Abstract
Background: Cytotoxic T-cell infiltrates are a nearly universal finding in the bone marrow of patients with multiple myeloma. It has been postulated that presence of T-cells in the bone marrow of multiple myeloma (MM) patients represents an immune response against the tumor and therefore, might be associated with an improved prognosis. However, the impact of bone marrow T-cells on the prognosis of multiple myeloma patients has not been studied systematically.
Methods: Bone marrow biopsies of patients with newly diagnosed multiple myeloma were stained by immnohistochemistry for the CD8 antigen and reviewed by a blinded hematopathologist. Three high power fields are reviewed for each biopsy and the total number of CD8 positive cells counted and reported. For patients with more than 300 cells per 3 fields, results were reported as >300. The number of bone marrow CD8 positive cells was then correlated with patients’ clinical data, including other prognostic factors and overall survival.
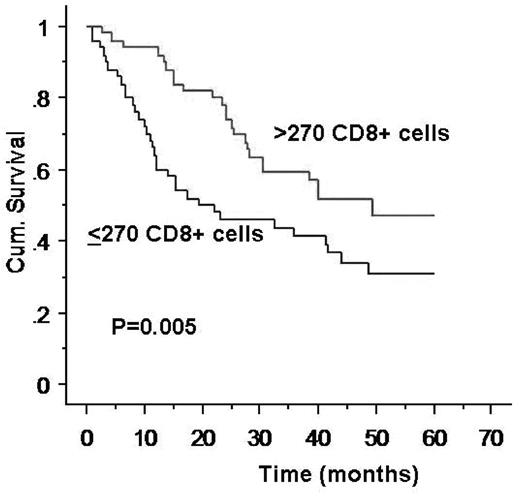
Results: Bone marrow biopsy specimens from 100 patients, performed within the week of a diagnosis of multiple myeloma and collected between May 1998 and January 2001 were evaluated. The median number of CD8 positive cells was 270 (33 – >300). Patients’ characteristics are shown in Table 1. Median follow up was 30 months (0–80). The number of cytotoxic T-cells as a continuous variable was a risk factor for shortened overall survival, HR 1.86 (95% CI 1.11–3.35). Using minimal p value approach, the cutoff of 270 cells (the median) risk stratified patients into two groups: the median survival of patients with > 270 CD8 positive cells was 16 months vs. 48 months in patients with ≤270 cells, p=0.005 (Figure). In multivariate analysis including age, B2M, albumin, CRP, bone marrow plasma cell percentage and plasma cell labeling index, the number of cytotoxic T-cells was an independent predictor of overall survival was HR 3.1, p=0.0017.
Conclusion: We show that the number of cytotoxic T-cells in the bone marrow is a strong and independent prognostic factor in patients with newly diagnosed multiple myeloma. Our observation does not contradict the hypothesis that cytotoxic T-cells participate in an immune response against the tumor since our findings may represent a higher level of immune response associated with baseline aggressive disease biology. However, our study suggests for the first time that increased marrow cytotoxic T-cells have an adverse effect on outcome in myeloma, and suggest that these cells may have a direct facilitating effect on tumor growth and on the marrow microenvironment. Further studies of the biology of behind this observation are warranted.
| Characteristic . | N . | Median (range) . |
|---|---|---|
| Gender male | 61 | |
| CRP | 81 | 0.4mg/L (0.01–11.2) |
| Albumin | 99 | 3.6 g/dL (2.6–5.4) |
| B2microglobulin | 94 | 4.0 (0.9–28) μg/mL |
| Marrow PC% | 90 | 45% (11–99) |
| PC labeling index | 90 | |
| high (>1%) | 36 | |
| BM CD8 cells | 100 | 270 (33 – >300) |
| ISS | 94 | |
| 1 | 19 | |
| 2 | 41 | |
| 3 | 34 |
| Characteristic . | N . | Median (range) . |
|---|---|---|
| Gender male | 61 | |
| CRP | 81 | 0.4mg/L (0.01–11.2) |
| Albumin | 99 | 3.6 g/dL (2.6–5.4) |
| B2microglobulin | 94 | 4.0 (0.9–28) μg/mL |
| Marrow PC% | 90 | 45% (11–99) |
| PC labeling index | 90 | |
| high (>1%) | 36 | |
| BM CD8 cells | 100 | 270 (33 – >300) |
| ISS | 94 | |
| 1 | 19 | |
| 2 | 41 | |
| 3 | 34 |
Figure
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal