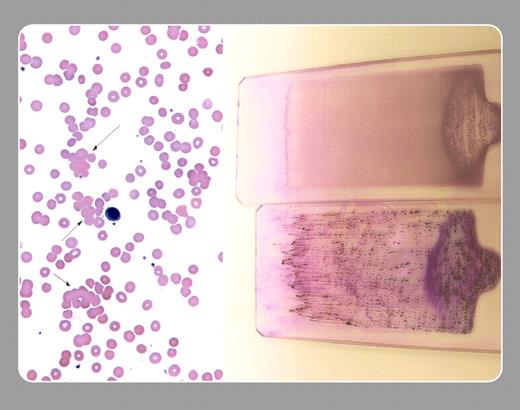
A 72-year-old gentleman was referred for a chronic low-grade anemia. Family history was negative. He had slightly enlarged lymph nodes and minimal hepatosplenomegaly. His peripheral smear showed a predomi nance (70%) of lymphocytes, normal platelets, and clumping of red cells (arrows in left panel). Serum electrophoresis showed a small IgM “M” component.
The recognition of the clumped red cells prompted the physician to cool the blood sample, and another smear was made. The warmer (room temperature) blood is shown on the top right and the slide of the chilled blood is on the bottom right. Macroscopic clumps of red cells, similar to those seen on the glass slide, were also noted on the wall of the test tube. The red cells were C3 Coombs–positive and IgG Coombs–negative. Clumped red cells and those that are not clumped but are in the vicinity spread poorly on peripheral smears and may resemble spherocytes. The cold agglutinin titer was positive at 1:640 000 and was the “M” component noted above.
A diagnosis of cold agglutinin hemolytic anemia was made. A transient cold agglutinin hemolytic anemia may occur with an infection (eg, mycoplasma). However, this man had a lymphoproliferative disease. Commonly, patients with cold agglutinin hemolytic anemia have no underlying disease (idiopathic cold agglutinin hemolytic anemia), but some of them evolve later to develop a lymphoproliferative disorder.
Many Blood Work images are provided by the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas images and images of case studies. For more information or to contribute to the Image Bank, visit www.ashimagebank.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal