Abstract
Eradication of Helicobacter pylori may lead to improvement of chronic immune thrombocytopenic purpura (ITP), although its efficacy over time is uncertain. We report the results of H pylori screening and eradication in 75 consecutive adult patients with ITP. We also used molecular methods to investigate lymphocyte clonality and H pylori genotypes in the gastric biopsies from 10 H pylori–positive patients with ITP and 19 H pylori–positive patients without ITP with chronic gastritis. Active H pylori infection was documented in 38 (51%) patients and successfully eradicated in 34 (89%) patients. After a median follow-up of 60 months, a persistent platelet response in 23 (68%) of patients with eradicated infection was observed; 1 relapse occurred. No differences in mucosal B- or T-cell clonalities were observed between patients with ITP and control participants. Of note, the frequency of the H pylori cagA gene (P = .02) and the frequency of concomitant H pylori cagA, vacAs1, and iceA genes (triple-positive strains; P = .015) resulted statistically higher in patients with ITP than in control participants. All asymptomatic H pylori–positive patients with ITP were suffering from chronic gastritis. Our data suggest a sustained platelet recovery in a proportion of patients with ITP by H pylori eradication alone. Overrepresentation of specific H pylori genotypes in ITP suggests a possible role for bacterium-related factors in the disease pathogenesis.
Introduction
The Gram-negative bacterium Helicobacter pylori is widely known as a causative agent of gastritis and peptic ulcers and as a high-risk factor for the development of gastric cancer and mucosa-associated lymphoid tissue lymphoma.1 The bacterium infection has also been implicated in the pathogenesis of extradigestive diseases, such as coronary heart disease, acne rosacea, idiopathic chronic urticaria, and also autoimmune diseases such as rheumatoid arthritis, autoimmune thyroiditis, Sjoegren syndrome, and Schoenlein-Henoch purpura.2 Moreover, in the last few years, several studies, primarily from Italy and Japan, found that the eradication of H pylori in infected patients with chronic immune thrombocytopenic purpura (ITP) leads to a substantial and persistent increase of platelet count in more than half of treated patients.3-17
The pathogenetic mechanisms underlying the relationship between H pylori infection and ITP are still to be elucidated, but some data suggest that the effect of bacterium eradication may depend on either genetic factors of the host, country-related factors, or H pylori strains.18
The real usefulness of bacterium eradication in ITP over time may be debatable, due to the limited duration of follow-up in most of the studies performed so far. To address this issue, we report the results of a 60-month follow-up of a study in 75 patients with ITP from a single center to conclude whether H pylori eradication may be an effective and long-term cure in chronic ITP. The second aim of the study is to give insights into the pathogenesis by investigating, in a selected group of patients, the possible association between either B- and T-cell clonality or specific H pylori strains and H pylori–associated ITP.
Patients and methods
Patients
Between January 1999 and December 2004, we enrolled 75 consecutive patients with adult chronic ITP: 33 men, 42 women with a median age of 56 years (range, 18-91 years). All but 2 patients were white, and came from Northern Italy; 93.3% were from Emilia-Romagna region, and 77.3% were from the province of Modena.
ITP was defined following the guidelines of the American Society of Hematology19 : idiopathic thrombocytopenia (platelets < 100 × 109/L) persistent for more than 6 months, with normal or increased megakaryocytosis in the bone marrow (patients more than 60 years old), and when other causes had been excluded, such as hepatits C virus (HCV) and HIV infections, drugs, lymphoproliferative disorders, other autoimmune diseases, and pseudothrombocytopenia.
Active H pylori infection was assessed by 13C urea breath test (UBT; Helicobacter test; Infai, Bochum, Germany) in all patients and, whenever possible, by histologic examination (Giemsa stain) of specimens obtained by an upper gastrointestinal endoscopy (22 patients; 29.3%). All immunosuppressive treatments and proton pump inhibitors were withdrawn at least 1 month before eradication. Bacterial eradication was performed with standard therapy: amoxicillin (1000 mg twice daily), clarithromycin (250 mg 3 times daily), and a proton-pump inhibitor (20 or 40 mg twice daily) for 1 week. Eradication was assessed by UBT 4 to 6 weeks after treatment withdrawal. Platelet counts were monitored every 2 weeks for the first 2 months, every month for the next 4 months and then every 6 months, after the end of treatment. A complete response (CR) was defined as a platelet count in the normal range for at least 3 months after eradication treatment. A partial response (PR) was defined as a platelet count not higher than 149 × 109/L or a doubling of initial value rising higher than 40 × 109/L. No response (NR) was defined as a platelet count that did not rise higher than 40 × 109/L, even if it was a doubling of initial value. The eradication treatment was also administered to 5 patients with ITP without H pylori infection, as control participants.
Biopsy and histology of the gastric mucosa
A total of 10 patients with ITP, with UBT positivity and without gastrointestinal symptoms, underwent upper gastrointestinal endoscopy; 2 distinct biopsy specimens were obtained from the corpus and antrum of the stomach. One fragment of each was placed in a sterile Eppendorf tube and stored at −80°C until DNA extraction; the second was fixed in 10% formalin and sent for routine histologic examination. Gastric biopsy specimens were also obtained from 35 patients without ITP with gastrointestinal symptoms who underwent the standard gastroscopy procedure and formed the control group. All paraffin-embedded tissue sections were stained with hematoxylin and eosin to detect gastric alterations and with Giemsa stain to detect H pylori.
For each patient of both groups, we evaluated the possible gastric mucosal B- and T-cell clonality and the presence of H pylori virulence factors: cagA (cytotoxin-associated gene A), vacA (vacuolating cytotoxin gene A) with s1, s2 (signal region) and m1, m2 (middle region) genotypes, iceA (induced by contact with epithelium gene; A1 and A2) and babA2 (blood group antigen-binding adhesin gene).
DNA extraction
Frozen gastric biopsy specimens were homogenized with a sterile micropestle, and the genomic DNA was extracted using Easy-DNA kit (Invitrogen, Carlsbad, CA) in accordance with the manufacturer's instructions and stored at −20°C. Genomic DNA was also extracted from two 5-μm-thick paraffin wax–embedded sections, when frozen biopsy samples were not available, using the QIAamp DNA mini kit (tissue protocol; Qiagen, Valencia, CA) and stored at −20°C.
Primers and PCR design
The detection of the H pylori cagA (in the middle conservative region), signal regions s1 and s2 and middle regions m1 and m2 of the vacA and iceA variants iceA1 and iceA2 and babA2 genes was done by polymerase chain reaction (PCR) using established primers.20-24
PCR reactions were performed in a reaction volume of 50 μL containing 1 × GeneAmp PCR Buffer (10 mM Tris-HCl [pH 8.3], 50 mM KCl, and 1.5 mM MgCl2; Applied Biosystems, Foster City, CA), 225 μM dNTPs (Amersham Biosciences, Arlington Heights, IL), 0.5 μM of each primer, 2 U AmpliTaq Gold (Applied Biosystems), 10% glycerol for iceA, and 1 μg DNA. Negative and positive controls were assayed in each test.
A previous study25 revealed that the vacA midregion type was detected by PCR in only about 70% of the patients when the primers vac3R and vac4F were used. Therefore, these primers were substituted by primers vac3R* and vac4F*22 and additionally used in negative cases for vacA m1 or m2.
The PCR amplification was performed under the following conditions: initial denaturation at 95°C for 10 minutes, followed by 35 cycles (40 cycles for babA2) of denaturation at 95°C for 1 minute, annealing for 1 minute, extension for 1 minute at 72°C (1.5 minutes at 72°C for babA2), and a final extension at 72°C for 10 minutes. Annealing temperatures were set at 55°C for cagA primers, at 52°C for vacA (va1F-va1R, vac3F-vac3R, vac4F-vac4R), and at 50°C for vacA (vac3F-vac3R*, vac4F*-vac4R), iceA, and babA2 primer sets.
IgH gene rearrangement
Analysis of IgH gene rearrangement was carried out as a seminested PCR according to 2 different previously described protocols.26
TCRγ gene rearrangement
Analysis of T-cell receptor γ (TCRγ) gene rearrangement was performed using 2 mixtures of primers for the various V and J segments by a single round of amplification as previously published,27 but with some modifications in PCR reaction conditions. Briefly, PCRs were performed using 2.5 U AmpliTaq Gold DNA polymerase in a 50-μL reaction that contained 1 × GeneAmp PCR Buffer, 1.5 mM MgCl2, 200 μM dNTPs, 300 ng of each primer, and 0.5 μg DNA under the following conditions: 10 minutes at 95°C, 45 cycles of 95°C for 1 minute, 55°C for 1 minute, 72°C for 1 minute, and final extension step for 10 minutes at 72°C.
A total of 20 μL of each PCR product was visualized by electrophoresis on 2% to 3% agarose gel stained with ethidium bromide under UV light and photographed (Gel Doc 2000; Bio-Rad, Hercules, CA).
In statistical analysis, data were expressed as the mean (SD) or median (range) as appropriate and were analyzed by using the t test. Percentages were compared by chi-square test (Fisher exact test for values < 5). A P value less than .05 was considered statistically significant. Disease-free survival was estimated using the Kaplan-Meier method. The statistical software used for the analyses was STATA/SE version 8.0 for Windows (Stata Corp, College Station, TX).
The study protocol was approved by the Provincial Ethical Committee of Modena, and an informed consent from all patients was obtained in accordance with the Declaration of Helsinki.
A second, separate consent was obtained from the patients with UBT positivity to allow gastric biopsy. The research aim of the procedure has been clarified. In the 5 patients with platelet counts less than 30 × 109/L, a 4-day course of intravenous immunoglobulin (IVIg) was administered. In these patients, gastric biopsy was performed when platelet counts reached 50 × 109/L, while eradication treatment was initiated when platelet counts decreased to lower than 30 × 109/L, which usually occurred after 1 month. No bleeding was noted in any patient.
Results
The clinical data concerning the 75 patients are shown in Tables 1,Table 2–3. Demographics of the first enrolled 37 patients, already reported elsewhere,4,5 as well as of the last enrolled 38 patients are shown in Table 2. On the whole, 22 (30%) patients entered the study at diagnosis of chronic ITP (7-9 months of persistent thrombocytopenia), while the remaining 53 (70%) have been previously diagnosed. A total of 52 percent of the patients have had previous treatment for ITP: all but 2 treated patients received steroids (often intermittently); 3 patients also received vincristine, 4 received cyclophosphamide, 7 received IVIg, 2 received cyclosporine, and 4 underwent splenectomy; 24 (61%) of 39 previously treated patients were refractory or dependent on steroid administration; 1 patient was also refractory to splenectomy.
H pylori infection and ITP: our series
| Time . | No. of patients† . | Infected, no. (%) . | Eradicated, no. (%) . | Responders, no. (%) . | CR/PR/NR, no. . | Median follow-up, mo (range) . | Reference . |
|---|---|---|---|---|---|---|---|
| 2001 | 30 | 13 (43) | 12 (92) | 6 (50)* | 4/2/6 | 81 | Emilia et al4 |
| 2002 | 7 | 3 (43) | 3 (100) | 2 (66) | 2/0/1 | 67 | Emilia et al5 |
| 2002-2004 | 38 | 22 (58) | 19 (86) | 15 (79)† | 10/5/5 | 32 (18-46) | Present report |
| Total | 75 | 38 (51) | 34 (89) | 23 (68) | 16/7/12 | 60 (18-90) | — |
| Time . | No. of patients† . | Infected, no. (%) . | Eradicated, no. (%) . | Responders, no. (%) . | CR/PR/NR, no. . | Median follow-up, mo (range) . | Reference . |
|---|---|---|---|---|---|---|---|
| 2001 | 30 | 13 (43) | 12 (92) | 6 (50)* | 4/2/6 | 81 | Emilia et al4 |
| 2002 | 7 | 3 (43) | 3 (100) | 2 (66) | 2/0/1 | 67 | Emilia et al5 |
| 2002-2004 | 38 | 22 (58) | 19 (86) | 15 (79)† | 10/5/5 | 32 (18-46) | Present report |
| Total | 75 | 38 (51) | 34 (89) | 23 (68) | 16/7/12 | 60 (18-90) | — |
Number of men, 33; women, 42. Median age, 56 y (range, 18-91 y). A total of 14 patients had platelet counts lower than 30 × 109/L. A total of 10 (71%) showed response (1 relapse at 7 months). A total of 2 patients died from nonhematologic diseases. CR indicates complete response; PR, partial response; NR, no response; and —, not applicable.
1 relapse 7 months after eradication.
1 patient resistant to eradication, achieved response during follow-up.
Patient demographics
| Patient no. . | Age in y, sex . | Disease duration, mo. . | Previous therapy . | H pylori infection . | Platelets, × 109/L . | Follow-up, mo . | Present condition . | |
|---|---|---|---|---|---|---|---|---|
| Before . | After (at 6 mo) . | |||||||
| Previously reported patients | ||||||||
| 1 | 52, M | 16 | None | Yes | 80 | 67 | 90 | NR-stable |
| 2 | 58, F | 15 | None | Yes | 80 | 111 | 87 | NR-stable |
| 3 | 63, M | 14 | None | Yes | 52 | 68 | 86 | NR-stable |
| 4 | 60, F | 16 | P | Yes | 30 | 31 | 86 | NR-P |
| 5 | 67, M | 46 | None | Yes | 50 | 126* | 85 | PR |
| 6 | 79, F | 70 | P, V | Yes | 33 | 220* | 83 | CR |
| 7 | 60, M | 15 | P | Yes | 25 | 176* | 80 | CR |
| 8 | 61, M | 39 | P | Yes | 80 | 76 | 80 | NR-stable |
| 9 | 75, M | 20 | None | Yes | 80 | 84 | 80 | NR-stable |
| 10 | 77, F | 21 | P | Yes | 27 | 172* | 79 | CR† |
| 11 | 33, M | 35 | P,Sple | Yes | 80 | 371* | 79 | CR |
| 12 | 89, M | 13 | P | Yes | 15 | 35 | 34 | NR-lost |
| 13 | 48, F | 53 | P | Yes | 50 | 125* | 78 | PR |
| 14 | 70, F | 110 | Ig,Cy | No | 37 | 80 | 88 | Stable |
| 15 | 79, M | 65 | P | No | 41 | 130 | 87 | Stable |
| 16 | 36, M | 52 | P,V | No | 30 | 110 | 87 | Stable |
| 17 | 19, F | 19 | None | No | 62 | 58 | 86 | Stable |
| 18 | 18, F | 18 | None | No | 58 | 70 | 85 | Stable |
| 19 | 20, F | 29 | P | No | 38 | 120 | 83 | Stable |
| 20 | 53, F | 64 | P,Ig,C | No | 35 | 80 | 83 | Stable |
| 21 | 55, F | 84 | P,C,V | No | 32 | 90 | 83 | Stable |
| 22 | 39, F | 34 | P | No | 43 | 100 | 82 | Stable |
| 23 | 26, F | 15 | P | No | 65 | 150 | 80 | Stable |
| 24 | 64, M | 79 | Ig,P | No | 45 | 130 | 80 | Stable |
| 25 | 64, M | 31 | P,C,Sple | No | 2 | 120 | 81 | Stable |
| 26 | 66, M | 23 | P | No | 40 | 140 | 79 | Stable |
| 27 | 49, F | 32 | Ig,Sple | No | 35 | 130 | 79 | Stable |
| 28 | 26, F | 21 | P | No | 40 | 140 | 79 | Stable |
| 29 | 35, F | 18 | P | No | 42 | 130 | 79 | Stable |
| 30 | 68, F | 120 | P,Sple,Cy | No | 40 | 115 | 79 | Stable |
| 31 | 66, M | 11 | P,C | Yes | 38 | 50 | 70 | NR-stable |
| 32 | 41, F | 12 | P | Yes | 38 | 160* | 68 | CR |
| 33 | 18, F | 10 | None | Yes | 46 | 180* | 66 | CR |
| 34 | 62, M | 12 | None | No | 48 | 50 | 72 | Stable |
| 35 | 38, M | 10 | None | No | 46 | 145 | 65 | Stable |
| 36 | 46, F | 12 | None | No | 42 | 190 | 64 | Stable |
| 37 | 58, M | 10 | None | No | 43 | 185 | 64 | Stable |
| Last enrolled patients | ||||||||
| 38 | 69, M | 7 | P | Yes | 29 | 190* | 46 | CR |
| 39 | 83, M | 10 | None | Yes | 43 | 170* | 45 | CR |
| 40 | 24, F | 9 | None | Yes | 50 | 180* | 45 | CR |
| 41 | 78, M | 7 | P | Yes | 10 | 20 | 44 | NR-P |
| 42 | 30, F | 12 | P | Yes | 34 | 38 | 43 | NR-sple |
| 43 | 52, M | 16 | None | Yes | 45 | 100* | 43 | PR |
| 44 | 85, F | 9 | P | Yes | 12 | 195* | 23 | CR‡ |
| 45 | 69, F | 7 | P | Yes | 50 | 163* | 43 | CR |
| 46 | 18, F | 9 | Ig/P | Yes | 9 | 22 | 41 | NR-P |
| 47 | 47, M | 186 | Ig/P | Yes | 6 | 173* | 39 | CR |
| 48 | 27, M | 7 | None | Yes | 80 | 120* | 39 | PR |
| 49 | 37, M | 18 | None | Yes§ | 25 | 99*¶ | 32 | PR |
| 50 | 37, M | 14 | P | Yes | 27 | 246* | 31 | CR |
| 51 | 73, F | 18 | None | Yes | 60 | 75 | 30 | NR-P |
| 52 | 77, M | 7 | None | Yes | 70 | 120* | 28 | PR |
| 53 | 26, F | 7 | P | Yes | 2 | 485* | 28 | CR |
| 54 | 52, F | 7 | Ig/P | Yes | 20 | 235* | 26 | CR |
| 55 | 77, F | 21 | P | Yes | 18 | 187* | 26 | CR |
| 56 | 77, F | 12 | P | Yes | 65 | 120* | 25 | PR |
| 57 | 70, F | 7 | P | Yes | 31 | 40 | 21 | NR-P |
| 58 | 45, F | 10 | None | Yes§ | 50 | 60 | 21 | NR-stable |
| 59 | 34, M | 7 | P | Yes§ | 1 | 12 | 18 | NR-P |
| 60 | 57, M | 7 | None | No | 1 | 113 | 41 | P |
| 61 | 68, M | 9 | None | No | 15 | 95 | 39 | P |
| 62 | 81, F | 12 | None | No | 5 | 248 | 34 | Stable |
| 63 | 46, M | 8 | None | No | 50 | 60 | 33 | Stable |
| 64 | 82, F | 19 | None | No | 78 | 70 | 32 | Stable |
| 65 | 36, F | 8 | None | No | 25 | 100 | 32 | P-stable |
| 66 | 26, M | 7 | None | No | 24 | 115 | 31 | P |
| 67 | 38, F | 12 | None | No | 50 | 48 | 31 | Stable |
| 68 | 85, F | 8 | None | No | 20 | 80 | 29 | Dead |
| 69 | 42, M | 16 | None | No | 60 | 55 | 28 | Stable |
| 70 | 35, M | 14 | None | No | 70 | 60 | 28 | Stable |
| 71 | 91, F | 10 | None | No | 25 | 90 | 27 | P-stable |
| 72 | 24, M | 8 | None | No | 12 | 85 | 25 | P |
| 73 | 47, M | 7 | None | No | 25 | 90 | 19 | P-stable |
| 74 | 48, M | 7 | None | No | 45 | 50 | 18 | Stable |
| 75 | 26, F | 7 | None | No | 40 | 48 | 18 | Stable |
| Patient no. . | Age in y, sex . | Disease duration, mo. . | Previous therapy . | H pylori infection . | Platelets, × 109/L . | Follow-up, mo . | Present condition . | |
|---|---|---|---|---|---|---|---|---|
| Before . | After (at 6 mo) . | |||||||
| Previously reported patients | ||||||||
| 1 | 52, M | 16 | None | Yes | 80 | 67 | 90 | NR-stable |
| 2 | 58, F | 15 | None | Yes | 80 | 111 | 87 | NR-stable |
| 3 | 63, M | 14 | None | Yes | 52 | 68 | 86 | NR-stable |
| 4 | 60, F | 16 | P | Yes | 30 | 31 | 86 | NR-P |
| 5 | 67, M | 46 | None | Yes | 50 | 126* | 85 | PR |
| 6 | 79, F | 70 | P, V | Yes | 33 | 220* | 83 | CR |
| 7 | 60, M | 15 | P | Yes | 25 | 176* | 80 | CR |
| 8 | 61, M | 39 | P | Yes | 80 | 76 | 80 | NR-stable |
| 9 | 75, M | 20 | None | Yes | 80 | 84 | 80 | NR-stable |
| 10 | 77, F | 21 | P | Yes | 27 | 172* | 79 | CR† |
| 11 | 33, M | 35 | P,Sple | Yes | 80 | 371* | 79 | CR |
| 12 | 89, M | 13 | P | Yes | 15 | 35 | 34 | NR-lost |
| 13 | 48, F | 53 | P | Yes | 50 | 125* | 78 | PR |
| 14 | 70, F | 110 | Ig,Cy | No | 37 | 80 | 88 | Stable |
| 15 | 79, M | 65 | P | No | 41 | 130 | 87 | Stable |
| 16 | 36, M | 52 | P,V | No | 30 | 110 | 87 | Stable |
| 17 | 19, F | 19 | None | No | 62 | 58 | 86 | Stable |
| 18 | 18, F | 18 | None | No | 58 | 70 | 85 | Stable |
| 19 | 20, F | 29 | P | No | 38 | 120 | 83 | Stable |
| 20 | 53, F | 64 | P,Ig,C | No | 35 | 80 | 83 | Stable |
| 21 | 55, F | 84 | P,C,V | No | 32 | 90 | 83 | Stable |
| 22 | 39, F | 34 | P | No | 43 | 100 | 82 | Stable |
| 23 | 26, F | 15 | P | No | 65 | 150 | 80 | Stable |
| 24 | 64, M | 79 | Ig,P | No | 45 | 130 | 80 | Stable |
| 25 | 64, M | 31 | P,C,Sple | No | 2 | 120 | 81 | Stable |
| 26 | 66, M | 23 | P | No | 40 | 140 | 79 | Stable |
| 27 | 49, F | 32 | Ig,Sple | No | 35 | 130 | 79 | Stable |
| 28 | 26, F | 21 | P | No | 40 | 140 | 79 | Stable |
| 29 | 35, F | 18 | P | No | 42 | 130 | 79 | Stable |
| 30 | 68, F | 120 | P,Sple,Cy | No | 40 | 115 | 79 | Stable |
| 31 | 66, M | 11 | P,C | Yes | 38 | 50 | 70 | NR-stable |
| 32 | 41, F | 12 | P | Yes | 38 | 160* | 68 | CR |
| 33 | 18, F | 10 | None | Yes | 46 | 180* | 66 | CR |
| 34 | 62, M | 12 | None | No | 48 | 50 | 72 | Stable |
| 35 | 38, M | 10 | None | No | 46 | 145 | 65 | Stable |
| 36 | 46, F | 12 | None | No | 42 | 190 | 64 | Stable |
| 37 | 58, M | 10 | None | No | 43 | 185 | 64 | Stable |
| Last enrolled patients | ||||||||
| 38 | 69, M | 7 | P | Yes | 29 | 190* | 46 | CR |
| 39 | 83, M | 10 | None | Yes | 43 | 170* | 45 | CR |
| 40 | 24, F | 9 | None | Yes | 50 | 180* | 45 | CR |
| 41 | 78, M | 7 | P | Yes | 10 | 20 | 44 | NR-P |
| 42 | 30, F | 12 | P | Yes | 34 | 38 | 43 | NR-sple |
| 43 | 52, M | 16 | None | Yes | 45 | 100* | 43 | PR |
| 44 | 85, F | 9 | P | Yes | 12 | 195* | 23 | CR‡ |
| 45 | 69, F | 7 | P | Yes | 50 | 163* | 43 | CR |
| 46 | 18, F | 9 | Ig/P | Yes | 9 | 22 | 41 | NR-P |
| 47 | 47, M | 186 | Ig/P | Yes | 6 | 173* | 39 | CR |
| 48 | 27, M | 7 | None | Yes | 80 | 120* | 39 | PR |
| 49 | 37, M | 18 | None | Yes§ | 25 | 99*¶ | 32 | PR |
| 50 | 37, M | 14 | P | Yes | 27 | 246* | 31 | CR |
| 51 | 73, F | 18 | None | Yes | 60 | 75 | 30 | NR-P |
| 52 | 77, M | 7 | None | Yes | 70 | 120* | 28 | PR |
| 53 | 26, F | 7 | P | Yes | 2 | 485* | 28 | CR |
| 54 | 52, F | 7 | Ig/P | Yes | 20 | 235* | 26 | CR |
| 55 | 77, F | 21 | P | Yes | 18 | 187* | 26 | CR |
| 56 | 77, F | 12 | P | Yes | 65 | 120* | 25 | PR |
| 57 | 70, F | 7 | P | Yes | 31 | 40 | 21 | NR-P |
| 58 | 45, F | 10 | None | Yes§ | 50 | 60 | 21 | NR-stable |
| 59 | 34, M | 7 | P | Yes§ | 1 | 12 | 18 | NR-P |
| 60 | 57, M | 7 | None | No | 1 | 113 | 41 | P |
| 61 | 68, M | 9 | None | No | 15 | 95 | 39 | P |
| 62 | 81, F | 12 | None | No | 5 | 248 | 34 | Stable |
| 63 | 46, M | 8 | None | No | 50 | 60 | 33 | Stable |
| 64 | 82, F | 19 | None | No | 78 | 70 | 32 | Stable |
| 65 | 36, F | 8 | None | No | 25 | 100 | 32 | P-stable |
| 66 | 26, M | 7 | None | No | 24 | 115 | 31 | P |
| 67 | 38, F | 12 | None | No | 50 | 48 | 31 | Stable |
| 68 | 85, F | 8 | None | No | 20 | 80 | 29 | Dead |
| 69 | 42, M | 16 | None | No | 60 | 55 | 28 | Stable |
| 70 | 35, M | 14 | None | No | 70 | 60 | 28 | Stable |
| 71 | 91, F | 10 | None | No | 25 | 90 | 27 | P-stable |
| 72 | 24, M | 8 | None | No | 12 | 85 | 25 | P |
| 73 | 47, M | 7 | None | No | 25 | 90 | 19 | P-stable |
| 74 | 48, M | 7 | None | No | 45 | 50 | 18 | Stable |
| 75 | 26, F | 7 | None | No | 40 | 48 | 18 | Stable |
Of the previously reported patients, nos. 1-30 are from Emilia et al;4 nos. 31-37 are from Emilia et al.5 For uninfected patients, platelet values are before and after immunosuppressive therapy.
P indicates prednisone; C, cyclosphosphamide; Cy, cyclosporine; V, vincristine; Ig, intravenous immunoglobulin; sple, splenectomy; CR, complete response; PR, partial response; and NR, no response.
Eradication-responsive patients.
Patient relapsed 7 months after eradication; at present, the patient is in CR with intermittent prednisone.
Died from heart failure.
Eradication failed after at least 2 regimens, including metronidazole.
Patient achieved response during follow-up.
Response to H pylori eradication treatment in patients with platelets less then 30 × 109/L
| Patient no. . | Age in y, sex . | Duration, mo . | H pylori infection . | Platelets, × 109/L . | Follow-up, mo. . | Present condition . | |
|---|---|---|---|---|---|---|---|
| Before . | After (at 6 mo) . | ||||||
| 1 | 69, M | 7 | Yes | 29 | 190* | 46 | CR |
| 10 | 77, F | 21 | Yes | 27 | 172* | 79 | CR† |
| 50 | 37, M | 14 | Yes | 27 | 246* | 31 | CR |
| 7 | 60, M | 15 | Yes | 25 | 176* | 80 | CR |
| 49 | 37, M | 18 | Yes | 25 | 99* | 32 | PR |
| 54 | 52, F | 7 | Yes | 20 | 235* | 26 | CR |
| 55 | 77, F | 21 | Yes | 18 | 187* | 26 | CR |
| 12 | 89, M | 13 | Yes | 15 | 35 | 34 | NR‡ |
| 44 | 85, F | 9 | Yes | 12 | 195* | 23 | Died in CR |
| 41 | 78, M | 7 | Yes | 10 | 20 | 44 | NR-P |
| 46 | 18, F | 9 | Yes | 9 | 22 | 41 | NR-P |
| 47 | 47, M | 186 | Yes | 6 | 173* | 39 | CR |
| 53 | 26, F | 7 | Yes | 2 | 485* | 28 | CR |
| 59 | 34, M | 7 | Yes | 1 | 12 | 18 | NR-P |
| 65 | 36, F | 8 | No | 25 | 100 | 32 | P-stable |
| 71 | 91, F | 9 | No | 25 | 90 | 27 | P-stable |
| 73 | 47, M | 7 | No | 25 | 90 | 19 | P-stable |
| 66 | 26, M | 7 | No | 24 | 115 | 31 | P |
| 68 | 85, F | 8 | No | 20 | 80 | 29 | Dead |
| 61 | 68, M | 9 | No | 15 | 95 | 39 | P |
| 72 | 24, M | 8 | No | 12 | 85 | 25 | P-stable |
| 62 | 81, F | 12 | No | 5 | 248 | 34 | Stable |
| 25 | 64, M | 31 | No | 2 | 120 | 81 | Stable |
| 60 | 57, M | 7 | No | 1 | 113 | 41 | P |
| Patient no. . | Age in y, sex . | Duration, mo . | H pylori infection . | Platelets, × 109/L . | Follow-up, mo. . | Present condition . | |
|---|---|---|---|---|---|---|---|
| Before . | After (at 6 mo) . | ||||||
| 1 | 69, M | 7 | Yes | 29 | 190* | 46 | CR |
| 10 | 77, F | 21 | Yes | 27 | 172* | 79 | CR† |
| 50 | 37, M | 14 | Yes | 27 | 246* | 31 | CR |
| 7 | 60, M | 15 | Yes | 25 | 176* | 80 | CR |
| 49 | 37, M | 18 | Yes | 25 | 99* | 32 | PR |
| 54 | 52, F | 7 | Yes | 20 | 235* | 26 | CR |
| 55 | 77, F | 21 | Yes | 18 | 187* | 26 | CR |
| 12 | 89, M | 13 | Yes | 15 | 35 | 34 | NR‡ |
| 44 | 85, F | 9 | Yes | 12 | 195* | 23 | Died in CR |
| 41 | 78, M | 7 | Yes | 10 | 20 | 44 | NR-P |
| 46 | 18, F | 9 | Yes | 9 | 22 | 41 | NR-P |
| 47 | 47, M | 186 | Yes | 6 | 173* | 39 | CR |
| 53 | 26, F | 7 | Yes | 2 | 485* | 28 | CR |
| 59 | 34, M | 7 | Yes | 1 | 12 | 18 | NR-P |
| 65 | 36, F | 8 | No | 25 | 100 | 32 | P-stable |
| 71 | 91, F | 9 | No | 25 | 90 | 27 | P-stable |
| 73 | 47, M | 7 | No | 25 | 90 | 19 | P-stable |
| 66 | 26, M | 7 | No | 24 | 115 | 31 | P |
| 68 | 85, F | 8 | No | 20 | 80 | 29 | Dead |
| 61 | 68, M | 9 | No | 15 | 95 | 39 | P |
| 72 | 24, M | 8 | No | 12 | 85 | 25 | P-stable |
| 62 | 81, F | 12 | No | 5 | 248 | 34 | Stable |
| 25 | 64, M | 31 | No | 2 | 120 | 81 | Stable |
| 60 | 57, M | 7 | No | 1 | 113 | 41 | P |
Data represent patients with ITP with platelet counts less than 30 × 109/L. Disease duration data from Table 2. For uninfected patients, platelet values are before and after immunosuppressive therapy.
P indicates intermittent prednisone.
Eradication-responsive patients.
Relapse 7 months after eradication.
Lost follow-up.
H pylori infection was found in 38 (51%) patients. No differences in the prevalence of infection were noted between infected men (19 infected vs 17 uninfected) and women (19 infected vs 20 uninfected). The median age of infected patients was 58 years (± 19 years), while the median age for uninfected patients was 49.9 years (± 20.7 years; P = .082). The baseline platelet count was similar in infected and uninfected patients (40.6 × 109/L [± 25.0 × 109/L] vs 37.2 × 109/L [± 18.6 × 109/L]; P = .507). A total of 14 (37%) of 38 patients infected with H pylori showed, at diagnosis, a severe form of ITP (platelet count less than 30 × 109/L). Eradication of the bacterium has been obtained in 34 (89%) infected patients, of which 18 (53%) were younger than 65 years, while 16 (47%) were older than 65 years (P = .387).
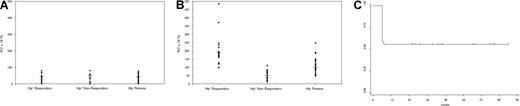
The median platelet count follow-up time (calculated from the date of registration to either June 31, 2006, or the date of death or loss of follow-up) was 60 months (range, 18-81 months). Only 2 non-ITP–related deaths occurred, caused by heart failure. At the end of follow-up, 23 (68%) of the 34 patients with eradicated infection had a significant and persistent increase in platelet count (95% confidence interval [CI] = 48%-81%); 1 patient refractory to eradication treatment showed response during follow-up (Tables 1,2); and 16 (46%) patients achieved CR (95% CI = 29%-73%), while 7 (20%) patients achieved PR (95% CI = 8%-37%) and 12 (34%) were nonresponders (95% CI = 19%-52%). The response rate was 40% (4 of 10 patients; 1 CR and 3 PR) in patients with baseline platelet counts greater than 50 × 109/L; 64% (9 of 14 patients; 6 CR and 3 PR) in patients with platelet counts between 50 and 30 × 109/L, and 71% (10 of 14 patients; 9 CR and 1 PR) in patients with platelet counts less than 30 × 109/L. Further details of disease duration and response in this latter patient group are shown in Table 3. All of the 6 patients with platelet counts between 29 and 20 × 109/L were responders (CR = 83%); 50% of the 4 patients with platelet counts between 19 and 10 × 109/L and 50% of 4 patients with platelet counts between 9 and 1 × 109/L were responders, and achieved CR. All of the 10 uninfected patients with platelet counts less than 30 × 109/L were responsive to immunosuppressive treatment (Table 3). The initial platelet count improvement was usually observed 2 weeks after completion of eradication therapy, with assessment at 6 months (Figure 1A,B). Disease-free survival analysis of H pylori–positive patients with ITP (responders and nonresponders to eradication treatment) showed that 55% of patients are disease free both at 7 and 60 months (95% CI = 38.3-69.3), with no late relapses (Figure 1C). No significant differences in the platelet response were noted in respect to sex and age: 11 of 17 men and 12 of 18 women were responders; 12 (52%) patients aged 65 years and younger and 11 (48%) patients older than 65 years showed a response (CR, 8 and 8, respectively; PR, 4 and 3, respectively; P = .505). Responders were not younger than nonresponders (59 ± 19 years vs 61 ± 19 years; P = .497), and had neither a higher baseline platelet count (39 ± 23 × 109/L vs 46 ± 24 × 109/L; P = .402) nor a shorter disease duration (21 ± 39 months vs 10 ± 11 months; P = .368). Among 23 responder patients, 15 (65%) had received prior therapy (including prednisone, immunoglobulin [2 patients], vincristine [1patient], and splenectomy [1 patient]) versus 9 (60%) of 15 nonresponders (P = .307).
Comparison of platelet counts between patient groups; disease-free survival in infected patients. (A) Platelet (PLT) count of H pylori–positive patients with ITP, both responders and nonresponders to eradication, and H pylori–negative patients with ITP, at baseline. Black lines represent the median platelet value. ● represents single patient platelet values. (B) Platelet (PLT) count of H pylori–positive patients with ITP, both responders and nonresponders to eradication, and H pylori–negative patients with ITP, at 6 months. Black lines represent the median platelet value. ● represents single patient platelet values. (C) Disease-free survival analysis of H pylori–positive patients measured by the Kaplan-Meier method. A total of 55 percent of patients are disease free both at 7 and 60 months (95% CI = 38.3-69.3).
Comparison of platelet counts between patient groups; disease-free survival in infected patients. (A) Platelet (PLT) count of H pylori–positive patients with ITP, both responders and nonresponders to eradication, and H pylori–negative patients with ITP, at baseline. Black lines represent the median platelet value. ● represents single patient platelet values. (B) Platelet (PLT) count of H pylori–positive patients with ITP, both responders and nonresponders to eradication, and H pylori–negative patients with ITP, at 6 months. Black lines represent the median platelet value. ● represents single patient platelet values. (C) Disease-free survival analysis of H pylori–positive patients measured by the Kaplan-Meier method. A total of 55 percent of patients are disease free both at 7 and 60 months (95% CI = 38.3-69.3).
The ITP recurred in only 1 patient 7 months after eradication, although the UBT remained negative. In 3 of 4 patients in whom eradication failed, the platelet count remained unchanged during follow-up; 1 patient (no. 49) achieved response during the follow-up (about 10 months after the third-line regimen, including metronidazole) without any further treatment. At the end of follow-up, all living patients were in good condition. No side effects after eradication treatment were noted in any patient. No platelet response was observed in any H pylori–negative patients in whom eradication therapy had been administered.
Among the 37 H pylori–negative patients, the platelet count remained substantially unchanged during follow-up in the 10 patients not requiring therapy; immunosuppressive treatment (prednisone and IVIg, or cyclophosphamide or vincristine) was often intermittently administered in the remaining 27 patients, including 10 patients with platelet counts less than 30 × 109/L, allowing CR in 4 patients and a PR in 23 patients (Table 2).
At histologic examination, all 10 clinically asymptomatic patients with ITP were confirmed to be infected with H pylori and were found to be suffering from chronic and/or atrophic gastritis. Of 35 clinically symptomatic patients without ITP, 23 were found to be infected with H pylori: 4 had peptic ulcer and 19 had chronic and/or atrophic gastritis; these latter patients were selected as controls, to be compared with patients with ITP who had the same gastric pathology. Regarding the mucosal B-cell clonality, no significant differences were noted between patients with ITP and control patients: 6 (60%) of 10 patients with ITP and 11 (58%) of 19 control patientss were mono- or oligoclonal (P = .61), while the remaining patients were polyclonal. Similarly, no differences were noted in respect to T-cell clonality: 3 (33%) of 9 patients with ITP were monoclonal, and 5 (29%) of 17 control patients were mono- or oligoclonal (P = .587; Table 4). As far as the responsiveness to eradication treatment, B-cell oligo-monoclonality was detected in 5 (83%) of 6 responsive patients and 1 (25%) of 4 nonresponsive patients (P = .065). Likewise, 2 (40%) of 5 responsive patients showed T-cell monoclonality versus 1 (25%) of 4 nonresponsive patients (P = .635; Table 4).
Virulence factor distribution: gastric B- and T-cell clonality
| Patient no. . | Sex, age in y . | cagA . | vacA s1 . | vacA s2 . | vacA m1 . | vacA m2 . | ice A1 . | ice A2 . | bab A2 . | IgH . | TCRγ . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients with ITP | |||||||||||
| 39 | M, 83 | + | + | − | + | − | − | + | − | Oligoclonal | ND |
| 41* | M, 78 | − | − | + | − | + | + | − | − | Polyclonal | Polyclonal |
| 42* | F, 30 | − | − | + | − | + | + | − | − | Polyclonal | Polyclonal |
| 47 | M, 47 | + | + | − | + | − | + | + | + | Polyclonal | Monoclonal |
| 48 | F, 27 | + | + | − | − | + | + | − | − | monoclonal | Polyclonal |
| 49 | M, 37 | − | − | + | − | + | + | − | − | Oligoclonal | Monoclonal |
| 50 | M, 37 | + | + | − | − | + | − | + | − | monoclonal | Polyclonal |
| 40 | F, 24 | + | + | − | − | + | - | + | ND | Oligoclonal | Polyclonal |
| 59* | M, 34 | + | + | − | − | + | + | − | + | monoclonal | Polyclonal |
| 58* | F, 45 | + | + | − | − | + | + | − | + | Polyclonal | Monoclonal |
| Control patients without ITP, with gastritis | |||||||||||
| 1 | M, 34 | + | + | − | + | − | + | + | + | Oligoclonal | Monoclonal |
| 2 | M, 89 | − | + | − | − | + | + | − | − | monoclonal | Polyclonal |
| 3 | F, 36 | − | + | − | − | + | − | + | − | Polyclonal | Polyclonal |
| 4 | M, 65 | − | − | + | − | + | + | − | − | Oligoclonal | Monoclonal |
| 5 | M, 60 | − | + | − | − | + | − | + | + | monoclonal | Polyclonal |
| 6 | M, 67 | + | + | − | + | − | − | − | + | Polyclonal | Polyclonal |
| 7 | F, 34 | − | − | + | − | + | + | − | ND | Polyclonal | Polyclonal |
| 8 | M, 74 | − | − | + | − | + | + | − | − | monoclonal | ND |
| 9 | M, 40 | + | + | − | − | + | − | + | + | Oligoclonal | Oligoclonal |
| 10 | F, 53 | + | + | − | − | − | − | + | + | Polyclonal | Polyclonal |
| 11 | M, 78 | − | − | + | − | + | − | + | ND | Polyclonal | Polyclonal |
| 12 | M, 36 | + | + | − | + | − | − | + | + | monoclonal | Polyclonal |
| 13 | F, 40 | − | − | + | − | + | + | − | − | Polyclonal | Polyclonal |
| 14 | F, 51 | − | − | + | − | + | − | − | − | Polyclonal | Oligoclonal |
| 15 | F, 71 | − | − | + | − | + | + | + | + | monoclonal | Monoclonal |
| 16 | F, 73 | − | − | + | − | + | + | − | − | monoclonal | Polyclonal |
| 17 | F, 77 | − | − | + | − | + | + | − | − | Oligoclonal | Polyclonal |
| 18 | F, 51 | − | + | − | + | − | + | − | + | Polyclonal | ND |
| 19 | F, 58 | − | − | + | − | + | + | − | + | Oligoclonal | Polyclonal |
| Patient no. . | Sex, age in y . | cagA . | vacA s1 . | vacA s2 . | vacA m1 . | vacA m2 . | ice A1 . | ice A2 . | bab A2 . | IgH . | TCRγ . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients with ITP | |||||||||||
| 39 | M, 83 | + | + | − | + | − | − | + | − | Oligoclonal | ND |
| 41* | M, 78 | − | − | + | − | + | + | − | − | Polyclonal | Polyclonal |
| 42* | F, 30 | − | − | + | − | + | + | − | − | Polyclonal | Polyclonal |
| 47 | M, 47 | + | + | − | + | − | + | + | + | Polyclonal | Monoclonal |
| 48 | F, 27 | + | + | − | − | + | + | − | − | monoclonal | Polyclonal |
| 49 | M, 37 | − | − | + | − | + | + | − | − | Oligoclonal | Monoclonal |
| 50 | M, 37 | + | + | − | − | + | − | + | − | monoclonal | Polyclonal |
| 40 | F, 24 | + | + | − | − | + | - | + | ND | Oligoclonal | Polyclonal |
| 59* | M, 34 | + | + | − | − | + | + | − | + | monoclonal | Polyclonal |
| 58* | F, 45 | + | + | − | − | + | + | − | + | Polyclonal | Monoclonal |
| Control patients without ITP, with gastritis | |||||||||||
| 1 | M, 34 | + | + | − | + | − | + | + | + | Oligoclonal | Monoclonal |
| 2 | M, 89 | − | + | − | − | + | + | − | − | monoclonal | Polyclonal |
| 3 | F, 36 | − | + | − | − | + | − | + | − | Polyclonal | Polyclonal |
| 4 | M, 65 | − | − | + | − | + | + | − | − | Oligoclonal | Monoclonal |
| 5 | M, 60 | − | + | − | − | + | − | + | + | monoclonal | Polyclonal |
| 6 | M, 67 | + | + | − | + | − | − | − | + | Polyclonal | Polyclonal |
| 7 | F, 34 | − | − | + | − | + | + | − | ND | Polyclonal | Polyclonal |
| 8 | M, 74 | − | − | + | − | + | + | − | − | monoclonal | ND |
| 9 | M, 40 | + | + | − | − | + | − | + | + | Oligoclonal | Oligoclonal |
| 10 | F, 53 | + | + | − | − | − | − | + | + | Polyclonal | Polyclonal |
| 11 | M, 78 | − | − | + | − | + | − | + | ND | Polyclonal | Polyclonal |
| 12 | M, 36 | + | + | − | + | − | − | + | + | monoclonal | Polyclonal |
| 13 | F, 40 | − | − | + | − | + | + | − | − | Polyclonal | Polyclonal |
| 14 | F, 51 | − | − | + | − | + | − | − | − | Polyclonal | Oligoclonal |
| 15 | F, 71 | − | − | + | − | + | + | + | + | monoclonal | Monoclonal |
| 16 | F, 73 | − | − | + | − | + | + | − | − | monoclonal | Polyclonal |
| 17 | F, 77 | − | − | + | − | + | + | − | − | Oligoclonal | Polyclonal |
| 18 | F, 51 | − | + | − | + | − | + | − | + | Polyclonal | ND |
| 19 | F, 58 | − | − | + | − | + | + | − | + | Oligoclonal | Polyclonal |
ND indicates not done.
Nonresponders to eradication treatment.
A different frequency distribution of the various H pylori virulence genes in patients with ITP compared with the controls was noted: the cagA, vacAs1, and iceA1 genes are each independently overrepresented in patients with ITP compared with the control patients, while conversely, the vacAs2 and the babA2 genes are overrepresented in the control group. Nevertheless, only the higher frequency of the cagA gene in patients with ITP was statistically significant (P = .02; Table 5). The expression of the babA2 gene was detected in 3 (30%) of 10 ITP patients and in 9 (47%) of 19 control patients (P = .309). In patients with ITP, the expression of the babA2 gene is apparently associated with the absence of response to eradication treatment. Of 4 ITP patients not responsive to eradication, 2 showed cagA negativity, and 2 showed cagA positivity (Table 4). The patient (no. 49) with late response was cagA negative. If a concomitant expression of at least 3 genes—the so-called “triple-positive strains”—is considered, the frequency of concomitant cagA, vacAs1, and iceA genes was significantly higher in patients with ITP than in control patients (7 [70%] of 10 vs 4 [22%] of 19; P = .015; Table 6).
Virulence factor distribution between patients with ITP and control patients
| . | cagA, no. (%) . | vacAs1, no. (%) . | s2, no. (%) . | m1, no. (%) . | m2, no. (%) . | iceA1, no. (%) . | A2, no. (%) . | babA2, no. (%) . |
|---|---|---|---|---|---|---|---|---|
| Patients with ITP | 7/10 (70) | 7/10 (70) | 3/10 (30) | 2/10 (20) | 8/10 (80) | 7/10 (70) | 4/10 (40) | 3/9 (33) |
| Control patients | 5/19 (26) | 9/19 (47) | 10/19 (53) | 4/19 (21) | 14/19 (74) | 11/19 (57) | 8/19 (42) | 9/17 (53) |
| P | .02 | .24 | .24 | .9 | .7 | .5 | .9 | .3 |
| . | cagA, no. (%) . | vacAs1, no. (%) . | s2, no. (%) . | m1, no. (%) . | m2, no. (%) . | iceA1, no. (%) . | A2, no. (%) . | babA2, no. (%) . |
|---|---|---|---|---|---|---|---|---|
| Patients with ITP | 7/10 (70) | 7/10 (70) | 3/10 (30) | 2/10 (20) | 8/10 (80) | 7/10 (70) | 4/10 (40) | 3/9 (33) |
| Control patients | 5/19 (26) | 9/19 (47) | 10/19 (53) | 4/19 (21) | 14/19 (74) | 11/19 (57) | 8/19 (42) | 9/17 (53) |
| P | .02 | .24 | .24 | .9 | .7 | .5 | .9 | .3 |
Distribution of ″triple-positive strains″ in patients with ITP and control patients
| Patients with ITP, no. (%) | 7/10 (70) |
| Control patients, no. (%) | 4/19 (22) |
| P | .015 |
| Patients with ITP, no. (%) | 7/10 (70) |
| Control patients, no. (%) | 4/19 (22) |
| P | .015 |
Concomitant expression of cagA, vacAs1, and iceA.
Discussion
The results of our study demonstrate the remarkable therapeutic efficacies (ie, bacterium eradication rate, platelet response rate, and durability of response) of antibiotics plus proton-pump inhibitors for an homogeneous ethnic group of adult patients with chronic ITP and active H pylori infection.
These findings are similar to those reported by several groups with 3 exceptions.3-17,28-35 The prevalence (51%) of bacterium infection in our series is not higher than that (58%) in the general population of the area of Modena province,36 or that (67%) in healthy Italian blood donors aged 50 years or older,37 in keeping with the data from the other countries, where the prevalence of infection in patients with ITP is similar or lower than that of the general population of the same area,6,10,13,38,39 with rare exceptions.15,40 In our study, we observed a platelet improvement in 68% of patients with eradicated infection (60.5% of patients infected; 30.6% of total patients with ITP); in about 1500 patients so far reported in the literature, including the 3 US and Spanish cohorts with the lowest responses, the rate of response was about 53%.17
The highest response rate was reported in cohorts from Italy, Japan, and the United Kingdom. A better response in younger Italian and British patients with high baseline platelet counts and minor duration of the disease,10 and better results in Japanese patients older than 60 years40 or in Italian patients not previously treated7 have been reported. In our series, no differences between responders and nonresponders were noted in sex ratio, mean age, disease duration, previous treatments, and baseline platelet counts. Platelet recovery was found in patients previously refractory to immunosuppression or splenectomy, as reported by others.7,40 We also observed a response rate of 71% in patients with a severe form of ITP (platelets < 30 × 109/L), similar to that of other reports,7,40 whereas minor41 or nearly negative10 results were also reported.
A total of 9 (64%) of our 14 patients with severe, refractory ITP who failed to maintain a platelet count higher than 30 × 109/L after 6 to 12 months of standard therapy maintained a response for a median of 34 months (range, 26-46 months); 1 patient maintained a response for 73 months. This finding seems to be of interest if compared, for example, with the results of treatment of ITP with rituximab. A recent systematic review on more than 300 patients treated with rituximab, many of whom had a severe form of ITP, showed an overall response of 62.5% with a median response duration of 10.5 months, while relapse was found to occur in 10.5% of the patients. Of note, 21.6% of the patients experienced mild or moderate adverse events, and 3.7% experienced severe events, while 2.9% of deaths (even if not necessarily attributed to rituximab) were recorded.42 Conversely, we never observed toxicity related to H pylori eradication treatment.
The administration of eradication therapy to H pylori–negative patients with ITP failed to show any platelet increase in all treated patients, as observed by others,8,15,32,41,43 suggesting the crucial role of bacterium eradication rather than an effect of antibiotics by itself.
Of interest, all of our patients with ITP who underwent gastric biopsy showed at histologic examination chronic and/or atrophic gastritis, although gastric symptoms have never been disclosed. A similar finding, but in dyspeptic patients with ITP, has only been reported by another group.40
Finally, at the end of follow-up, our living patients are all in remission, without any treatment; only 1 patient relapsed, and 2 died from non-ITP–related disease. The follow-up of 60 months in our study is the longest reported so far, whereas in the literature, it varies from 4 to 24 months, except for 1 series followed for 31.2 months.14
The variability in the clinical outcome of eradicating the bacterium in patients from different countries and some differences in clinical features of responsive patients, even from the same area, raise the issue of whether and how H pylori infection plays a role in the development or persistence of a proportion of ITP. The pathogenetic mechanisms of ITP have still to be fully elucidated, and include platelet destruction due to phagocytosis by macrophages, antibody-dependent cell-mediated cytotoxicity,44 and T-cell–mediated destruction.45 The disease has also been associated with impaired megakaryocyte production.46 Several hypotheses have been raised to explain the possible interaction between H pylori and thrombocytopenia.10,41,46-49 Some H pylori strains bind von Willebrand factor and interact with glycoprotein Ib to induce platelet aggregation, but its contribution to immune thrombocytopenia remains to be demonstrated.50 Nevertheless, these hypotheses have yet to be confirmed and cannot be easily reconciled with the observation that improvement in the platelet count was generally seen 2 weeks after completion of eradication therapy, as reported also by others.10
To address these issues and to give further insights into the role of H pylori in chronic ITP, we investigated the possible clonality of B and T cells in the gastric mucosa and assessed the H pylori genotypes in patients with ITP compared with those without ITP with the same gastric pathology. Gastric B-cell and T-cell monoclonality or oligoclonality have been observed in certain instances of H pylori chronic gastritis, without ITP.51,52 Peripheral blood B-cell clonality has elsewhere been reported in a low percentage of infected patients with ITP.53 No differences in the pattern of B-cell and T-cell clonality have been found between our infected patients with ITP and control participants. A prevalence of B-cell clonality was noted in 83% of our responsive patients versus the 25% of nonresponsive patients; a prevalence of T-cell clonality was present in 40% of responsive patients versus 25% of nonresponsive patients. Peripheral blood T-cell clonality has been observed in patients with ITP and H pylori infection, prevailing in responder patients.54 Peripheral blood B- and/or T-cell clonality has been noted in noninfected patients with ITP, with better response to therapy.54,55 On the whole, the findings from our limited series do not suggest a clear role of B- and T-cell clonality in the pathogenesis of ITP associated with H pylori infection.
The analysis of frequency distribution of the various H pylori virulence genes showed a marked difference between patients with ITP and control participants: the cagA, vacAs1, and iceA genes are each independently overrepresented in patients with ITP compared with control participants, while conversely, the vacAs2 and babA2 genes are overrepresented in the control group. Nevertheless, the main finding appears to be the higher frequency of the cagA gene in patients with ITP, even statistically significant (P = .02). In addition, the concomitant expression of at least 3 genes, cagA, vacAs1, and iceA, “triple -positive strains,” is significantly more frequent in patients with ITP than in control participants (P = .015). Conversely, the frequency of babA2 gene expression is significantly lower in patients with ITP than in controls, but of note, in 2 of 3 patients with ITP it is apparently associated with the absence of platelet response to eradication treatment. No differences in the virulence profile of cagA, vacA, and iceA strains were found in Japanese patients with ITP compared with control patients with ulcer or gastritis.40 On the other hand, other Japanese investigators found no differences in H pylori virulence factors between responder and nonresponder patients with ITP.13 The association of some specific H pylori genotypes with ITP is reminiscent of the association between certain H pylori genotypes and other human diseases, such as gastric ulcer and gastric adenocarcinoma, which correlate with “triple-positive strains” babA2, vacAs1, and cagA,24 or intestinal metaplasia, correlating with cagA, vacAs1m1, and babA2,56 while the iceA1 gene was suggested to be a marker of peptic ulcer.57
The existence of some specific genotypes of H pylori associated with ITP might explain the different platelet response rates to eradication treatment in ITP from different geographic areas, which may have different genotype distribution. The existence of some specific genotypes of H pylori, with a different pathogenic potential in relation to ITP, might overcome the issue raised by the finding of similar seroprevalence rates of H pylori infection in patients with ITP compared with control participants. Although our small series may not adequately represent the whole ITP population, it may provide some useful insights into the pathogenesis of H pylori–related ITP. In summary, whichever is the mechanism by which H pylori might contribute to ITP, the eradication of the bacterium has proved to be of significant clinical value in a considerable number of patients with ITP. The long follow-up and the extremely low percentage of relapse in our series suggest a sustained recovery of disease for most patients with ITP responsive to H pylori eradication. Thus, the screening of all patients with ITP for H pylori at diagnosis and the eradication of the bacterium in H pylori–positive patients should precede other specific treatments for ITP whenever possible. This strategy is a useful and inexpensive way to avoid the discomfort and side effects of either immunosuppressive treatments or splenectomy in a subset of patients with ITP.
Further investigations are warranted to address how some of the H pylori virulence factors, identified in our study, may affect disease pathogenesis in ITP.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We are indebted to Dr Alberto Merighi, Dr Anna Maria Primerano, and Dr Antonella Scancelli (Gastroenterology Unit, Modena); Prof Roberto Marasca, Prof Alessandro Liberati, Dr Katia Cagossi, Dr Leonardo Ferrara, Dr Annalisa Imovilli, Dr Giovanni Riva, and Dr Roberto D'Amico (Department of Oncology and Hematology, Modena); and Dr Daniele Vallisa (Department of Oncology and Hematology, Azienda Unità Sanitaria Locale (AUSL) Piacenza).
This work was supported in part by the Italian Ministry for University and Scientific Research (MIUR), Rome, Italy; Associazione Italiana per la Ricerca sul Cancro (AIRC), Milan, Italy; and the European Commission FP6 Life-Sciences-Health Program (INCA Project: LSHC-CT-2005–018704).
Authorship
Contribution: G.E., M.L., and G.T. designed the research; G.E. and M.L. analyzed data and wrote the paper; P.Z. performed molecular studies; G.J. attended to statistical analysis; M.M., L.P., F.F., F.V., G.L., and A.D. performed the clinical studies. G.E. and M.L. contributed equally to the study.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Giovanni Emilia, Department of Oncology and Hematology, Policlinico, via del Pozzo 71, 41100 Modena, Italy; e-mail: emilia.giovanni@unimore.it.