Abstract
The primary granule proteins elastase (ELA2) and proteinase 3 (PR3) both contain the nonapeptide PR1, which can induce cytotoxic T lymphocyte (CTL) responses against chronic myeloid leukemia (CML) cells. To investigate whether eradication of CML after allogeneic stem cell transplantation (SCT) was influenced by PR3 and ELA2 gene expression or PR1-specific CTL responses, we studied cells from 87 CML patients and 27 HLA-A*0201+ donors collected prior to T-cell–depleted HLA-identical sibling SCT. For patients in advanced phase (AdP), a higher expression of both PR3 and ELA2 in CD34+ progenitors before SCT was associated with a lower incidence of relapse-related death, improved leukemia-free survival (LFS), and overall survival (OS); in chronic phase patients, no differences were observed. PR1-CTL responses were detected in 7 of 27 HLA-identical sibling donors, and associated with improved LFS and OS after SCT on follow-up. PR1-CTL responses detected in 7 of 28 CML patients before transplantation were not predictive of outcome and correlated inversely with PR3 and ELA2 expression. These findings suggest that assessment of PR3 and ELA2 expression in leukemic progenitors is useful for predicting posttransplantation outcome in AdP patients undergoing SCT. The presence of a donor immune response against PR1 may be advantageous and could be exploited therapeutically.
Introduction
Although the advent of tyrosine kinase inhibitors (TKIs) has greatly broadened the treatment options for patients with chronic myeloid leukemia (CML),1,2 allogeneic stem cell transplantation (SCT) remains the only treatment that can conclusively eradicate disease.3-5 The curative effect of SCT has been attributed to the allogeneic graft-versus-leukemia (GVL) effect to which CML is particularly susceptible, as evidenced by the success of donor lymphocyte infusion (DLI) in the treatment of disease relapse, and improved rates of long-term disease-free-survival in patients who have graft-versus-host disease (GVHD).6,7 The primary granule proteins neutrophil elastase (ELA2) and proteinase 3 (PR3) both contain the nonapeptide PR1,8,9 which can elicit leukemia-associated cytotoxic T lymphocyte (CTL) responses in CML patients as well as in healthy individuals.10 The presence of PR1 responses in CML patients after SCT has been found to correlate with complete remission, suggesting that T-cell responses to PR3 and ELA2 in leukemia cells are implicated in GVL.11 Furthermore, in a large group of CML patients not undergoing SCT, higher expression of the ELA2 and PR3 genes encoding these proteins in CD34+ progenitors of CML patients in chronic phase (CP) correlates with improved survival.12 This observation suggests that high PR3 and ELA2 expression is linked either to a favorable antileukemia immune effect, or to a more favorable intrinsic leukemia phenotype or to both.
Therapeutic success in CML, whether associated with SCT or TKI, is less frequent in patients with CML whose disease has advanced beyond the chronic phase. TKIs have limited efficacy and SCT is associated with higher relapse rates and transplant-related mortality. This reduced treatment responsiveness could be due to an escape from immune regulation or to an intrinsic gain of leukemic potential, or to both; and might therefore implicate changes in primary granular protein expression as well as in T-cell responses to PR1.
To explore how ELA2 and PR3 expression and associated T-cell responses affected leukemia control after SCT and how they differed between chronic phase and more advanced CML, we investigated 87 CML patients receiving SCT from HLA-identical siblings. We sought to determine whether PR1-specific CTL responses in either the patient or donor before SCT were associated with molecular remission (MR) after SCT. Using real-time quantitative reverse-transcription–polymerase chain reaction (RQ-PCR), we also investigated the influence of ELA2 and PR3 expression in leukemic CD34+ progenitors on outcome after SCT. We found that higher ELA2 and PR3 expression in leukemic progenitor cells in advanced-phase (AdP) CML was associated with an improved outcome after SCT, suggesting that factors intrinsic to the leukemia in a given patient may be an important predictive factor. The presence of a PR1-CTL response in the donor cells may further improve antileukemic immunologic effects.
Patients, materials, and methods
Patients
All CML patients who underwent T-cell–depleted SCT between September 1993 and May 2006 in the Hematology Branch, National Heart, Lung, and Blood Institute were eligible for study inclusion provided pre-SCT cells were available. The pre-SCT disease status of either CP or AdP (accelerated and blast phase) was determined using the International Bone Marrow Transplant Registry criteria.13 Patients reported in this work were enrolled in National Heart, Lung and Blood Institute's Institutional Review Board–approved studies. All patients and donors gave written informed consent in accordance with the Declaration of Helsinki before enrolling in myeloablative (n = 84 patients) or nonmyeloablative (n = 3 patients) transplantation protocols, details of which have been reported previously14,15 and are summarized in Table 1. In brief, myeloablative conditioning consisted of 3 consecutive transplant conditioning regimens: [1] 13.5 Gy total body irradiation (TBI) with cyclophosphamide (Cy) 120 mg/kg and standard-dose cyclosporine (target plasma levels, 200-400 μg/L); 24 patients received bone marrow grafts (September 1993-December 1996) and 15 patients received peripheral blood stem cell transplant (PBSCT) (January 1997-January 1999); [2] 13.5 Gy TBI with Cy 120 mg/kg and low-dose cyclosporine (target levels 100-200 μg/L), or no cyclosporine; 23 patients received PBSCT (March 1999-August 2001); [3] 12 Gy TBI with Cy 120 mg/kg, fludarabine 125 mg/m2, and low-dose cyclosporine, or no cyclosporine; 22 patients received PBSCT (February 2002-May 2006). Three patients received nonmyeloablative conditioning with fludarabine 125 mg/m2, Cy 120 mg/kg, and standard-dose cyclosporine or mycophenolate mofetil with PBSCT. All patients received T-cell–depleted grafts (containing 0.2-2 × 105/kg residual CD3+ T cells) and from December 1996, only PBSCT was performed.14 In the absence of GVHD, or unless MR was documented, 1-5 × 107/kg CD3+ T cells were added back on days 30 to 60 (n = 67) or on day 100 (n = 14) as previously reported.16 Only 12 patients had T cells added at both time points. Cyclosporine was given for 6 months from the day prior to DLI, and tapered off if no chronic GVHD occurred.14,16 Standard prophylaxis against infection included fluconazole, trimethoprim/sulfamethoxazole for at least 6 months after SCT, and weekly surveillance for cytomegalovirus (CMV) antigenemia as previously described.17,18 Current leukemia-free survival (LFS) was defined as the survival without evidence of leukemia (MR) at the time of the most recent assessment.19
Patient characteristics
| Factor . | No. (%) . |
|---|---|
| Sex | |
| Female | 28 (32) |
| Male | 59 (68) |
| Disease phase | |
| Chronic | 55 (63) |
| Accelerated | 26 (30) |
| Blastic | 6 (7) |
| HLA type–HLA-A*0201 | |
| Positive | 31 (36) |
| Negative | 56 (64) |
| Source of stem cells for SCT | |
| BM | 24 (28) |
| PBSC | 63 (72) |
| Conditioning regimen | |
| 13.5 Gy TBI, Cy 120 mg/kg, SD CSA | |
| BMT | 24 (28) |
| PBSC transplantation | 15 (17) |
| 13.5 Gy TBI, Cy 120 mg/kg, LD CSA or no CSA; PBSC transplantation | 23 (26) |
| 12 Gy TBI, Cy 120 mg/kg, Flu 125mg/m2, LD CSA or no CSA; PBSC transplantation | 22 (25) |
| Cy 120 mg/kg, Flu 125 mg/m2, CSA ± mycophenolate mofetil; PBSC transplantation | 3 (4) |
| PR1 responses | |
| Patient, n = 28 | 7 (25) |
| Donor, n = 27 | 7 (26) |
| Factor . | No. (%) . |
|---|---|
| Sex | |
| Female | 28 (32) |
| Male | 59 (68) |
| Disease phase | |
| Chronic | 55 (63) |
| Accelerated | 26 (30) |
| Blastic | 6 (7) |
| HLA type–HLA-A*0201 | |
| Positive | 31 (36) |
| Negative | 56 (64) |
| Source of stem cells for SCT | |
| BM | 24 (28) |
| PBSC | 63 (72) |
| Conditioning regimen | |
| 13.5 Gy TBI, Cy 120 mg/kg, SD CSA | |
| BMT | 24 (28) |
| PBSC transplantation | 15 (17) |
| 13.5 Gy TBI, Cy 120 mg/kg, LD CSA or no CSA; PBSC transplantation | 23 (26) |
| 12 Gy TBI, Cy 120 mg/kg, Flu 125mg/m2, LD CSA or no CSA; PBSC transplantation | 22 (25) |
| Cy 120 mg/kg, Flu 125 mg/m2, CSA ± mycophenolate mofetil; PBSC transplantation | 3 (4) |
| PR1 responses | |
| Patient, n = 28 | 7 (25) |
| Donor, n = 27 | 7 (26) |
The median age of patients was 36 years (range, 12–68 years).
SCT indicates allogeneic stem cell transplantation; BM, bone marrow; PBSC, peripheral blood stem cell; TBI, total body irradiation; Cy, cyclophosphamide; SD, standard dose; CSA, cyclosporine; LD, low dose; Flu, fludarabine; and PR1, VLQELNVTV nonapeptide.
Sample preparation
For laboratory studies, cells (mainly leukapheresis products) were collected within 2 months prior to SCT. Pre-SCT bone marrow cells were used in 9 patients. Donor leukaphereses were collected before administration of granulocyte colony-stimulating factor (G-CSF) to mobilize stem cells for the actual transplantation. Mononuclear cells (MNCs) from either leukapheresis product or bone marrow harvest were isolated using Ficoll-Hypaque density gradient centrifugation (Organon Teknika, Durham, NC) and cryopreserved in RPMI 1640 supplemented with 20% fetal calf serum and 10% dimethyl sulfoxide. CD34+ cells from thawed MNCs were selected by binding to immunomagnetic beads (MiniMACS; Miltenyi Biotec, Auburn, CA) according to the manufacturer's instructions. In HLA-A*0201+ patients and donors, CD8+ T cells were purified using immunomagnetic beads, which were detached using DetachaBead (Dynal, Oslo, Norway) according to the manufacturer's instructions. Total RNA was extracted from CD34+, CD34−, and CD8+ cells using the RNeasy kit (Qiagen, Valencia, CA). Reverse transcription was performed using the Advantage RT-for-PCR kit (Clontech, Mountain View, CA).
PR1-CTL responses
Purified CD8+ cells were rested overnight in RPMI 1640 supplemented with 10% fetal calf serum. C1R-A2 cells (American Type Culture Collection, Manassas, VA), which are C1R cells (from an HLA-A–null human B-lymphoblastoid cell line) expressing a transfected genomic clone of HLA-A2.1,20 were loaded with PR1 peptide (VLQELNVTV) at 0.1-, 1.0-, and 10-μM doses for 2 hours, and subsequently cocultured with CD8+ T cells for 3 hours. CMV peptide 495-503 (NLVPMVATV) and the synthetically modified gp100 peptide (209-2M) melanoma self-antigen 209-217 (IMDQVPFSV) were used as positive controls. PR1-CTL response was measured as interferon-γ mRNA expression (relative to CD8) obtained by RQ-PCR as previously described.10
RQ-PCR for ELA2 and PR3 expression
TaqMan Assays-on-demand probe-and-primer reagents (Applied Biosystems, Foster City, CA) for ELA2, Hs00357734_m1, and PR3, Hs00160521_m1, were used according to the manufacturer's instructions. ABL expression was used as the endogenous cDNA quantity control for all samples. Its expression was measured using 300 nM primers and 200 nM probe as previously described.12 All reactions were performed in triplicate on 10 μL volume using standard conditions with 40 cycles of amplification using the ABI PRISM 7900 sequence detection system.
Post-SCT analysis for MR
BCR-ABL mRNA levels were monitored serially in patient total leukocytes at regular intervals after SCT using RT-PCR with details as previously described.14 Briefly, until July 2003, a double-nested PCR to amplify BCR-ABL and a single-round PCR to amplify the control gene ABL were used. Subsequently, duplicate cDNA samples were assayed using RQ-PCR with 50 cycles of amplification in a Light-Cycler (Roche, Mannheim, Germany) using a commercial RQ-PCR kit for G6PDH (Roche, Indianapolis, IN) as the control gene. In all reactions, serial 10-fold dilutions of RNA prepared from the BCR-ABL–positive cell line K562 was used as positive control, and RNA from the BCR-ABL–negative cell line HMy was used as the negative control. Assays could detect classical e13a2 and e14a2 transcripts, but not transcripts from other minor breakpoint cluster regions.
In this report, patient samples were considered positive for BCR-ABL if bands were detected on ethidium bromide–stained agarose gel electrophoresis in the double-nested PCR or if either of the duplicate samples generated a signal beyond the threshold in RQ-PCR. Samples were considered negative for BCR-ABL in the absence of a band if RNA integrity was confirmed by satisfactory amplification of the control gene. The sensitivity of both double-nested PCR and RQ-PCR for BCR-ABL was comparable. Both assays could detect BCR-ABL transcripts in K562 RNA diluted to 1:100 000 to 1:1 000 000 in control RNA.
Statistical methods
Patient groups were compared using the χ2 test for categorical data or Mann-Whitney U test for continuous data. Survival curves were calculated using the Kaplan-Meier method, and patient groups were compared using the log-rank test. Patients were divided into groups delineated by the median, or upper or lower quartile cutoffs of RQ-PCR expression values for ELA2 and PR3. RQ-PCR results from CD34+ and CD34− populations in patient samples were compared using Spearman ρ. P values were from 2-sided tests with values < .05 considered significant. Data analysis was performed using SPSS 14 for Windows software (SPSS, Chicago, IL).
Results
Transplantation outcome
Patient characteristics are described in Table 1. The median follow-up time for the cohort after SCT was 61.7 months (range, 0.5-157 months). Patients underwent transplantation at a median of 12.8 months from diagnosis (range, 1.6-147 months). Details of conditioning regimens and GVHD prophylaxis have recently been reported.14-16 In this patient cohort, disease phase, CD34 dose at SCT, and lymphocyte count at day 30 were associated with superior overall survival (OS) and LFS.14 As patients underwent transplantation over a 13-year period, T-cell depletion techniques and stem cell collection methods were systematically improved with the advent of newer technology.17,21 However, as recently reported, there was no difference in LFS and OS between older transplant protocols and more recent protocols.14 In particular, relapse rates in these patient groups have not changed despite modest improvements in transplant-related mortality with era of transplantation (unpublished data, B.N.S. and A.J.B., January 2007).
Thirty-seven (42%) of the 87 patients relapsed; 14 had molecular relapse and 23 had hematologic relapse. Additional DLI alone was given in 13 patients, imatinib alone in 8 patients, and a combination of DLI and imatinib, or chemotherapy as indicated in 16 patients.22,23 Sixty-five (75%) of the 87 CML patients were alive at one year after SCT, and 44 of these surviving patients (68%) had achieved MR at this time point. After a median of 90 months follow-up (range, 12-157 months) for patients who achieved MR at one year, no disease relapse occurred in 38 (86%) of 44 patients. Of the remaining 6 patients who were in MR at one year, 4 died of nonrelapse causes (3 from GVHD at 25, 29, and 64 months after SCT, and 1 from disseminated herpes infection at 12 months after SCT), and 2 patients relapsed—one underwent transplantation in blast phase, relapsed 45 months after SCT, and died of progressive disease, while the other patient underwent transplantation in CP and had further DLI for molecular relapse 66 months after SCT. Fourteen (67%) of the remaining 21 patients surviving one year but not in MR at this time point achieved MR on further follow-up (median, 61.7 months; range, 21-126 months).
Sample analysis
Pre-SCT cryopreserved cells for CD34+ selection were available in 82 of 87 CML patients, of which 51 were in CP and 31 in AdP (6 blast phase, 25 accelerated phase) at the time of SCT. In the majority (65/82, 79%), CD34+ cells were less than 10% of the total MNC population. The median CD34+ percentage was 2.9% (range, 0.2%-48.5%), with patients in AdP having the highest values. Thirty-one patients were HLA-A*0201+ and of these, adequate numbers of pre-SCT cells were available for assessment of the HLA-A*0201–restricted PR1-CTL response in 28 CML patients and 27 HLA-identical sibling donors.
PR3 and ELA2 gene expression in CML patients and association with post-SCT outcome
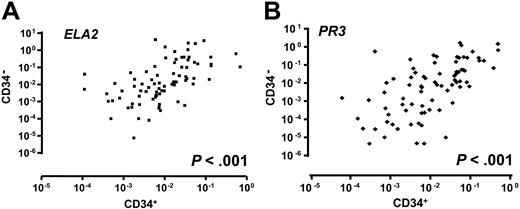
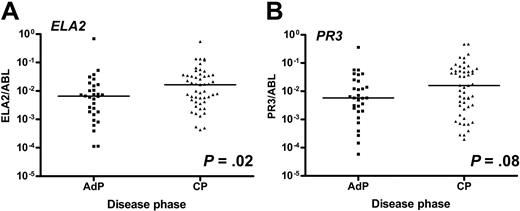
The expression of both PR3 and ELA2 genes was highly correlated in CD34+ and CD34− cells (P < .001, Figure 1), as was the expression of PR3 and ELA2 in both CD34+ and CD34− cells (P < .001). There was a differential expression of ELA2 in CML CD34+ progenitors according to the disease phase, with higher expression in CP patients compared with AdP patients (median, 0.0165 [range, 0.0004-0.55] vs 0.0065 [range, 0.0001-0.69], P = .02, Figure 2A). Although there was a trend for increased PR3 expression in CP patients in comparison with those in AdP, this did not reach statistical significance (median, 0.0159 [range, 0.0002-0.47] vs 0.0058 [range, 0.00006-0.36], P = .08, Figure 2B).
ELA2 and PR3 expression in CD34+ and CD34− populations. Scatterplots showing good correlation of ELA2 (A) and PR3 (B) expression between CD34+ and CD34− populations in CML patients before SCT. P values refer to Spearman ρ. Values of genes represent the RQ-PCR expression as a ratio of the gene of interest to the ABL control gene.
ELA2 and PR3 expression in CD34+ and CD34− populations. Scatterplots showing good correlation of ELA2 (A) and PR3 (B) expression between CD34+ and CD34− populations in CML patients before SCT. P values refer to Spearman ρ. Values of genes represent the RQ-PCR expression as a ratio of the gene of interest to the ABL control gene.
Relationship of ELA2 and PR3 expression with CML disease phase. Scatterplots showing expression of ELA2 (A) and PR3 (B) in CD34+ progenitors in chronic-phase (CP) compared with advanced-phase (AdP) CML. (Bars correspond with median.)
Relationship of ELA2 and PR3 expression with CML disease phase. Scatterplots showing expression of ELA2 (A) and PR3 (B) in CD34+ progenitors in chronic-phase (CP) compared with advanced-phase (AdP) CML. (Bars correspond with median.)
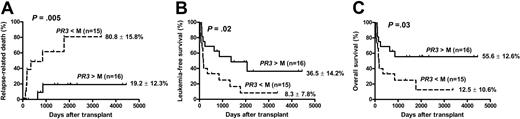
In a univariate analysis of all CML patients before SCT, the lowest expression (lower quartile) of both ELA2 and PR3 in CD34+ progenitors was associated with a higher relapse-related death (RRD) (P = .015 and P = .01, respectively), but not with OS or LFS. When patients in this cohort were analyzed according to CML disease phase, in CP patients ELA2 and PR3 expression was not associated with LFS and OS as no RRD occurred in this group. However, in AdP patients, who had a generally poorer outcome after SCT compared with CP patients, high expression of PR3 in CD34+ progenitors was associated with a reduced RRD (P = .005), resulting in superior OS and LFS (P = .03 and P = .02, respectively) (Figure 3). Similarly, in this group of AdP patients, a higher ELA2 expression in CD34+ progenitors was associated with a reduced RRD (21.3% ± 13.4% vs 72.7% ± 15.2%, P = .01) and improved OS (54.1% ± 13% vs 17.8% ± 10.5%, P = .04) and LFS (34.8% ± 14.1% vs 13.3% ± 8.8%, P = .049).
Transplantation outcome and PR3 expression in advanced phase CML. (A) Probability of relapse-related death, (B) leukemia-free survival, and (C) overall survival in AdP-CML. Groups are segregated according to the median (M) values of PR3 expression.
Transplantation outcome and PR3 expression in advanced phase CML. (A) Probability of relapse-related death, (B) leukemia-free survival, and (C) overall survival in AdP-CML. Groups are segregated according to the median (M) values of PR3 expression.
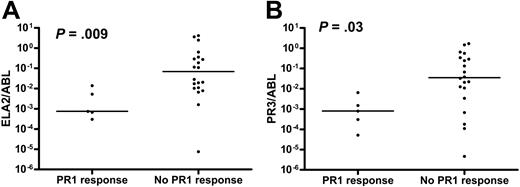
Relationship between patient PR1 responses and PR3 and ELA2 expression
PR1-CTL responses were detected in 7 of 28 HLA-A*0201+ CML patients before SCT. As the greater proportion of cells in the MNC population with the ability to present antigen was CD34−, a relationship between the expression of PR3 and ELA2 in these populations with PR1-CTL responses was sought. A lower expression of either PR3 or ELA2 in the CD34− population was associated with a detectable PR1-CTL response (P = .03 and P = .009 respectively, Figure 4). The presence of patient PR1-CTL responses before SCT was not associated with improved OS or LFS, or reduced RRD after SCT. Patient PR1-CTL response was not associated with MR after SCT (data not shown).
PR1-CTL responses in CML patients pre-SCT. Relationship of (A) ELA2 and (B) PR3 expression in CD34− cells of HLA-A*0201+ CML patients with native PR1-CTL response. (Bars correspond with median.)
PR1-CTL responses in CML patients pre-SCT. Relationship of (A) ELA2 and (B) PR3 expression in CD34− cells of HLA-A*0201+ CML patients with native PR1-CTL response. (Bars correspond with median.)
Donor PR1 response
PR1-CTL responses in HLA-A*0201+ donors were elicited using cells collected prior to G-CSF mobilization. Seven of 27 donors with available cellular material for study demonstrated PR1-CTL responses. Donor and patient PR1-CTL responses tended to occur independently; the detection of PR1-CTL responses in both donor and patient was found in only 2 patient-donor pairs, both in CP-CML. Patients who had a donor with PR1-CTL responses had improved LFS (71% vs 60%) and OS (86% vs 60%) after SCT compared with those whose donors had no PR1-CTL response; however, as this was a small cohort, this difference was not statistically significant. Patients with a donor PR1-CTL response had a shorter follow-up after SCT (median, 62 months; range, 28-86 months) compared with those without donor PR1-CTL response (median, 76 months; range, 4-157 months). The majority of HLA-A*0201+ patients had higher expression of PR3 and ELA2; 2 recipients from donors without PR1 responses and 1 recipient from a donor with PR1 response had low PR3 and ELA2 expression. Of the 7 patients who had donors with PR1-CTL responses, 6 were in CP and 1, in AdP. Of the 5 CP patients and single AdP patient with sufficient pre-SCT cells for assessment of PR3 and ELA2 expression in CD34+ progenitors, all except the AdP patient had high expression of either PR3 or ELA2. The AdP patient with low expression of both PR3 and ELA2 succumbed to RRD despite having donor PR1-CTL response. Durable MR had occurred in 5 of the 7 patients with donor PR1-CTL response by 4 years after SCT (median, 41 months; range, 28-48 months). Of the 20 other patients who had donors with no PR1-CTL responses, 8 were in AdP and 12 CP before SCT. Of these, 11 patients (10 CP and 1 AdP) achieved durable MR at a median of 36 months (range, 5-127 months) after SCT. Seven patients (2 CP, 5AdP) did not achieve durable MR (4 died of progressive CML after relapse and 3 are alive on follow-up with disease). The remaining 2 patients who were in AdP had early transplant-related mortality and were unevaluable for durable MR.
Discussion
The capacity of SCT to cure CML was established in the 1980s.5,13,24 Until the advent of TKI, the preferred initial treatment for newly diagnosed CML patients was SCT. In recent years, the efficacy of imatinib in inducing cytogenetic and molecular remissions in both CP and AdP disease has displaced SCT as primary treatment for CML in most patients. Nevertheless, SCT has withstood the test of time, with the longest survivors now living beyond 20 years from SCT,25 whereas a substantial proportion of patients treated with imatinib still have cytogenetically or molecularly detectable disease and are therefore at least theoretically at risk for leukemia recurrence. Furthermore, a significant number of patients fail initial treatment or acquire secondary resistance to imatinib and are therefore candidates for SCT.26 The durability and completeness of disease eradication after SCT for CML is attributed to the GVL effect. The demonstration that PR1, a nonapeptide derived from both PR3 and ELA2, which are proteins overexpressed in CML progenitors, could induce CTL preferentially lysing leukemic cells indicates that a specific GVL effect targeting these primary granular proteins is possible8,9,27 and is supported by the observation that PR1-CTL responses in CML patients after SCT correlate with disease remission.11 PR1-CTL responses have also been detected in healthy individuals using a sensitive RQ-PCR assay10 and transfer of PR1-specific T-cell clones from donor to recipient following SCT has been described,28 suggesting that pre-existing donor immunity to PR1 may be important in establishing a GVL effect.
In this cohort encompassing a relatively large number of CML patients treated with SCT, the majority (86%) of patients who had achieved MR one year after SCT remained free of detectable BCR-ABL transcripts after a median of 90 months follow-up, suggesting that these responses are durable. As PR1 is HLA-A*0201+ restricted, we were able to test only a third of patients and donors in our cohort for specific CTL responses. We could detect PR1-CTL responses in only 7 of 27 HLA-A*0201+ donors. By chance, the majority of the recipients of grafts from these donors were CP-CML, and thus we could not conclude whether the improved outcome in these patients was a result of the effectiveness of donor-derived PR1-CTL responses or simply a reflection of the better prognosis conferred by CP. Larger numbers of patients will be needed to identify whether donor PR1 response is an independent variable for transplantation outcome.
In patients who are not HLA-A*0201+, other epitopes of PR3 or ELA2 specific for different HLA alleles may be similarly presented. Our previous finding that T cells specific for several primary granular proteins (and with cytotoxicity to CML progenitors) occur in non–HLA-A*0201+ individuals suggests that there are numerous peptide epitopes of these proteins that can elicit GVL responses.9,29 As a control in this study, we also tested the HLA-A*0201+ donors for T-cell responses to the HLA-A*0201+ binding peptide WT1–126 (RMFPNAPYL) derived from WT1, the Wilms tumor antigen, which is also overexpressed in CML. Only 3 donors had detectable WT1-specific T cells, and only 1 of these had concurrent PR1-CTL response. Donor WT1-CTL response did not correlate with improved outcomes in the 3 recipients (data not shown). While these findings suggest that PR3 and ELA2 may be specifically implicated as antigens in the GVL response, they do not exclude the potential importance of other GVL targets such as minor histocompatibility antigens.30
Recently, a higher expression of both PR3 and ELA2 in CD34+ progenitors in CP-CML patients at diagnosis was found to be associated with a longer survival in a large cohort of patients who were not treated with SCT.12 We sought a relationship between PR3 and ELA2 expression in CML CD34+ progenitors and SCT outcome, as these progenitors are essential targets for the GVL effect, and have been shown to be eliminated in in vitro studies of CML patients responding to DLI after relapse.31 In this study in a heterogeneous group of CML patients, a higher PR3 and ELA2 expression in CD34+ progenitors was similarly associated with a reduced RRD. This effect was most marked in AdP-CML patients, where both OS and LFS were significantly improved in patients with higher PR3 and ELA2 expression. These findings are important because PR3 and ELA2 expression is the only prognostic disease marker so far identified in AdP patients that defines large survival differences (55% vs 12.5%, for high and low expression, respectively). Furthermore, these results suggest that GVL effects can occur even among poor-risk patients, and that patients responding favorably to SCT are those with a disease biology favoring GVL. The fact that CD34+ progenitors of AdP-CML patients have a lower expression of primary granule proteins, in particular ELA2, compared with those in CP may also explain why CML disease phase at the time of SCT remains the most important disease feature influencing transplantation outcome. Because of our ignorance of non–HLA-A*0201–restricted T-cell responses to primary granular proteins and the limited number of patients with HLA-A*0201 studied, this analysis could not definitively answer the question whether high expression of these proteins is a prerequisite for an effective donor GVL effect. However the data do support the notion that a T-cell response to primary granular proteins and a high expression of these proteins in leukemia progenitors are both favorable for optimum GVL effects.
We also investigated the relationship between the expression of genes that encode these primary granular proteins and PR1-CTL responses in CML patients before SCT. Interestingly, we found that a lower expression of either PR3 or ELA2 was associated with PR1-CTL responses, and no responses were detectable in patients with higher expression of either PR3 or ELA2 in CD34+ progenitors (data not shown) or their CD34− progeny. These findings are in keeping with a previous report suggesting that the abundance of PR3 and ELA2 proteins may cause immune tolerance with the deletion of high-avidity PR1-CTL clones.32 Furthermore, these results suggest that vaccination strategies using PR1 peptide alone in unconditioned CML patients in order to eradicate minimal residual disease could also cause disease tolerance.
In conclusion, our findings suggest that the eradication of CML after SCT may be dependent on 2 factors: first, a disease with a biology amenable to immunologic attack, which implicates both disease phase and primary granular protein expression, and second, the presence of an effective donor immune response against antigens such as PR1. These results allow us to speculate that in the context of SCT, peritransplantation vaccination strategies with PR1 for donors may improve post-SCT outcome without increasing the risk of GVHD. In AdP-CML patients who have a high risk of relapse after SCT, it may also be beneficial to attempt to manipulate disease biology by up-regulating PR3 expression, such as with interferon-α,33 in addition to early use of TKIs and DLI.22
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: A.S.M.Y. conceived and designed the study, processed samples, performed experiments, analyzed data, and wrote the report; K.R. performed experiments, advised on study design, and commented on the report; B.N.S. collected patient data, provided clinical care, performed statistical analysis, and commented on the report; R.E. processed samples and performed experiments; S.M. advised on statistical analysis and commented on the report; J.M.G. advised on study design and commented on the report; A.J.B. supervised the study, provided clinical care, and wrote the report.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Agnes S. M. Yong, Hematology Branch, National Heart, Lung, and Blood Institute, National Institutes of Health, Building 10, Hatfield CRC, Rm 3-5140, 10 Center Dr, MSC 1202, Bethesda, MD 20892-1202; e-mail: yonga@nhlbi.nih.gov.
References
National Institutes of Health

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal