In this issue of Blood, Brunstein and colleagues describe the use of nonmyeloablative conditioning and double umbilical cord blood transplantation (UCBT) for treatment of adult patients.
UCBT is an attractive source of hematopoietic progenitor cells that might be broadly applicable to patients lacking acceptable donors. A major limitation of UCBT has been the small cell dose and resulting delayed time to engraftment in adults. The data in this report convincingly demonstrate that rapid neutrophil recovery with ultimate predominance of a single cord can be achieved with this technique. Although the follow-up is short, the favorable relapse-free survival following a nonmyeloablative regimen suggests a potent UCB-mediated graft-versus-tumor effect. A single very large UCB unit meeting the protocol transplant standard was found and used in only 17 of the 110 patients, underscoring the limitations of comparing transplantation of 1 versus 2 cords in this study. Nevertheless, as suggested by the authors, it appears unlikely that a randomized comparison of unmanipulated single versus double UCBT will be performed for adults, in view of this data. Double UCBT seems likely to emerge as a standard to which newer adult UCBT techniques will be compared in the future.
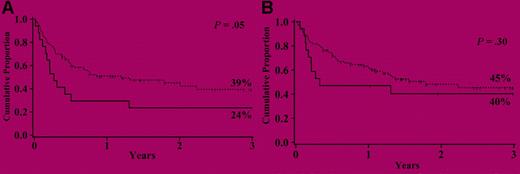
Cumulative proportion of 3-year event-free survival (A) and overall survival (B) for patients receiving either 1 (—) or 2 (■■■) UCB unit transplants after a nonmyeloablative conditioning regimen. See the complete figure in the article beginning on page 3064.
Cumulative proportion of 3-year event-free survival (A) and overall survival (B) for patients receiving either 1 (—) or 2 (■■■) UCB unit transplants after a nonmyeloablative conditioning regimen. See the complete figure in the article beginning on page 3064.
A number of important questions continue to surround double UCBT. How important is the increasing degree of HLA matching both to the recipient and between the 2 cords? It is likely that the rapidly enlarging CB banks will make tighter matching routinely possible. Since 2 cords may produce a somewhat higher incidence of acute graft-versus-host disease (GVHD) in adults than single CBT, is there an increased risk of infection or other GVHD complications using this technique? Should GVHD be modulated (as done in this study) using high-dose antithymocyte globulin (ATG) or similar techniques, and what is the association with risk of tumor relapse? How important is the long-term thrombocytopenia seen in a subset of these patients, and can new technologies overcome this problem? Why did younger patients in this study fare more poorly than older patients with favorable clinical features? Do they need more dose-intensive therapy? How important is careful patient selection, and to what degree does such selection limit the generalizability of the results of this trial?
This report, and other studies,1-3 provide increasing evidence that UCBT represents a practical and important advance in hematopoietic-cell transplantation. The improvement in engraftment and event-free survival reported here provides much encouragement for wider exploration of this technique. Issues such as the use of ex vivo UCB manipulation,4 in vivo administration of newer thrombopoietin-type agents,5 and optimization of immune suppression to modulate GVHD can now be explored in a more meaningful way. The relationship between preparative regimen intensity, GVHD, UCB engraftment, and toxicities requires investigation, as many patients may need more intensive chemotherapy regimens for tumor eradication. Disease-specific investigations will become an important part of future studies. Finally, some would argue that these results are sufficiently promising that randomized comparisons between UCBT and, for example, haploidentical peripheral blood transplantation will soon be warranted. The outcomes of the patients in this prospective report provide some of the most meaningful adult UCBT data to date, and can be used to benchmark future studies exploring this maturing technique in adults.
Conflict-of-interest disclosure: The authors declare no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal