In this issue of Blood, Gaetani and colleagues provide an analysis of mutations in α-spectrin that give rise to HE and HPP. Their results indicate a biochemical basis for mutations in a single gene giving rise to such widely varying clinical phenotypes.
Hereditary elliptocytosis (HE) has an estimated incidence in the United States of 3 to 5 members of the population per 10 000. The most common mutations underlying the disease are in the SPTA1 gene, which encodes αI-spectrin.1 Clinically, the phenotype is very variable, ranging from asymptomatic (where the diagnosis may only come about adventitiously upon examination of a blood film) to severe hemolytic anemia. A related condition, hereditary pyropoikilocytosis (HPP), is in effect an aggravated form of HE. So, how do mutations in a single gene give rise to such a wide spectrum of outcomes?
It is more than 2 decades since spectrin mutations were first associated with HE. Since then, numerous mutations in SPTA1 have been identified in cases of HE and HPP.1 Many of these change an amino acid at the αI-spectrin site that binds to βI-spectrin in the formation of spectrin tetramers. Spectrin tetramers are the functional units that provide resistance to shear stresses in circulation.2 Gaetani and colleagues engineered 14 different mutations into recombinant fragments of αI-spectrin (see figure). They then used microcalorimetry, an exquisitely sensitive technique that measures the heat changes associated with binding between proteins, to quantify the binding of the mutants to fragments of βI-spectrin. Their results indicate that different mutations have very different effects on affinity. For example, changing arginine 34 to tryptophan (R34W) has little or no effect on affinity of interaction. In contrast, 5 other mutants completely lost detectable binding activity. The remaining mutations exhibited reductions in affinity, but not complete loss of binding. Gaetani et al also analyzed the recombinant proteins for evidence of gross structural changes, and found none. They concluded that HE and HPP arising from these mutations result from changes in molecular recognition between spectrin subunits rather than structural alterations.
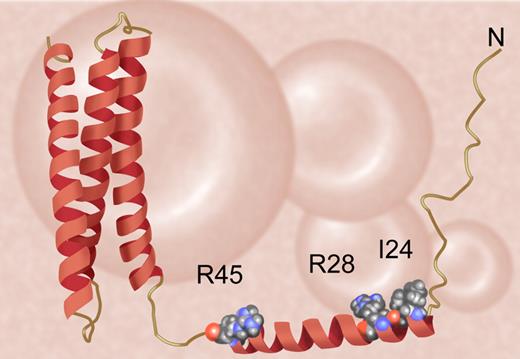
The structure of the N-terminal region of αI-spectrin. The figure is drawn from Protein Databank entry 1OWA. The first helix of αI-spectrin interacts with β in forming spectrin tetramers. In the accompanying paper, Gaetani et al describe the mechanisms by which mutations in residues I24, R28, and R45 (among others) cause hereditary elliptocytosis. In the cases of the residues indicated, pathogenic mutations eliminate interaction with β-spectrin. Illustration by Anthony Baines and Debra Tyler.
The structure of the N-terminal region of αI-spectrin. The figure is drawn from Protein Databank entry 1OWA. The first helix of αI-spectrin interacts with β in forming spectrin tetramers. In the accompanying paper, Gaetani et al describe the mechanisms by which mutations in residues I24, R28, and R45 (among others) cause hereditary elliptocytosis. In the cases of the residues indicated, pathogenic mutations eliminate interaction with β-spectrin. Illustration by Anthony Baines and Debra Tyler.
One of the intriguing questions raised by the current study is whether mutations such as R34W, which cause little or no change in molecular recognition and yet are associated with the disease, are actually pathogenic. The authors suggest that perhaps their assay does not detect all the critical changes in molecular activity. For instance, the R34W mutation was originally found in trans with a low expression polymorphism, αLELY. The combined mutations might sufficiently reduce spectrin activity in situ to produce HE. Alternatively (or in addition), there may be further mutations that were not picked up in the original analyses of the patients concerned.
The data reported here also contrast with a separate case of HE analyzed by Johnson et al3 in another recent paper in Blood. In this case, the pathogenic mutation was not in the tetramerization site, but was located much further away in the body of the αI-spectrin polypeptide. The effect of the mutation was revealed in the stability of protein folding. So, HE/HPP can arise from more than one class of mechanism.
Gaetani et al conclude that mutations that abolish binding of α-spectrin to β-spectrin are at sites highly conserved across all spectrins, even in simple invertebrates. In this respect, the red-cell membrane continues to live up to its traditional role of illuminating processes essential to the function of membranes in all animals.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal