Abstract
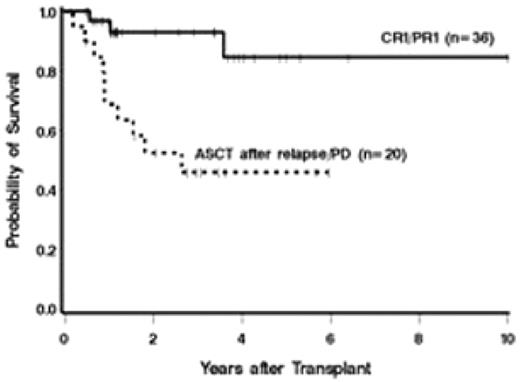
Mantle cell lymphoma (MCL) has one of the worst prognoses of any subtype of non-Hodgkin’s lymphoma (NHL), with a median survival of 3–4 years in most series. High-dose therapy followed by autologous stem cell transplantation (ASCT) is an increasingly common treatment approach for MCL, and some ASCT studies suggest that less heavily pre-treated patients have a longer duration of progression-free survival (PFS), suggesting that ASCT may lead to more favorable outcomes if used earlier in the course of therapy. We analyzed the outcomes of ASCT with respect to remission status at the time of transplantation and induction regimen used in 56 consecutive transplanted patients with MCL. Twenty-one patients received induction chemotherapy with HyperCVAD with or without rituximab (±R) followed by ASCT in first complete or partial remission (CR1/PR1), 15 received CHOP (±R) followed by ASCT in CR1/PR1, and 20 received ASCT following disease progression. A variety of conditioning regimens were used for ASCT in all 3 groups. Estimates of overall (OS) and progression-free survival (PFS) at 3 years among patients transplanted in CR1/PR1 were 93% and 63%, compared with 46% and 36% for patients transplanted with relapsed or refractory disease, respectively (Figure 1). The hazard of mortality among patients transplanted with relapsed or refractory disease was 6.09 times that of patients transplanted in CR1/PR1 (P=.006). Patients in the CHOP (±R) group appeared to have a higher risk of failure for PFS compared to patients in the HyperCVAD (±R) group, though the difference did not reach statistical significance (hazard ratio [HR] 3.67, P=.11) with the small sample size available. The estimated 3-year PFS was 81% for patients in the HyperCVAD group and 44% for patients in the CHOP group. Patients who received R with induction therapy had a reduced risk of mortality (HR 0.33, P=.05) and failure for PFS (HR 0.28, P=.005) compared to those who did not. In summary, these results suggest that ASCT in first remission leads to improved survival outcomes for patients with MCL compared to ASCT with relapsed or refractory disease, and a HyperCVAD (±R) induction regimen may be associated with an improved PFS among patients transplanted in CR1/PR1.
Kaplan-Meier estimates of overall survival from the time of ASCT, with respect to remission status at ASCT.
Kaplan-Meier estimates of overall survival from the time of ASCT, with respect to remission status at ASCT.
Author notes
Disclosure:Research Funding: L.H. received funding for clinical trials from Celgene, RPR, and Genzyme corporations. A.K.G. received research support from GlaxoSmithKline, Lilly, Seattle Genetics and Biogen-Idec. Honoraria Information: A.K.G. has received honoraria from Millenium Pharmaceuticals.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal