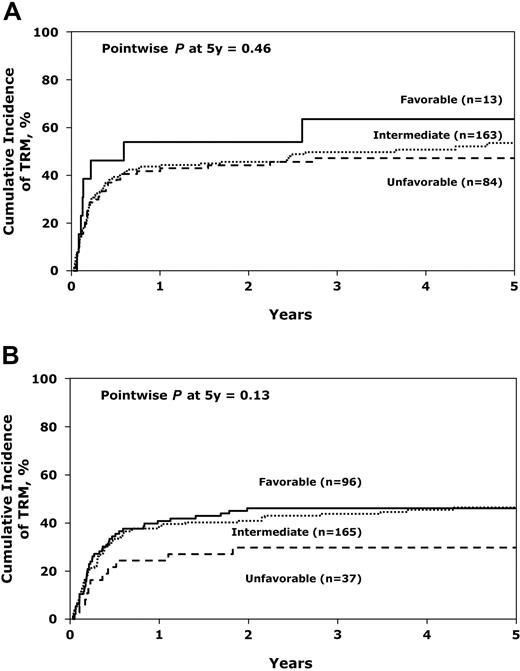
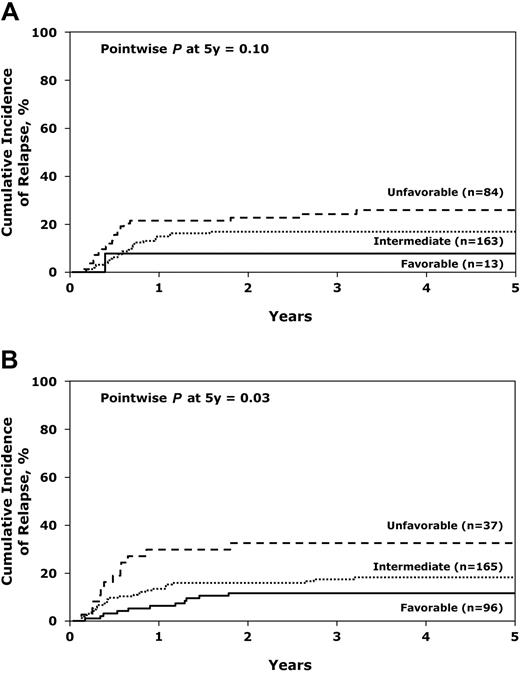
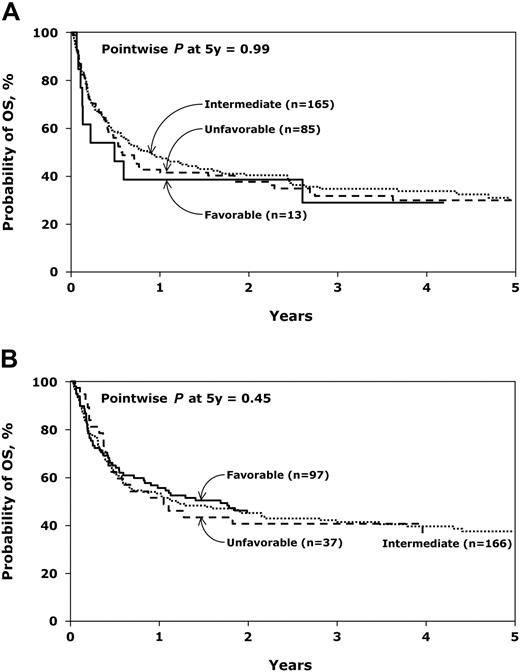
The TRM at 100 days and 5 years, respectively, for patients in CR1 among patients with favorable cytogenetics was 46% (95% CI, 21%-72%) and 63% (95% CI, 36%-87%), respectively; 32% (95% CI, 25%-39%) and 53% (95% CI, 45%-62%), respectively, for patients with intermediate cytogenetics; and 29% (95% CI, 19%-39%) and 47% (95% CI, 36%-58%), respectively, for patients with unfavorable cytogenetics (Table 3, Figure 1A). The relapse rates at 5 years were 8% (95% CI, 0%-28%), 17% (95% CI, 11%-23%), and 26% (95% CI, 17%-36%), for patients with favorable, intermediate, and unfavorable cytogenetics, respectively (Figure 2A). The DFS at 5 years for the patients with favorable, intermediate, and unfavorable cytogenetics was 29% (95% CI, 8%-56%), 30% (95% CI, 22%-38%), and 27% (95% CI, 19%-39%), respectively (Figure 3A). The OS for patients with favorable, intermediate, and unfavorable cytogenetics was 29% (95% CI, 8%-56%), 30% (95% CI, 22%-38%), and 30% (95% CI, 20%-41%), respectively (Figure 4A).
Cumulative incidence of treatment-related mortality. (A) Comparison of treatment-related mortality after unrelated donor transplantation for AML in first complete remission by cytogenetic risk group. (B) Comparison of treatment-related mortality after unrelated donor transplantation for AML in second complete remission by cytogenetic risk group.
Cumulative incidence of treatment-related mortality. (A) Comparison of treatment-related mortality after unrelated donor transplantation for AML in first complete remission by cytogenetic risk group. (B) Comparison of treatment-related mortality after unrelated donor transplantation for AML in second complete remission by cytogenetic risk group.
Cumulative incidence of relapse. (A) Comparison of relapse after unrelated donor transplantation for AML in first complete remission by cytogenetic risk group. (B) Comparison of relapse after unrelated donor transplantation for AML in second complete remission by cytogenetic risk group.
Cumulative incidence of relapse. (A) Comparison of relapse after unrelated donor transplantation for AML in first complete remission by cytogenetic risk group. (B) Comparison of relapse after unrelated donor transplantation for AML in second complete remission by cytogenetic risk group.
Probability of disease-free survival. (A) Comparison of disease-free survival after unrelated donor transplantation for AML in first complete remission by cytogenetic risk group. (B) Comparison of disease-free survival after unrelated donor transplantation for AML in second complete remission by cytogenetic risk group.
Probability of disease-free survival. (A) Comparison of disease-free survival after unrelated donor transplantation for AML in first complete remission by cytogenetic risk group. (B) Comparison of disease-free survival after unrelated donor transplantation for AML in second complete remission by cytogenetic risk group.
Probability of overall survival. (A) Comparison of overall survival after unrelated donor transplantation for AML in first complete remission by cytogenetic risk group. (B) Comparison of overall survival after unrelated donor transplantation for AML in second complete remission by cytogenetic risk group.
Probability of overall survival. (A) Comparison of overall survival after unrelated donor transplantation for AML in first complete remission by cytogenetic risk group. (B) Comparison of overall survival after unrelated donor transplantation for AML in second complete remission by cytogenetic risk group.
Univariate analyses of patients who underwent unrelated donor transplantation for AML, by disease status prior to transplantation and cytogenetics risk group
| Outcome . | Favorable . | Intermediate . | Unfavorable . | P* . |
|---|---|---|---|---|
| First complete remission, n | 13 | 164 | 84 | |
| Treatment-related mortality, %, (95% CI) | ||||
| At 100 d | 46 (21-72) | 32 (25-39) | 29 (19-39) | .48 |
| At 3 y | 63 (36-87) | 50 (42-57) | 47 (36-58) | .55 |
| At 5 y | 63 (36-87) | 53 (45-62) | 47 (36-58) | .46 |
| Relapse, no. %, (95% CI) | ||||
| At 3 y | 8 (0-28) | 17 (11-23) | 26 (17-36) | .10 |
| At 5 y | 8 (0-28) | 17 (11-23) | 26 (17-36) | .10 |
| Disease-free survival, no. %, (95% CI) | ||||
| At 3 y | 29 (8-56) | 33 (26-41) | 29 (19-39) | .73 |
| At 5 y | 29 (8-56) | 30 (22-38) | 27 (19-39) | .92 |
| Overall survival, %, (95% CI) | ||||
| At 3 y | 29 (8-56) | 35 (27-42) | 32 (22-42) | .85 |
| At 5 y | 29 (8-56) | 30 (22-38) | 30 (20-41) | .99 |
| Second complete remission, n | 97 | 165 | 37 | |
| Treatment-related mortality, %, (95% CI) | ||||
| At 100 d | 27 (19-36) | 22 (16-28) | 16 (6-30) | .34 |
| At 3 y | 46 (40-52) | 44 (36-51) | 30 (16-45) | .13 |
| At 5 y | 46 (36-56) | 46 (39-54) | 30 (16-45) | .13 |
| Relapse, %, (95% CI) | ||||
| At 3 y | 12 (6-19) | 17 (12-24) | 32 (19-48) | .038 |
| At 5 y | 12 (6-19) | 18 (13-25) | 32 (19-48) | .033 |
| Disease-free survival, %, (95% CI) | ||||
| At 3 y | 42 (33-52) | 39 (32-47) | 38 (23-54) | .83 |
| At 5 y | 42 (33-52) | 35 (28-43) | 38 (23-54) | .56 |
| Overall survival, no. %, (95% CI) | ||||
| At 3 y | 45 (35-55) | 42 (35-50) | 41 (25-57) | .86 |
| At 5 y | 45 (35-55) | 37 (30-45) | 36 (21-53) | .45 |
| Outcome . | Favorable . | Intermediate . | Unfavorable . | P* . |
|---|---|---|---|---|
| First complete remission, n | 13 | 164 | 84 | |
| Treatment-related mortality, %, (95% CI) | ||||
| At 100 d | 46 (21-72) | 32 (25-39) | 29 (19-39) | .48 |
| At 3 y | 63 (36-87) | 50 (42-57) | 47 (36-58) | .55 |
| At 5 y | 63 (36-87) | 53 (45-62) | 47 (36-58) | .46 |
| Relapse, no. %, (95% CI) | ||||
| At 3 y | 8 (0-28) | 17 (11-23) | 26 (17-36) | .10 |
| At 5 y | 8 (0-28) | 17 (11-23) | 26 (17-36) | .10 |
| Disease-free survival, no. %, (95% CI) | ||||
| At 3 y | 29 (8-56) | 33 (26-41) | 29 (19-39) | .73 |
| At 5 y | 29 (8-56) | 30 (22-38) | 27 (19-39) | .92 |
| Overall survival, %, (95% CI) | ||||
| At 3 y | 29 (8-56) | 35 (27-42) | 32 (22-42) | .85 |
| At 5 y | 29 (8-56) | 30 (22-38) | 30 (20-41) | .99 |
| Second complete remission, n | 97 | 165 | 37 | |
| Treatment-related mortality, %, (95% CI) | ||||
| At 100 d | 27 (19-36) | 22 (16-28) | 16 (6-30) | .34 |
| At 3 y | 46 (40-52) | 44 (36-51) | 30 (16-45) | .13 |
| At 5 y | 46 (36-56) | 46 (39-54) | 30 (16-45) | .13 |
| Relapse, %, (95% CI) | ||||
| At 3 y | 12 (6-19) | 17 (12-24) | 32 (19-48) | .038 |
| At 5 y | 12 (6-19) | 18 (13-25) | 32 (19-48) | .033 |
| Disease-free survival, %, (95% CI) | ||||
| At 3 y | 42 (33-52) | 39 (32-47) | 38 (23-54) | .83 |
| At 5 y | 42 (33-52) | 35 (28-43) | 38 (23-54) | .56 |
| Overall survival, no. %, (95% CI) | ||||
| At 3 y | 45 (35-55) | 42 (35-50) | 41 (25-57) | .86 |
| At 5 y | 45 (35-55) | 37 (30-45) | 36 (21-53) | .45 |
Pointwise P value.
Patients in CR2.
The TRM at 100 days and 5 years, respectively, was 27% (95% CI, 19%-36%) and 46% (95% CI, 36%-56%); 22% (95% CI, 16%-28%) and 46% (95% CI, 39%-54%); and 16% (95% CI, 6%-30%) and 30% (95% CI, 16%-45%) for patients with favorable, intermediate, and unfavorable cytogenetics, respectively (Table 3; Figure 1B). The cumulative incidence of relapse at 5 years for the 3 groups was 12% (95% CI, 6%-19%), 18% (95% CI, 13%-25%), and 32% (95% CI, 19%-48%) (Figure 2B). The DFS at 5 years was 42% (95% CI, 33%-52%), 35% (95% CI, 28%-43%), and 38% (95% CI, 23%-54%) (Figure 3B). The OS at 5 years was 45% (95% CI, 33%-55%), 37% (95% CI, 30%-45%), and 36% (95% CI, 21%-53%) (Figure 4B).
Multivariate analyses
Patients in CR1.
In multivariate analyses, for patients in CR1, significant variables associated with worse DFS included cell dose lower than 3 × 108/kg (P = .010) (within the first 6 months after transplantation), and receiving an HLA-mismatched transplant (P < .001) (beyond the first 3 months after transplantation) (Table 4). For OS, significant variables were cell dose lower than 3 × 108/kg (P < .001) (within the first 6 months after transplantation) and receiving an HLA-mismatched transplant (P < .001) (beyond first 3 months after transplantation) (Table 4). TRM was significantly higher for patients who were CMV seropositive (P = .007) (Table 4). The TRM was higher in the first 6 months after HSCT for patients with a graft cell dose of 3 × 108 or fewer nucleated cells/kg (P < .001) and for those patients whose time from diagnosis to transplantation was greater than 6 months (P = .016). The TRM for patients in CR1 was not significantly associated with cytogenetic subgroups (P = .65). Among patients in CR1, relapse was significantly associated with unfavorable risk cytogenetics (P = .009), HLA-mismatched transplants (P < .001), time from diagnosis to transplantation less than 6 months (P = .015), and receiving T-cell–depleted transplants (P = .013) (Table 4).
Multivariate analyses of cytogenetic risk groups after unrelated donor transplantation for AML in first complete remission
| Outcome . | No. . | Relative risk (95% CI) . | P . |
|---|---|---|---|
| Treatment-related mortality* | |||
| Intermediate | 155 | 1.00‖ | |
| Unfavorable | 82 | 0.91 (0.62-1.35) | .65 |
| Relapse† | |||
| Intermediate | 155 | 1.00‖ | |
| Unfavorable | 82 | 2.22 (1.22-4.06) | .009 |
| Treatment failure‡ | |||
| Intermediate | 155 | 1.00‖ | |
| Unfavorable | 82 | 1.23 (0.89-1.70) | .21 |
| Death§ | |||
| Intermediate | 155 | 1.00‖ | |
| Unfavorable | 82 | 1.14 (0.82-1.59) | .43 |
| Outcome . | No. . | Relative risk (95% CI) . | P . |
|---|---|---|---|
| Treatment-related mortality* | |||
| Intermediate | 155 | 1.00‖ | |
| Unfavorable | 82 | 0.91 (0.62-1.35) | .65 |
| Relapse† | |||
| Intermediate | 155 | 1.00‖ | |
| Unfavorable | 82 | 2.22 (1.22-4.06) | .009 |
| Treatment failure‡ | |||
| Intermediate | 155 | 1.00‖ | |
| Unfavorable | 82 | 1.23 (0.89-1.70) | .21 |
| Death§ | |||
| Intermediate | 155 | 1.00‖ | |
| Unfavorable | 82 | 1.14 (0.82-1.59) | .43 |
CI indicates confidence interval.
Other significant covariates were recipient CMV status (positive vs negative: RR = 1.71, 95% CI, 1.16–2.53, P = .007); cell dose (Poverall2 < 0.001; ≤ 3 × 108/kg vs > 3 × 108/kg within first 6 months after transplantation: RR = 2.99, 95% CI, 1.73-5.18, P < .001; cell dose ≤ 3 × 108/kg vs > 3 × 108/kg beyond first 6 months after transplantation: RR = 0.78, 95% CI, 0.36-1.72, P = 0.54) and time from diagnosis to transplant (>6 months vs <6 months: RR = 1.58, 95% CI = 1.09-2.29, P = .016).
Other significant covariates were donor-recipient HLA match (mismatch vs match: RR = 4.41, 95% CI = 2.27-8.59, P < .001), time from diagnosis to transplantation (> 6 months vs ≤ 6 months: RR = .45, 95% CI = 0.23-0.86, P = .015) and GVHD prophylaxis (Poverall2 = 0.030; FK506 ± other vs CSA + MTX ± other: RR = 0.57, 95% CI = 0.25-1.32, P = .19; T-cell depletion vs CSA + MTX ± other: RR = 0.39, 95% CI = 0.19-0.82, P = .013; T-cell depletion vs FK506 ± other: RR = 0.68, 95% CI = 0.25-1.89, P = .46).
Other significant covariates were cell dose (Poverall2 = 0.029; ≤ 3 × 108/kg vs > 3 × 108/kg within first 6 months after transplantation: RR = 1.74, 95% CI = 1.14-2.66, P = .010; cell dose ≤ 3 × 108/kg vs > 3 × 108/kg beyond first 6 months after transplant: RR = 0.82, 95% CI = 0.46-1.44, P = 0.49) and donor-recipient HLA match (Poverall2 < 0.001; mismatch vs match within first 3 months after transplantation: RR = 1.03, 95% CI = 0.61-1.72, P = 0.92; mismatch vs match beyond first 3 months after transplantation: RR = 2.51, 95% CI = 1.60-3.94, P < .001).
Other significant covariates were cell dose (Poverall2<0.001; ≤ 3 × 108/kg vs > 3 × 108/kg within first 6 months after transplantation: RR = 2.53, 95% CI = 1.56-4.08, P < .001; cell dose ≤ 3 × 108/kg vs > 3 × 108/kg beyond first 6 months after transplantation: RR = 0.68, 95% CI = 0.40-1.15, P = .15) and donor-recipient HLA match (Poverall2 = 0.001; mismatch vs match within first 3 months after transplantation: RR = 0.94, 95% CI = 0.56-1.60, P = .83; mismatch vs match beyond first 3 months after transplantation: RR = 2.31, 95% CI = 1.48-3.59, P < .001).
Reference group.
Patients in CR2.
For DFS, significant variables associated with outcome included recipient age 19 to 35 years (P = .07) and older than 35 years (P = .005); and receiving conditioning regimens other than Cy + TBI ± other (P = .036) or Bu + Cy ± other (P = .004) (Table 5). Variables negatively influencing OS included recipient age 19 to 35 years (P = .017) and older than 35 years (P = .001); and receiving an HLA-mismatched transplant (P = .042) (Table 5). Significant variables associated with higher TRM included age 19 to 35 years (P = .009), age older than 35 years (P < .001), CMV seropositivity (P = .020), HLA mismatch (P = .027), and receiving conditioning regimens other than Cy + TBI ± other (P = .03) or Bu + Cy ± other (P = .011) (Table 5). The TRM was not significantly associated with cytogenetics (P = .57). Relapse was somewhat more frequent in patients with unfavorable cytogenetics compared with favorable cytogenetics (P = .037) (although the overall test comparing all 3 groups is not significant, P = .11), and duration of CR1 less than 12 months (P = .015) (within the first 6 months after transplantation) (Table 5).
Multivariate analyses of cytogenetic risk groups after unrelated donor transplantation for AML in second complete remission
| Outcome . | No. . | Relative risk (95% CI) . | P . |
|---|---|---|---|
| Treatment-related mortality* | |||
| Favorable | 94 | 1.00‖ | Poverall2 = .57 |
| Intermediate | 163 | 0.95 (0.65-1.38) | .77 |
| Unfavorable | 36 | 0.70 (0.36-1.36) | .29 |
| Relapse† | |||
| Favorable | 94 | 1.00‖ | Poverall2 = .11 |
| Intermediate | 163 | 1.54 (0.76-3.09) | .23 |
| Unfavorable | 36 | 2.48 (1.06-5.80) | .037 |
| Treatment failure‡ | |||
| Favorable | 94 | 1.00‖ | Poverall2 = .66 |
| Intermediate | 163 | 1.16 (0.84-1.61) | .37 |
| Unfavorable | 36 | 1.15 (0.70-1.90) | .57 |
| Death§ | |||
| Favorable | 95 | 1.00‖ | Poverall2 = .81 |
| Intermediate | 163 | 1.12 (0.80-1.56) | .52 |
| Unfavorable | 36 | 1.10 (0.66-1.81) | .72 |
| Outcome . | No. . | Relative risk (95% CI) . | P . |
|---|---|---|---|
| Treatment-related mortality* | |||
| Favorable | 94 | 1.00‖ | Poverall2 = .57 |
| Intermediate | 163 | 0.95 (0.65-1.38) | .77 |
| Unfavorable | 36 | 0.70 (0.36-1.36) | .29 |
| Relapse† | |||
| Favorable | 94 | 1.00‖ | Poverall2 = .11 |
| Intermediate | 163 | 1.54 (0.76-3.09) | .23 |
| Unfavorable | 36 | 2.48 (1.06-5.80) | .037 |
| Treatment failure‡ | |||
| Favorable | 94 | 1.00‖ | Poverall2 = .66 |
| Intermediate | 163 | 1.16 (0.84-1.61) | .37 |
| Unfavorable | 36 | 1.15 (0.70-1.90) | .57 |
| Death§ | |||
| Favorable | 95 | 1.00‖ | Poverall2 = .81 |
| Intermediate | 163 | 1.12 (0.80-1.56) | .52 |
| Unfavorable | 36 | 1.10 (0.66-1.81) | .72 |
CI indicates confidence interval.
Unfavorable vs intermediate: RR = 0.74, 95% CI = 0.39-1.40, P = .74. Other significant covariates were age at transplantation (Poverall2 = 0.002; 19-35 years vs ≤ 18 years: RR = 1.86, 95% CI = 1.17-2.95, P = .009; > 35 years vs ≤ 18 years: RR = 2.26, 95% CI = 1.43-3.59, P < .001; > 35 years vs 19-35 years: RR = 1.22, 95% CI = 0.82-1.81, P = .33), recipient CMV status (positive vs negative: RR = 1.53, 95% CI, 1.07-2.18, P = .020); conditioning regimen (Poverall2 = 0.034; Bu + Cy ± other vs CyTBI ± other: RR = 0.71, 95% CI = 0.41-1.23, P = .23; other vs CyTBI ± other: RR = 1.97, 95% CI = 1.07-3.63, P = .030; other vs BuCy ± other: RR = 2.76, 95% CI = 1.27-6.02, P = .011) and donor-recipient HLA match (mismatch vs match: RR = 1.53, 95% CI = 1.05-2.22, P = .027).
Unfavorable vs intermediate: RR = 1.61, 95% CI = 0.80-3.25, P = .18. Other significant covariate was duration of first CR (time-dependent covariate). The effect of duration of first CR differs with the length of time after transplantation (> 12 months vs ≤ 12 months within first 6 months after transplantation: RR = 0.08, 95% CI = 0.01-0.62, P = .15; > 12 months vs ≤ 12 months beyond first 6 months after transplantation: RR = 1.86, 95% CI = 0.86-4.00, P = .11).
Unfavorable vs intermediate: RR = 0.99, 95% CI = 0.62-1.58, P = .98. Other significant covariates were age at transplantation (Poverall2 = 0.017; 19-35 years vs ≤ 18 years: RR = 1.40, 95% CI = 0.97-2.03, P = .07; > 35 years vs ≤ 18 years: RR = 1.70, 95% CI = 1.18-2.45, P = .005; > 35 years vs 19-35 years: RR = 1.21, 95% CI = 0.85-1.71, P = .29) and conditioning regimen (Poverall2 = 0.017; Bu + Cy ± other vs CyTBI ± other: RR = 0.68, 95% CI = 0.43-1.06, P = .09; other vs CyTBI ± other: RR = 1.82, 95% CI = 1.04-3.18, P = .036; other vs BuCy ± other: RR = 2.69, 95% CI = 1.36-5.32, P = .004).
Unfavorable vs intermediate: RR = 0.89, 95% CI = 0.64-1.25, P = .94. Other significant covariates were age at transplantation (Poverall2 = 0.005; 19-35 years vs ≤ 18 years: RR = 1.58, 95% CI = 1.08-2.29, P = .017; > 35 years vs ≤ 18 years: RR = 1.83, 95% CI = 1.26-2.67, P = .001; > 35 years vs 19-35 years: RR = 1.16, 95% CI = 0.82-1.65, P = .39) and donor-recipient HLA match (mismatch vs match: RR = 1.40, 95% CI = 1.01-1.95, P = .042).
Reference group.
Discussion
The curative potential of allogeneic HSCT is attributable, in part, to the potent graft-versus-leukemia effect generated by reactivity of donor cells against recipient tissues including persistent or residual recipient leukemia cells.13,14 Theoretically, the potency of this reaction correlates with the degree of genetic disparity, although other factors contribute to the effectiveness of GVL.15,16 This hypothesis was tested by determining the outcome by cytogenetic risk classification following MUD HSCT for patients with AML in either CR1 or CR2. Neither DFS nor OS was adversely influenced by the presence of unfavorable cytogenetics. The relapse rate was higher among patients in either CR1 or CR2 with unfavorable cytogenetics compared with those with favorable or intermediate cytogenetics, although the number of patients with favorable cytogenetics was quite small. This suggests that, in fact, MUD HSCT was less effective as an antileukemic strategy among patients with unfavorable cytogenetics than among patients with intermediate cytogenetics both in CR1 and CR2. It may be that DFS and OS were similar in the 3 risk groups because the TRM among the favorable- and intermediate-risk groups was higher; negating any advantage they might have otherwise had because of a lower relapse rate. Slower hematopoietic and immune reconstitution with bone marrow–derived stem cells as opposed to those derived from blood, may have contributed to the TRM.17 The higher incidence of CMV seropositivity among CR1 patients with unfavorable cytogenetics may have contributed to the TRM. In addition, the fact that more patients in CR2 with unfavorable cytogenetics were CMV seronegative may have contributed to such patients faring better than expected. Strategies to reduce TRM may be beneficial. However, it is possible that if TRM decreases and more patients survive, relapse of cytogenetically defined high risk AML may be modestly reduced by MUD HSCT.
Despite the higher relapse rate among patients with unfavorable cytogenetics, the outcome appears significantly better than that achieved with conventional induction and consolidation chemotherapy.11,18 With aggressive chemotherapy, the OS for patients with unfavorable cytogenetics is only approximately 5% to 10%.11,18 Our data, therefore, suggest that the strategy of MUD HSCT should be considered in all patients with unfavorable cytogenetics at diagnosis. This same recommendation cannot be made for patients with intermediate-risk cytogenetics in CR1 since the 5-year DFS was only 30%, which is not generally different from that obtained with chemotherapy. Autologous HSCT may be an alternative treatment for patients with unfavorable cytogenetics. Although a recent study from the CIBMTR suggested that such an approach was associated with a better outcome than MUD HSCT, the influence of cytogenetics in this study is unknown.5 However, the US Intergroup found autologous HSCT was not protective against the poor prognosis associated with unfavorable cytogenetics.8
We recognize several important limitations of this analysis including the fact that cytogenetics were not centrally reviewed, potential lead time biases may have been introduced, and the presence of the possible influence of recently described molecular prognostic factors. While the time required for transplantation may have excluded some high-risk patients because of relapse, the patients who underwent transplantation represented a cohort with well-described adverse cytogenetics. Most of the recently described unfavorable molecular prognostic factors are not routinely available when these patient data were collected. It should also be acknowledged that some patent cohorts have relatively small number of patients, and the preparative regimens and prophylactic regimens for GVHD prophylaxis are heterogeneous. Given the relatively small number of patients in some groups, it is possible that small differences in classification of cytogenetics risk groups may influence results. We found that using the classifications established by both the CALGB11 and MRC,18 there were no differences in the cause-specific ratios comparing results for overall survival. Patients with unfavorable cytogenetics fare less well than those with favorable or intermediate cytogenetics following HLA-matched sibling allogeneic HSCT.9,19,20 While several studies have assessed factors associated with more favorable outcome after MUD HSCT, none have evaluated the influence of cytogenetics. Beatty et al have shown that the relapse associated with mismatched donors is lower than with matched unrelated donors.21 However, OS was not different, and a multivariate analysis did not identify an association between genetic disparity and OS. Sierra et al reported that transplantation in CR, a marrow cell dose higher than 3.5 × 108/kg, and CMV seronegative status before MUD HSCT in the donor and recipient were favorable prognostic factors for outcome.6 In this study, all patients undergoing transplantation in CR1 had adverse prognostic features including, but not confined to, unfavorable cytogenetics (6 patients). Six others were classified as high risk because of difficulty achieving CR and 2 had acute megakaryocytic leukemia. Despite these adverse prognostic features, the outcome was excellent after MUD HSCT with leukemia-free survival of 50% at 5 years, although the total number of patients was small and the influence of unfavorable cytogenetics was not directly tested. Chown et al reported favorable outcome for a small series of children and young adults with AML in remission with high-risk features including one patient with FAB M6 AML, one with mixed lineage leukemia and monosomy 7, one who had failed induction and had an elevated white blood cell count, another who had failed induction with unfavorable cytogenetics, and a fifth patient with FAB M1 AML and a history of antecedent myelodysplastic syndrome.22 In this small study, the median age was 13 years (range, 4–31 years) and no formal analysis by cytogenetics was undertaken. In the present study, only cell dose and degree of mismatching influenced overall outcome (DFS and OS) among patients in CR1. Recipient age and conditioning regimen affected DFS and recipient age and degree of mismatching affected OS among patients in CR2.
Several new approaches may improve the outcome for patents undergoing MUD HSCT. In an effort to diminish TRM among recipients of MUD transplants, a similar strategy, but with nonmyeloablative conditioning has been explored23,24 with cumulative nonrelapse mortality of approximately 22%.25 Furthermore, the use of granulocyte colony-stimulating factor–stimulated peripheral blood mononuclear cells instead of marrow-derived cells resulted in higher donor T-cell chimerism and improved OS. This strategy further exploits potential GVL and may prove useful, particularly for patients with unfavorable cytogenetics who are often older adults and unable to tolerate a conventional ablative HSCT. Transplantation of stem cells derived from matched unrelated umbilical cord is an attractive alternative strategy which is under study.26,27 Stem cells from cord blood are quickly available and the time to locate a suitable donor unit can be as short as 2 weeks. Reduced-intensity (nonmyeloablative) conditioning with umbilical cord HSCT is associated with a low incidence of acute graft-versus-host disease.28,29 Very recent data suggest that double umbilical cord blood transplantation (UCBT) may be associated with reduced relapsed rates compared with single unit infusions.30 However, whether such as approach generates sufficient GVL to protect against relapse and improve outcome in patents with unfavorable cytogenetics has not been determined.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The CIBMTR is supported by Public Health Service Grant U24-CA76518 from the National Cancer Institute, the National Institute of Allergy and Infectious Diseases, and the National Heart, Lung and Blood Institute. Supported also by the Office of Naval Research; Health Services Research Administration (DHHS); grants from AABB, Abbott Laboratories; Aetna; AIG Medical Excess; American Red Cross; Amgen; an anonymous donation to the Medical College of Wisconsin; AnorMED; Astellas Pharma US; Berlex Laboratories; Biogen IDEC; Blue Cross and Blue Shield Association; BRT Laboratories; Celgene; Cell Therapeutics; CelMed Biosciences; Cubist Pharmaceuticals; Dynal Biotech, LLC; Edwards Lifesciences RMI; Endo Pharmaceuticals; Enzon Pharmaceuticals; ESP Pharma; Gambro BCT; Genzyme Corporation; GlaxoSmithKline; Histogenetics; Human Genome Sciences; International Waldenstrom Macroglobulinemia Foundation; Kirin Brewery Company; Ligand Pharmaceuticals; Merck & Company; Millennium Pharmaceuticals; Miller Pharmacal Group; Milliman USA; Miltenyi Biotec; National Center for Biotechnology Information; National Leukemia Research Association; National Marrow Donor Program; Nektar Therapeutics; NeoRx Corporation; Novartis Pharmaceuticals; Novo Nordisk Pharmaceuticals; Ortho Biotech; Osiris Therapeutics; Pall Medical; Pfizer; Pharmion; Protein Design Labs; QOL Medical; Roche Laboratories; StemCyte; Stemco Biomedical; StemSoft Software; SuperGen; Sysmex; The Marrow Foundation; THERAKOS, a Johnson & Johnson Company; University of Colorado Cord Blood Bank; Valeant Pharmaceuticals; ViaCell; ViraCor Laboratories; WB Saunders Mosby Churchill; Wellpoint; and Zelos Therapeutics
Authorship
Contribution: M.S.T. had primary responsibility for study design, data analysis, interpretation, and paper writing; also, M.S.T. had primary responsibility for the entire paper as an accurate, and verifiable report; G.W.D. participated in the cytogenetic reports review, interpretation of data, and paper writing; S.G. had primary responsibility for data file preparation, data analysis, and interpretation of data; B.R.L. participated in study design, analyzed data, and interpreted data; A.K. participated in interpretation of data and paper writing; H.M.L. participated in interpretation of data and paper writing; M.R.L. participated in interpretation of data and paper writing; J.M. participated in interpretation of data and paper writing; T.P. participated in the cytogenetic reports review; W.S.P. participated in data analysis and had primary responsibility for the entire paper as an accurate and verifiable report; J.M.R. participated in interpretation of data and paper writing; M.W. participated in interpretation of data and paper writing; D.J.W. had primary responsibility for study design, data analysis, interpretation, and paper writing. Also, D.J.W. had primary responsibility for the entire paper as an accurate and verifiable report.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Martin S. Tallman, Northwestern University Feinberg School of Medicine, 676 N St Clair, Suite 850, Chicago, IL 60611; e-mail: m-tallman@northwestern.edu.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal