Abstract
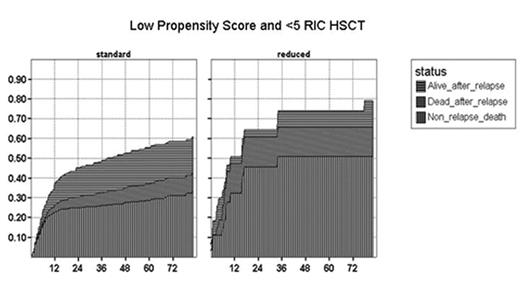
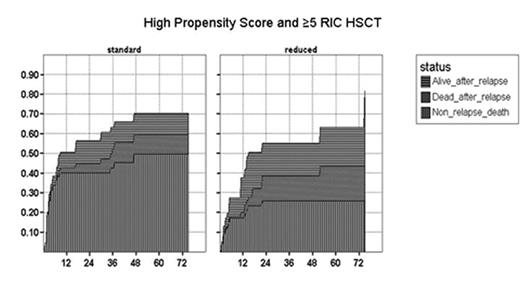
Allogeneic transplantation continues to have a role in the management of high risk CML. However the place of reduced intensity (RIC) versus myeloablative conditioning (MAC) is uncertain in younger patients. A total of 2331 first HSCT’s performed from 1998–2005 were reported to the European Group for Blood and Marrow Transplantation Registry, RIC was used in 276 and MAC in 2055. Overall survivals were similar for the first 9 months. After 9 months the survival curves separated (HR for RIC 1.8, 95% CI 1.2–2.8 p=0.01). All estimates were based on time dependent Cox models and landmark analyses at 9 months. EBMT score was higher in the RIC group (score 0–2, 27% vs 52% p<0.001) and was associated with 5-year survival estimates: EBMT score 0–2, 68% vs 68%, 3–4, 48% vs 56% and 5–7, 27% vs 33% for RIC and MAC respectively. Comparison of RIC and MAC is complicated by differences in patient characteristics. A propensity score was developed to adjust for these differences from a logistic regression model based on the following factors: age, use of PBSC, T cell depletion, disease phase, year, CMV status, sex mismatch, time to transplant and donor type. The propensity score predicts the likelihood of receiving a RIC (high score, RIC more likely). Adjusting for the propensity score compensates for the differences in the underlying covariates. Forty nine percent of RIC allografts were performed in centres reporting ≥5 RIC transplants. There was a significant interaction between propensity score, a centre’s RIC-activity and conditioning intensity on survival. Excluding centres not performing RIC to avoid bias and adjusting for propensity score, survival >9 months was worse in RIC patients with a low propensity score when treated in centres with <5 RICS (HR 2.4 CI 1.3–4.4) whereas survival >9 months was equal in centres treating ≥5 patients with RIC who had a high propensity score (HR 0.8 CI 0.4–1.6). The figures below illustrate this showing the cumulative risk of non-relapse mortality, relapse and death after relapse for these groups estimated in a competing risk setting.
Conclusion: Transplant centre experience and patient selection impact on outcome. Survival with RIC HSCT is inferior to MAC except for the subgroup of patients with a high propensity score transplanted at centres with ≥5 RIC HSCT.
Low Propensity Score and <5 RIC HSCT
High propensity Score and ≥5 RIC HSCT
Author notes
Disclosure:Membership Information: AG has an advisory role for Novartis and BMS.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal