Abstract
We have prospectively evaluated the biologic response to desmopressin in 77 patients with type 1 von Willebrand disease (VWD) enrolled within the Molecular and Clinical Markers for the Diagnosis and Management of type 1 VWD project. Complete response to desmopressin was defined as an increase of both ristocetin cofactor activity (VWF:RCo) and factor VIII coagulant activity (FVIII:C) to 50 IU/dL or higher and partial response as VWF:RCo or FVIII:C lower than 50 IU/dL after infusion, but at least 3-fold the basal level. Complete response was observed in 83% of patients; partial in 13%; and no response in 4%. Patients with some abnormality of VWF multimeric pattern had significantly lower basal FVIII:C and VWF, lower VWF:RCo/Ag ratio, and less complete responses to desmopressin than patients with a normal multimeric pattern (P = .002). Patients with mutations at codons 1130 and 1205 in the D′-D3 domain had the greatest relative increase, but shortest FVIII and VWF half-lives after infusion. Most partial and nonresponsive patients had mutations in the A1-A3 domains. Response to desmopressin in these VWD patients seemed to be associated with the location of the causative mutation. The presence of subtle multimeric abnormalities did not hamper potential clinically useful responses, as in typical type 1 VWD.
Introduction
Treatment or prevention of bleeding episodes in von Willebrand disease (VWD), the most common inherited bleeding disorder,1,2 is achieved by normalizing the level of functional von Willebrand factor (VWF) and of coagulation factor VIII (FVIII), either by stimulating their endogenous release from endothelial cells with desmopressin (1-desamino-8-d arginine vasopressin, DDAVP) or by infusion of plasma-derived FVIII and VWF concentrate.3 Desmopressin acts as a specific agonist for the vasopressin V2 receptor and induces secretion of VWF from endothelial cells by binding to V2 receptors on cell membranes and by activating cyclic adenosine monophosphate (c-AMP)–mediated signaling.4 Most patients with type 1 VWD respond to desmopressin, whereas few with type 2 VWD (due to functional deficiencies in VWF) and none with type 3 VWD (due to lack of VWF) are expected to respond.3,5 The increase of VWF and FVIII is generally 2- to 4-fold, but may be much higher.3,6,7 Although most type 1 patients have a mild phenotype and respond well to desmopressin, a large subgroup of those with a more severe phenotype are nonresponders.8 Even though a major genetic influence is expected as the response is individual and tends to be of the same magnitude from one occasion to another,9 the relationship between desmopressin response and a particular genetic background has not been systematically investigated. Recent data indicate that some mutations in the VWF gene (VWF) may affect both the magnitude and the duration of the response to desmopressin.10-13
A recent multicenter European study, Molecular and Clinical Markers for the Diagnosis and Management of Type 1 von Willebrand disease (MCMDM-1VWD) (http://www.euvwd.group.shef.ac.uk/), studied a large cohort of patients with VWD type 1 from 9 European countries. According to the phenotypic and genotypic results,14 3 different groups of patients were identified: group 1: patients with an abnormal plasma VWF multimeric pattern, with or without an identified mutation; group 2: patients with normal multimers and an identified mutation; and group 3: patients with normal multimers and no identified mutation.14
As a part of the project, we undertook a prospective study on desmopressin responsiveness. The main aim was to gain information about the pathophysiologic consequences of different type 1 mutations by studying the pattern of response to desmopressin according to the basal VWF multimeric pattern and the location of the mutations in VWF.
Methods
Study design
The MCMDM-1VWD study was an EU-funded survey on type 1 VWD (Goodeve et al14 ; Tosetto et al15 ; Eikenboom et al16 ; and http://www.euvwd.group.shef.ac.uk for further details). Twelve VWD treatment centers in 9 European countries participated in the study. Partner numbers (P) were as follows: P1, Sheffield, United Kingdom; P2, Vicenza, Italy; P3, Milano, Italy; P4, La Coruna, Spain; P5, Paris and Lille, France; P6, Leiden, The Netherlands; P7, Hamburg, Germany; P8, Aarhus, Denmark; P9, Prague, Czech Republic; P10, Malmo, Sweden; P11, Leicester, United Kingdom; P12, Birmingham United Kingdom. The study aimed at recruiting the full spectrum of type 1 VWD families including milder cases to mimic the clinical situation as much as possible and not to have bias toward the more severe, highly penetrant type 1 VWD. One hundred fifty-four families historically diagnosed to have type 1 VWD by their treatment center were recruited into the study. Each comprised an index case (IC) with VWD, at least one further affected family member (AFM), plus unaffected family members (UFMs).
Desmopressin test
The protocol was submitted and approved by local Internal Review Boards, according to the rules present in each country. Informed signed consent was obtained from each patient in accordance with the Declaration of Helsinki. The test was undertaken by index cases or, when indicated, by an affected family member.
Desmopressin was administered at 0.3 μg/kg body weight either by subcutaneous or intravenous route (in this case, the compound was diluted in 50 to 100 mL isotonic saline and infused over 30 minutes). The time of sampling was scheduled taking the time of subcutaneous injection or the beginning of intravenous infusion as time 0. Plasma samples were obtained prior to infusion and at 60, 120, and 240 minutes after administration of desmopressin from at least one affected member of each family, preferably the index case. For some pediatric patients, 240-minute samples were not obtained.
Laboratory methods
Venous blood anticoagulated with 0.109 M sodium citrate (1:9 vol/vol) was centrifuged at 2500g for 15 minutes and platelet-poor plasma aliquoted and stored at −80°C. Factor VIII procoagulant activity (FVIII:C), von Willebrand factor antigen (VWF:Ag), and ristocetin cofactor activity (VWF:RCo) were measured as previously described15 at each individual center and the results were centrally confirmed by P2 on aliquoted, frozen plasma samples shipped on dry ice. Values obtained in the central laboratory were used for all calculations reported in the present paper. Platelet count was checked at baseline and at 60 and 240 minutes to identify unrecognized type 2B VWD cases. The plasma VWF multimeric pattern was analyzed by P7, as previously described.14 Plasma VWF:RCo/VWF:Ag before and at peak were calculated. The mean ratio in 1155 healthy controls was 1.02 plus or minus 0.26 (range, 0.43-2.78). The 2.5 percentile was 0.59, which was used as the lower reference limit for analysis.
Definition of biologic response to desmopressin
Patients were defined as follows: complete responders: both VWF:RCo and FVIII:C were 50 IU/dL or higher after desmopressin; partial responders: VWF:RCo or FVIII:C were lower than 50 IU/dL but increased at least 3-fold; and nonresponders: neither criterion. Patients with VWF:RCo and/or FVIII:C 50 IU/dL or higher at baseline at time of testing (16 patients) were considered as complete responders if a level of 100 IU/dL or higher was reached for both measurements.
Statistical analysis
Differences in frequencies among subgroups were tested using the Fisher exact test; differences of median values were tested using the nonparametric median test or one-way analysis of variance (ANOVA) with Scheffe adjustment for multicomparison tests when required. Interquartile (IQ) ranges were calculated as the range spanning from 25th to 75th.
For pharmacokinetic analysis, we computed both the elimination half-lives (t1/2) and area under the curve (AUC) of VWF and FVIII:C measurements. Because only 4 measurements were available for most patients (at times 0, 60, 120, and 240 minutes), a classical 2-compartment model could not be fitted to our data. Therefore, t1/2 and AUC were computed by approximating the kinetic model to a simple exponential decay, using the 3 times after desmopressin (60, 120, and 240 minutes) to fit the exponential curve in each patient. Subsequently, in each patient the AUC and t1/2 were computed from time 0 to infinite using the fitted exponential curve. For those subjects in whom only 3 measurements were available (times 0, 60, and 120), only AUCs but not half-lives could be computed and are reported. All pharmacokinetic measures (including fitting of the exponential curve for each patient) were computed using the pharmacokinetic procedures of the Stata software package (Stata 9.0; StataCorp, College Station, TX). Differences in median values of AUC or half-lives were computed using the nonparametric Mann-Whitney test.
Results
Table 1 reports the characteristics of the investigated subjects. A total of 77 patients (age range: 6-75 years) were tested in 8 different centers. In 4 centers, patients were not enrolled for ethical reasons. Median FVIII:C and VWF and VWF:RCo/VWF:Ag ratio were significantly lower in patients with an abnormal multimeric pattern, while no difference was observed between patients with normal multimeric pattern with or without an identified mutation. Patients with no mutations identified were significantly younger, while no difference was observed in blood group representation among the 3 groups. Mutations in VWF were identified in 58 (71.1%) of 77 patients: 47 patients had 1 mutation, 10 patients had 2 mutations, and 1 patient had 3 mutations.
Baseline characteristics of investigated subjects
| . | Group 1: abnormal VWF multimers, n = 34 . | Group 2: normal VWF multimers and a mutation, n = 27 . | Group 3: normal VWF multimers and no mutation, n = 16 . | P* . |
|---|---|---|---|---|
| Male/female | 12/22 | 13/14 | 4/12 | .29 |
| Median age, y (range) | 40.5 (13-75) | 37 (6-67) | 27.5 (6-64) | .05 |
| Blood group O (%) | 18 (52.9) | 13 (48.1) | 13 (81.2) | .08 |
| Median VWF:RCo, IU/dL (IQ range) | 9.5 (15) | 52 (17) | 51.5 (20.5) | <.001 |
| Median VWF:Ag, IU/dL (IQ range) | 16 (18) | 52 (30) | 50 (24.5) | <.001 |
| Median FVIII:C, IU/dL (IQ range) | 24 (28) | 74 (46) | 70 (33) | <.001 |
| Mean VWF:RCo/VWF:Ag ratio (IQ range) | 0.67 (0.45) | 1.02 (0.28) | 1.06 (0.34) | .001 |
| Identified mutations, no. | ||||
| None | 3 | 0 | 16 | NA |
| One | 24 | 23 | 0 | NA |
| Two | 7† | 3 | 0 | NA |
| Three | 0 | 1 | 0 | NA |
| . | Group 1: abnormal VWF multimers, n = 34 . | Group 2: normal VWF multimers and a mutation, n = 27 . | Group 3: normal VWF multimers and no mutation, n = 16 . | P* . |
|---|---|---|---|---|
| Male/female | 12/22 | 13/14 | 4/12 | .29 |
| Median age, y (range) | 40.5 (13-75) | 37 (6-67) | 27.5 (6-64) | .05 |
| Blood group O (%) | 18 (52.9) | 13 (48.1) | 13 (81.2) | .08 |
| Median VWF:RCo, IU/dL (IQ range) | 9.5 (15) | 52 (17) | 51.5 (20.5) | <.001 |
| Median VWF:Ag, IU/dL (IQ range) | 16 (18) | 52 (30) | 50 (24.5) | <.001 |
| Median FVIII:C, IU/dL (IQ range) | 24 (28) | 74 (46) | 70 (33) | <.001 |
| Mean VWF:RCo/VWF:Ag ratio (IQ range) | 0.67 (0.45) | 1.02 (0.28) | 1.06 (0.34) | .001 |
| Identified mutations, no. | ||||
| None | 3 | 0 | 16 | NA |
| One | 24 | 23 | 0 | NA |
| Two | 7† | 3 | 0 | NA |
| Three | 0 | 1 | 0 | NA |
NA, indicates not applicable.
Tests difference among the 3 groups.
Including 3 patients with R1205H/M740I changes.
Overall biologic response to desmopressin
Overall median maximum relative increases after desmopressin were 3.2-fold (range: 1.3- to 53.7-fold) for VWF:RCo, 2.7-fold (range: 1.3- to 16-fold; missing VWF:Ag value for the highest VWF:RCo responder) for VWF:Ag, and 3.7-fold (range: 1.2- to 21.7-fold) for FVIII:C. Complete response was observed in 64 (83%) of 77, partial response in 10 (13%) of 77, and no response in 3 (4%) of 77 patients. On average, basal FVIII:C and VWF were significantly higher in patients who achieved complete response (Table 2). There was no difference in type of response between the 11 patients younger than 16 years and the 66 patients 16 years or older (P = .68).
Characteristics of response to desmopressin according to the presence of abnormal or normal basal multimeric pattern and presence of mutation
| . | Complete response, n = 64 . | Partial response, n = 10 . | No response, n = 3 . | P* . |
|---|---|---|---|---|
| Male/female | 25/39 | 3/7 | 1/2 | .88 |
| Median age, y (range) | 38 (6-67) | 41 (13-62) | 49 (21-75) | .61 |
| Blood group O (%) | 36 (56.2) | 7 (70.0) | 1 (33.3) | .55 |
| Median VWF:RCo, IU/dL (interquartile range) | 44.5 (31) | 7 (8) | 3 (13) | .001 |
| Median VWF:Ag, IU/dL (interquartile range) | 44 (34) | 15 (7) | 17 (7) | .004 |
| Median FVIII:C, IU/dL (interquartile range) | 53 (54) | 23 (6) | 28 (44) | .007 |
| Mean VWF:RCo/VWF:Ag ratio (interquartile range) | 0.94 (0.39) | 0.52 (0.63) | 0.22 (0.82) | .005 |
| Groups | .002 | |||
| 1: Abnormal VWF multimers (%) | 22 (64.7) | 9 (26.4) | 3 (8.8) | — |
| 2: Normal VWF multimers and a mutation (%) | 26 (96.3) | 1 (3.7) | 0 (0) | — |
| 3: Normal VWF multimers and no mutation (%) | 16 (100) | 0 (0) | 0 (0) | — |
| Identified mutations, no. | .70 | |||
| None | 18 | 1 | 0 | — |
| One | 37 | 8 | 2 | — |
| Two | 8 | 1 | 1 | — |
| Three | 1 | 0 | 0 | — |
| . | Complete response, n = 64 . | Partial response, n = 10 . | No response, n = 3 . | P* . |
|---|---|---|---|---|
| Male/female | 25/39 | 3/7 | 1/2 | .88 |
| Median age, y (range) | 38 (6-67) | 41 (13-62) | 49 (21-75) | .61 |
| Blood group O (%) | 36 (56.2) | 7 (70.0) | 1 (33.3) | .55 |
| Median VWF:RCo, IU/dL (interquartile range) | 44.5 (31) | 7 (8) | 3 (13) | .001 |
| Median VWF:Ag, IU/dL (interquartile range) | 44 (34) | 15 (7) | 17 (7) | .004 |
| Median FVIII:C, IU/dL (interquartile range) | 53 (54) | 23 (6) | 28 (44) | .007 |
| Mean VWF:RCo/VWF:Ag ratio (interquartile range) | 0.94 (0.39) | 0.52 (0.63) | 0.22 (0.82) | .005 |
| Groups | .002 | |||
| 1: Abnormal VWF multimers (%) | 22 (64.7) | 9 (26.4) | 3 (8.8) | — |
| 2: Normal VWF multimers and a mutation (%) | 26 (96.3) | 1 (3.7) | 0 (0) | — |
| 3: Normal VWF multimers and no mutation (%) | 16 (100) | 0 (0) | 0 (0) | — |
| Identified mutations, no. | .70 | |||
| None | 18 | 1 | 0 | — |
| One | 37 | 8 | 2 | — |
| Two | 8 | 1 | 1 | — |
| Three | 1 | 0 | 0 | — |
— indicates not applicable.
Tests difference among the 3 groups.
Response according to baseline multimeric pattern
Response to desmopressin was evaluated according to the 3 dif-ferent groups of patients previously identified: group 1: patients with abnormal multimers (n = 34); group 2: patients with normal multimers and a mutation (n = 27); and group 3: patients with normal multimers and no mutation (n = 16) (Table 2).
Patients with normal multimers had a median relative VWF:RCo increase of 2.6 (range: 1.3-10.3). The VWF:RCo increase did not differ between patients with normal multimers and a mutation (2.8; range: 1.3-10.3), and those with normal multimers and no mutation (2.5; range: 1.8-4.0).
Patients with basal abnormal multimers had a VWF:RCo increase of 6.5 (range: 1.7-53.7). Most of them (31/34) had a detected mutation. If patients with mutations C1130F/G/R and R1205H were excluded, the remaining patients with abnormal multimers (n = 21) had a median maximal VWF:RCo increase of 3.5 (range: 1.7-13.7).
Patients with an abnormal basal VWF multimeric pattern had significantly fewer complete responses due to their lower basal levels and 12 of 13 patients with partial9 or no response3 belonged to this group (P = .002 by Fisher exact test). Ten of these 12 had an abnormal basal VWF:RCo/VWF:Ag that normalized after desmopressin administration in 5 of 10 patients.
The analysis of multimeric pattern showed that ultralarge VWF multimers appeared after desmopressin administration in approximately 80% of patients with a slight decrease of basal high-molecular-weight multimers and/or a smeary pattern and abnormal VWF:RCo/Ag (Figure 1). Furthermore, the smeary pattern associated with the lack of subbands was transiently corrected after infusion in most patients, regardless of the location of the mutation (data not shown).
Multimeric pattern (medium resolution gel) of plasma VWF and densitometric scan of multimeric profile before and after desmopressin in a patient with C1130G mutation. Black = normal plasma; red = time 0; blue = time 60 minutes; green = time 120 minutes; and magenta = time 240 minutes. All the multimers are present, although the largest are relatively decreased (red), with increased smaller multimer concentrations. After desmopressin, an increase of the largest forms but also of the smaller forms is observed, with progressive return to basal pattern (increased clearance).
Multimeric pattern (medium resolution gel) of plasma VWF and densitometric scan of multimeric profile before and after desmopressin in a patient with C1130G mutation. Black = normal plasma; red = time 0; blue = time 60 minutes; green = time 120 minutes; and magenta = time 240 minutes. All the multimers are present, although the largest are relatively decreased (red), with increased smaller multimer concentrations. After desmopressin, an increase of the largest forms but also of the smaller forms is observed, with progressive return to basal pattern (increased clearance).
Response according to the location of mutations
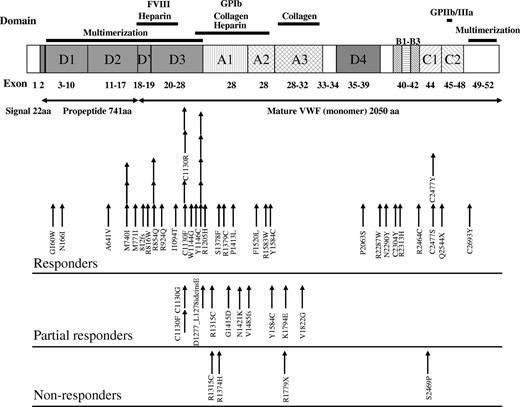
Table 3 and Figure 2 summarize responses to desmopressin according to the location of mutations. All the patients with mutations in D1-D2 and D4-CK domains and type 2N and intronic/promoter mutations responded completely. There were complete, partial, and nonresponders with mutations in domains D3 and A1-A3. Patients with C1130F/G/R mutations were either complete (n = 5) or partial (n = 2) responders. There was both a partial and a nonresponder with R1315C.
Desmopressin response and FVIII and VWF measurements before and at peak level by VWF domain
| Domain location and type of mutation . | No. of responsive patients/total . | FVIII:C, IU/dL, mean±SD . | VWF:RCo, IU/dL, mean±SD . | VWF:RCo/Ag, mean±SD . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before . | Peak . | Fold increase . | Before . | Peak . | Fold increase . | Before . | Abn/N* . | Peak . | Abn/N . | ||
| D1-D2 | 3/3 | 59 ± 29 | 144 ± 67 | 2.5 ± 0.4 | 52 ± 31 | 120 ± 70 | 2.4 ± 0.32 | 0.87 ± 0.33 | 1/2 | 0.89 ± 0.26 | 0/3 |
| G160W | 1/1 | 56 | 119 | 2.1 | 25 | 68 | 2.3 | 0.54 | 1/0 | 0.68 | 0/1 |
| N166I | 1/1 | 90 | 220 | 2.4 | 44 | 92 | 2.1 | 1.19 | 0/1 | 0.8 | 0/1 |
| A641V | 1/1 | 32 | 98 | 2.9 | 86 | 200 | 2.3 | 0.88 | 0/1 | 1.18 | 0/1 |
| D′-D3 | 14/16 | 20 ± 21§ | 138 ± 75 | 9.7 ± 5.9∥ | 10 ± 16∥ | 87 ± 36 | 18.1 ± 11.7∥ | 0.46 ± 0.23 | 12/4 | 0.92 ± 0.25 | 1/15 |
| M771I | 1/1 | 31 | 112 | 3.6 | 22 | 101 | 4.6 | 0.65 | 0/1 | 0.96 | 0/1 |
| I1094T | 1/1 | 93 | 324 | 3.5 | 65 | 144 | 2.2 | 0.91 | 0/1 | 0.83 | 0/1 |
| C1130F/G/R (range) | 5/7 | 17 ± 9 (1.5-26) | 118 ± 62 (13-183) | 7.1 ± 2 (5.1-10.5) | 5 ± 4 (3-14) | 73 ± 29 (44-123) | 17.1 ± 5.1 (7.4-23) | 0.31 ± 0.16 (0.13-0.64) | 6/1 | 0.87 ± 0.33 (0.56-1.54) | 1/6 |
| W1144G | 1/1 | 22 | 137 | 6.2 | 16 | 101 | 6.3 | 0.48 | 1/0 | 0.91 | 0/1 |
| R1205H† (range) | 6/6 | 10 ± 3 (7-16) | 136 ± 32 (109-195) | 15.3 ± 5.9 (6.9-21.7) | 4 ± 2 (3-7) | 89 ± 42 (53-161) | 26 ± 14 (16.9-53.7) | 0.53 ± 0.19 (0.33-0.87) | 5/1 | 1 ± 0.22 (0.7-1.3) | 0/6 |
| A1-A3 | 6/14 | 46 ± 28 | 125 ± 58 | 3.1 ± 1 | 27 ± 29 | 75 ± 62 | 4 ± 2.1 | 0.54 ± 0.37 | 8/6 | 0.81 ± 0.48 | 5/9 |
| D1277 L1278delinsE | 0/1 | 36 | 109 | 3 | 3 | 15 | 5 | 0.17 | 1/0 | 0.36 | 1/0 |
| R1315C (range) | 1/3 | 24 ± 6 (17-28) | 82 ± 19 (67-103) | 3.5 ± 0.7 (2.7-4) | 11 ± 8 (3-18) | 42 ± 34 (12-79) | 4 ± 2.6 (2-7.2) | 0.58 ± 0.41 (0.19-1) | 2/1 | 1 ± 0.65 (0.31-1.58) | 1/2 |
| R1374H | 0/1 | 73 | 213 | 2.9 | 18 | 34 | 1.9 | 0.22 | 1/0 | 0.18 | 1/0 |
| R1379C | 1/1 | 107 | 266 | 2.5 | 53 | 176 | 3.3 | 0.9 | 0/1 | 1.4 | 0/1 |
| P1413L | 1/1 | 54 | 111 | 2.1 | 31 | 87 | 2.8 | 0.67 | 0/1 | 0.93 | 0/1 |
| G1415D | 0/1 | 23 | 106 | 4.6 | 3 | 18 | 6 | 0.13 | 1/0 | 0.31 | 1/0 |
| N1421K | 0/1 | 30 | 142 | 4.7 | 3 | 31 | 10.3 | 0.11 | 1/0 | 0.48 | 1/0 |
| F1520L | 1/1 | 68 | 183 | 2.7 | 91 | 200 | 2.2 | 0.98 | 0/1 | 1.2 | 0/1 |
| R1583W | 1/1 | 31 | 97 | 3.1 | 48 | 130 | 2.7 | 0.92 | 0/1 | 0.91 | 0/1 |
| Y1584C | 1/1 | 91 | 113 | 1.2 | 75 | 136 | 1.8 | 0.94 | 0/1 | 1.36 | 0/1 |
| K1794E | 0/1 | 25 | 83 | 3.3 | 6 | 38 | 3.3 | 0.29 | 1/0 | 0.73 | 0/1 |
| V1822G | 0/1 | 37 | 79 | 2.1 | 16 | 48 | 3 | 0.55 | 1/0 | 0.8 | 0/1 |
| C2304Y | 1/1 | 150 | 300 | 2 | 54 | 86 | 1.6 | 0.79 | 0/1 | 0.85 | 0/1 |
| R2313H | 1/1 | 92 | 249 | 2.7 | 73 | 136 | 1.9 | 0.86 | 0/1 | 0.85 | 0/1 |
| R2464C | 1/1 | 44 | 167 | 3.8 | 34 | 120 | 3.5 | 1 | 0/1 | 0.94 | 0/1 |
| C2477Y/S | 2/2 | 43-58 | 61-300 | 1.4-5.2 | 33-35 | 87-89 | 2.5-2.7 | 0.86-1.25 | 0/2 | 0.88-1.24 | 0/2 |
| Q2520P | 1/1 | 45 | 236 | 5.2 | 18 | 122 | 6.8 | 0.78 | 0/1 | 1.04 | 0/1 |
| Q2544X | 1/1 | 75 | 214 | 2.9 | 35 | 124 | 3.5 | 1.35 | 0/1 | 1.35 | 0/1 |
| C2693Y | 1/1 | 41 | 119 | 2.9 | 29 | 88 | 3 | 0.57 | 1/0 | 0.87 | 0/1 |
| Domain location and type of mutation . | No. of responsive patients/total . | FVIII:C, IU/dL, mean±SD . | VWF:RCo, IU/dL, mean±SD . | VWF:RCo/Ag, mean±SD . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before . | Peak . | Fold increase . | Before . | Peak . | Fold increase . | Before . | Abn/N* . | Peak . | Abn/N . | ||
| D1-D2 | 3/3 | 59 ± 29 | 144 ± 67 | 2.5 ± 0.4 | 52 ± 31 | 120 ± 70 | 2.4 ± 0.32 | 0.87 ± 0.33 | 1/2 | 0.89 ± 0.26 | 0/3 |
| G160W | 1/1 | 56 | 119 | 2.1 | 25 | 68 | 2.3 | 0.54 | 1/0 | 0.68 | 0/1 |
| N166I | 1/1 | 90 | 220 | 2.4 | 44 | 92 | 2.1 | 1.19 | 0/1 | 0.8 | 0/1 |
| A641V | 1/1 | 32 | 98 | 2.9 | 86 | 200 | 2.3 | 0.88 | 0/1 | 1.18 | 0/1 |
| D′-D3 | 14/16 | 20 ± 21§ | 138 ± 75 | 9.7 ± 5.9∥ | 10 ± 16∥ | 87 ± 36 | 18.1 ± 11.7∥ | 0.46 ± 0.23 | 12/4 | 0.92 ± 0.25 | 1/15 |
| M771I | 1/1 | 31 | 112 | 3.6 | 22 | 101 | 4.6 | 0.65 | 0/1 | 0.96 | 0/1 |
| I1094T | 1/1 | 93 | 324 | 3.5 | 65 | 144 | 2.2 | 0.91 | 0/1 | 0.83 | 0/1 |
| C1130F/G/R (range) | 5/7 | 17 ± 9 (1.5-26) | 118 ± 62 (13-183) | 7.1 ± 2 (5.1-10.5) | 5 ± 4 (3-14) | 73 ± 29 (44-123) | 17.1 ± 5.1 (7.4-23) | 0.31 ± 0.16 (0.13-0.64) | 6/1 | 0.87 ± 0.33 (0.56-1.54) | 1/6 |
| W1144G | 1/1 | 22 | 137 | 6.2 | 16 | 101 | 6.3 | 0.48 | 1/0 | 0.91 | 0/1 |
| R1205H† (range) | 6/6 | 10 ± 3 (7-16) | 136 ± 32 (109-195) | 15.3 ± 5.9 (6.9-21.7) | 4 ± 2 (3-7) | 89 ± 42 (53-161) | 26 ± 14 (16.9-53.7) | 0.53 ± 0.19 (0.33-0.87) | 5/1 | 1 ± 0.22 (0.7-1.3) | 0/6 |
| A1-A3 | 6/14 | 46 ± 28 | 125 ± 58 | 3.1 ± 1 | 27 ± 29 | 75 ± 62 | 4 ± 2.1 | 0.54 ± 0.37 | 8/6 | 0.81 ± 0.48 | 5/9 |
| D1277 L1278delinsE | 0/1 | 36 | 109 | 3 | 3 | 15 | 5 | 0.17 | 1/0 | 0.36 | 1/0 |
| R1315C (range) | 1/3 | 24 ± 6 (17-28) | 82 ± 19 (67-103) | 3.5 ± 0.7 (2.7-4) | 11 ± 8 (3-18) | 42 ± 34 (12-79) | 4 ± 2.6 (2-7.2) | 0.58 ± 0.41 (0.19-1) | 2/1 | 1 ± 0.65 (0.31-1.58) | 1/2 |
| R1374H | 0/1 | 73 | 213 | 2.9 | 18 | 34 | 1.9 | 0.22 | 1/0 | 0.18 | 1/0 |
| R1379C | 1/1 | 107 | 266 | 2.5 | 53 | 176 | 3.3 | 0.9 | 0/1 | 1.4 | 0/1 |
| P1413L | 1/1 | 54 | 111 | 2.1 | 31 | 87 | 2.8 | 0.67 | 0/1 | 0.93 | 0/1 |
| G1415D | 0/1 | 23 | 106 | 4.6 | 3 | 18 | 6 | 0.13 | 1/0 | 0.31 | 1/0 |
| N1421K | 0/1 | 30 | 142 | 4.7 | 3 | 31 | 10.3 | 0.11 | 1/0 | 0.48 | 1/0 |
| F1520L | 1/1 | 68 | 183 | 2.7 | 91 | 200 | 2.2 | 0.98 | 0/1 | 1.2 | 0/1 |
| R1583W | 1/1 | 31 | 97 | 3.1 | 48 | 130 | 2.7 | 0.92 | 0/1 | 0.91 | 0/1 |
| Y1584C | 1/1 | 91 | 113 | 1.2 | 75 | 136 | 1.8 | 0.94 | 0/1 | 1.36 | 0/1 |
| K1794E | 0/1 | 25 | 83 | 3.3 | 6 | 38 | 3.3 | 0.29 | 1/0 | 0.73 | 0/1 |
| V1822G | 0/1 | 37 | 79 | 2.1 | 16 | 48 | 3 | 0.55 | 1/0 | 0.8 | 0/1 |
| C2304Y | 1/1 | 150 | 300 | 2 | 54 | 86 | 1.6 | 0.79 | 0/1 | 0.85 | 0/1 |
| R2313H | 1/1 | 92 | 249 | 2.7 | 73 | 136 | 1.9 | 0.86 | 0/1 | 0.85 | 0/1 |
| R2464C | 1/1 | 44 | 167 | 3.8 | 34 | 120 | 3.5 | 1 | 0/1 | 0.94 | 0/1 |
| C2477Y/S | 2/2 | 43-58 | 61-300 | 1.4-5.2 | 33-35 | 87-89 | 2.5-2.7 | 0.86-1.25 | 0/2 | 0.88-1.24 | 0/2 |
| Q2520P | 1/1 | 45 | 236 | 5.2 | 18 | 122 | 6.8 | 0.78 | 0/1 | 1.04 | 0/1 |
| Q2544X | 1/1 | 75 | 214 | 2.9 | 35 | 124 | 3.5 | 1.35 | 0/1 | 1.35 | 0/1 |
| C2693Y | 1/1 | 41 | 119 | 2.9 | 29 | 88 | 3 | 0.57 | 1/0 | 0.87 | 0/1 |
Mutations in italics are associated with abnormal multimeric pattern.
Abnormal/normal ratio (>0.59).
Patients with additional M740I change were included in this group since basal and peak levels for FVIII:C and VWF:RCo were similar to those with R1205H.
Including 3 patients with basal abnormal VWF multimers
P < .05 versus no-mutations subgroup (all P values were adjusted for multicomparison tests).
P < .01 versus no-mutations subgroup (all P values were adjusted for multicomparison tests).
Distribution of mutations over the VWF protein for desmopressin responders, partial responders, and nonresponders. Each arrow represents one mutation. Intronic/promoter mutations are not shown (Table 3). Among the nonresponders, a single patient had 2 mutations (R1779X/S2469P). Among the partial responders, a patient was compound heterozygous for V1485fs/Y1584C.
Distribution of mutations over the VWF protein for desmopressin responders, partial responders, and nonresponders. Each arrow represents one mutation. Intronic/promoter mutations are not shown (Table 3). Among the nonresponders, a single patient had 2 mutations (R1779X/S2469P). Among the partial responders, a patient was compound heterozygous for V1485fs/Y1584C.
Most of the patients with partial (6/10: D1277 L1278delinsE, R1315C, G1415D, N1421K, K1794E, and V1822G) or no response (2/3: R1315C and R1374H) to desmopressin had mutations in A1-A3 domains, followed by 2 partial responders with mutations in D′-D3 domains (C1130F or C1130G) and 1 partial (V1485fs/Y1584C) and 1 nonresponder (R1779X/S2469S) in the group with more than one mutation. Only a single patient among those without a mutation identified had a partial response, but had basal abnormal multimers. Basal abnormal VWF:RCo/VWF:Ag (lower than the reference limit in healthy subjects of 0.59) was evident in 25 of 77 patients, while at peak only 6 of 77 patients still had an abnormal ratio: 4 of them had mutations in the A1-A3 domains (D1277 L1278delinsE, R1315C, R1374H, G1415D) and 1 had C1130G, all with abnormal multimers, while 1 had N1421K mutation and a normal basal multimeric pattern. Basal FVIII:C and VWF:RCo levels in D′-D3 patients were significantly lower compared with the other subgroups (P < .01 vs all). This finding was due mainly to the presence of patients with C1130F/G/R and R1205H mutations who form an almost separate subgroup with higher increases of VWF than other patients. Thus, the median relative increase of VWF:RCo was 17.6 (range: 7.4-23.0) for patients with C1130F/G/R mutations, and 20.3 (range: 16.9-53.7) for those with the R1205H mutation. The corresponding value for all other patients was 2.7 (range: 1.3-13.7). Likewise, basal VWF:RCo/VWF:Ag ratio was the lowest in these patients (12/16 abnormal) but it normalized in nearly all (1/16 abnormal at peak), with average levels indistinguishable from those of the patients with mutations in other domains.
Patients with enhanced response to desmopressin
Of the 13 patients with more than 10-fold increase of VWF:RCo, 12 had R1205H (3 with and 3 without a M740I change) or C1130F/G/R (n = 6) mutations in the D′-D3 domains. The patient with V1485fs/Y1584C had 13.7-fold increase. Of the 8 patients with a FVIII:C more than 10-fold over baseline at peak, 5 carried the VWD Vicenza mutation, 1 had C1130G, and 2 had type 2N genotypes (R854Q/R924Q and R816W).
Patients with shortened FVIII:C or VWF survival
The present study was not aimed at extensively evaluating all the pharmacokinetic characteristics of FVIII and VWF after desmopressin since in that case a prolonged sampling would have been required. However, even though mean residence time was not measurable confidently, we calculated the area under the curve (AUC) and half-life for FVIII and VWF (Table 4). Since we did not have a healthy control group, we contrasted the results obtained with different mutations to those of patients with normal multimers and no mutation. Overall, 21 patients showed a VWF:RCo half-life less than 4 hours, which could be roughly considered indicative of increased clearance. Fourteen had mutations in D′D3 (13 R1205H or C1130F/G/R, 1 W1144G), 3 in A1-A3 (R1315C, R1379C, K1794E) 3 had double mutations (Y1146C/S1378F, V1485fs/Y1584C, R2464C/Y1584C) and 1 had no mutation. Apart from K1794E, all had abnormal multimers.
FVIII:C and VWF AUC and half-lives after desmopressin
| . | Median AUC0, tmax, IU/dL/h (no. of patients) . | P* . | Median half-life, h (no. of patients) . | P . |
|---|---|---|---|---|
| VWF:RCo | ||||
| No mutation | 334.1 (19) | — | 12.0 (9) | — |
| 2 N | 372.7 (3) | .53 | 8.8 (2) | .15 |
| D1-D2 | 328.7 (3) | .58 | NM | NA |
| D4-CK | 305.1 (8) | .23 | 6.0 (6) | .39 |
| D′-D3 | 171.9 (16) | .04 | 1.4 (15) | <.001 |
| A1-A3 | 146.1 (14) | .04 | 7.4 (11) | .17 |
| Intronic | 130.0 (5) | .13 | NA | NA |
| Double mutations | 229.3 (9) | .22 | 2.7 (4) | .02 |
| VWF:Ag | ||||
| No mutation | 293.3 (19) | — | 10.8 (8) | — |
| 2 N | 368.7 (3) | .53 | 6.7 (2) | .11 |
| D1-D2 | 371.1 (3) | .53 | NM | NA |
| D4-CK | 345.6 (8) | .90 | 21.6 (6) | .03 |
| D′-D3 | 179.5 (16) | .01 | 2.1 (14) | <.001 |
| A1-A3 | 218.3 (14) | .05 | 9.6 (11) | .84 |
| Intronic | 165.3 (5) | .13 | NA | NA |
| Double mutations | 214.0 (9) | .04 | 4.2 (5) | .72 |
| FVIII:C | ||||
| No mutation | 486.8 (19) | — | 6.2 (9) | — |
| 2 N | 407.1 (3) | .53 | 3.4 (3) | .04 |
| D1-D2 | 442.6 (3) | .53 | NM | NA |
| D4-CK | 686.0 (8) | .07 | 5.4 (6) | .39 |
| D′-D3 | 317.4 (16) | .01 | 2.0 (15) | <.001 |
| A1-A3 | 298.0 (14) | .001 | 6.2 (11) | .65 |
| Intronic | 367.0 (5) | .61 | NA | NA |
| Double mutations | 379.0 (9) | .22 | 3.3 (5) | .09 |
| . | Median AUC0, tmax, IU/dL/h (no. of patients) . | P* . | Median half-life, h (no. of patients) . | P . |
|---|---|---|---|---|
| VWF:RCo | ||||
| No mutation | 334.1 (19) | — | 12.0 (9) | — |
| 2 N | 372.7 (3) | .53 | 8.8 (2) | .15 |
| D1-D2 | 328.7 (3) | .58 | NM | NA |
| D4-CK | 305.1 (8) | .23 | 6.0 (6) | .39 |
| D′-D3 | 171.9 (16) | .04 | 1.4 (15) | <.001 |
| A1-A3 | 146.1 (14) | .04 | 7.4 (11) | .17 |
| Intronic | 130.0 (5) | .13 | NA | NA |
| Double mutations | 229.3 (9) | .22 | 2.7 (4) | .02 |
| VWF:Ag | ||||
| No mutation | 293.3 (19) | — | 10.8 (8) | — |
| 2 N | 368.7 (3) | .53 | 6.7 (2) | .11 |
| D1-D2 | 371.1 (3) | .53 | NM | NA |
| D4-CK | 345.6 (8) | .90 | 21.6 (6) | .03 |
| D′-D3 | 179.5 (16) | .01 | 2.1 (14) | <.001 |
| A1-A3 | 218.3 (14) | .05 | 9.6 (11) | .84 |
| Intronic | 165.3 (5) | .13 | NA | NA |
| Double mutations | 214.0 (9) | .04 | 4.2 (5) | .72 |
| FVIII:C | ||||
| No mutation | 486.8 (19) | — | 6.2 (9) | — |
| 2 N | 407.1 (3) | .53 | 3.4 (3) | .04 |
| D1-D2 | 442.6 (3) | .53 | NM | NA |
| D4-CK | 686.0 (8) | .07 | 5.4 (6) | .39 |
| D′-D3 | 317.4 (16) | .01 | 2.0 (15) | <.001 |
| A1-A3 | 298.0 (14) | .001 | 6.2 (11) | .65 |
| Intronic | 367.0 (5) | .61 | NA | NA |
| Double mutations | 379.0 (9) | .22 | 3.3 (5) | .09 |
— indicates reference group; NM, half-life not measurable since peak occurred at 240 minutes; and NA, not available.
P value for the considered variable against the no-mutations subgroup.
As a whole, median AUC and half-life for VWF:RCo were significantly greater and longer in patients with a normal baseline multimeric pattern compared with those with basal VWF multimeric abnormalities (AUC: 328.7 IU/dL/h, IQ range: 167.4, vs 137.1 IU/dL/h, IQ range: 119, respectively; half-life: 9.3 hours, IQ range: 13 vs half-life: 2.5 hours, IQ range: 3.4, respectively; P < .001 for both parameters). As to VWF:RCo AUC, only patients with mutations in A1-A3 and D′-D3 domains had significantly smaller AUC, while VWF:RCo half-life was dramatically shorter in patients with D′-D3 mutations (P < .001) and to a lesser extent in those with double mutations (P < .02). As to VWF:Ag, D′-D3 and to a lesser extent double and A1-A3 mutations were significantly associated with smaller AUC, while again half-life was dramatically shorter in patients with D′-D3 mutations. Interestingly, a significantly prolonged half-life for VWF:Ag was observed in patients with D4-CK mutations compared with patients without mutation, even though the range was wide (3.6-38 hours). For FVIII:C, AUC was significantly smaller for mutations in the A1-A3 and D′-D3 domains, while half-life was again shortest in patients with D′-D3 mutations and significantly shorter in patients with mutations in FVIII-binding domain.
Half-lives could not be calculated for patients with mutations in the D1-D2 domains as peak levels were achieved at 240 minutes (data not shown).
Discussion
Desmopressin is considered the first-choice treatment for patients with VWD type 1. However, within this category, patients with heterogeneous phenotypes and genetic background are included, as recently demonstrated by the EU project, the Canadian project, and the UKCHDO study on type 1 VWD.14,17,18 Furthermore, not all patients with type 1 respond similarly to desmopressin and in patients with severe phenotypes the rates of favorable biologic response might be lower than expected.8
In this study, we evaluated the biologic response to desmopressin in the largest cohort of patients with well-characterized type 1 VWD so far published. Seventy-seven patients were recruited among those belonging to 154 families enrolled within the MCMDM-1VWD project.14
Overall, a complete response was observed in 83%, partial response in 13%, and no response in 4% of the patients. The median relative VWF:RCo increase was 3.2, but the range was wide (1.3-53.7). These results are similar to those obtained previously in a group of type 1 patients.8 Even after exclusion of patients with basal FVIII:C and VWF:RCo 50 IU/dL or higher, this figure did not change substantially and, thus, approximately 80% had a complete response according to the predefined criteria. The predefined response criteria reflect an approach potentially useful in a clinical setting. We therefore chose to use the achievement of peak levels of FVIII:C and VWF:RCo 50 IU/dL or higher to discriminate between complete response with likely good clinical utility and partial or no response. Previous studies in adults and children demonstrated that 26% to 80% of patients may respond, depending on the criteria adopted and the severity of the basal phenotype.8,19 Even a normal VWF:RCo/VWF:Ag, which suggests the presence of a true quantitative VWF defect, appeared not to guarantee a favorable response.8 However, a direct comparison of these results in type 1 VWD with ours is difficult since different inclusion criteria and definition of biologic response were used. However, unlike the study of Federici et al,8 but in keeping with our results (Table 2), greater baseline FVIII:C and VWF:RCo levels were significantly associated with positive desmopressin response in children.19 Importantly, the genetic background was not investigated in either of these studies.
According to the 3 groups of patients defined within the MCMDM-1VWD,14 the basal and peak FVIII:C and VWF:RCo were significantly lower in patients with an abnormal multimeric pattern, while no difference was observed between patients with normal multimers with or without a mutation (Table 1). Patients with an abnormal VWF:RCo/VWF:Ag ratio were clustered mainly in the group with abnormal multimers, who had a lower complete response rate (P = .002) (Table 2). Subtle abnormalities of plasma VWF multimeric pattern did not prevent a normalization of VWF:RCo/VWF:Ag ratio and of FVIII:C and VWF:RCo in the majority of patients, unlike typical type 2A VWD.8 This suggests that only major abnormalities (eg, lack of large or intermediate multimers as in typical type 2A and 2B variants) may adversely influence the likelihood of response in patients with VWD. This is also supported by the fact that most patients with abnormal multimers at baseline showed the appearance of the largest multimers after desmopressin or correction of an inner multimeric abnormality (eg, “smeary pattern”; Figure 1). The lack of appearance of the largest multimers in a few of these patients could be related to a fast proteolysis or insufficient sensitivity of multimeric analysis, while the “smeary” pattern could be clouded by the normal VWF released upon desmopressin from Weibel-Palade bodies. Whatever the explanation, a highly sensitive multimeric analysis technique, such as that used in the MCMDM1-VWD study, is probably not required in the clinical laboratory to predict desmopressin response.
The identification of the genetic background in most of our patients has allowed us, for the first time, to evaluate the pattern of response to desmopressin according to the location of the mutation (Table 3; Figure 2). From a general analysis of our results, some remarks can be made. 2 types of mutations, the C1130F/G/R and especially the R1205H (with or without M740I), accounted for much of the highest increases. These patients have been reported to have a brisk increase of FVIII:C and VWF,10,20 but reduced VWF survival. Patients with VWD Vicenza, previously included among type 2M cases, are now classified as type 1.21 Patients with VWD Vicenza and with C1130F have normal VWF platelet content,22,23 which has been considered an important predictor of a favorable response to desmopressin.24 Both the C1130F and the R1205H mutations may be characterized by increased intracellular retention of VWF, which may explain the very large immediate release of VWF after desmopressin administration.12,25 This may be corroborated by the fact that the relative FVIII increase, even though large, was only about half or less of the VWF increase. For other mutations, the relative increases of VWF and FVIII were of about the same magnitude. The location of the mutation in VWF is, however, not the only factor that determines the magnitude of response, as relatively large ranges were also seen for patients with the same type of mutation (eg, 7.4-23.0 relative VWF increase for patients with C1130F/G/R and 16.9-53.7 for those with R1205H).
All patients with single mutations in D1-D2 and D4-CK domains and all type 2N and intronic/promoter mutations responded completely. All partial and nonresponders had mutations in D3 and A1-A3 domains, except for the patient with S2469P in the C1 domain, who was, however, compound heterozygous for a null mutation. However, there were also patients with complete responses and mutations in domains D3 and A1-A3. Furthermore, there were both complete and partial responders among patients with C1130F/G/R mutations, as well as both a partial and a nonresponder with R1315C. Thus, no clear-cut distinction between complete, partial and nonresponders could be made on the basis of the location of the mutation alone.
Patients with R1315C and R1374H have been previously included among type 2M or 2A subtypes, and we confirm that these mutations are usually associated with a poor response to desmopressin (only 1 of 4 patients responded), as previously demonstrated.8 None of the patients with mutations in A1-A3 had thrombocytopenia after infusion (data not shown), further emphasizing that they are different from typical type 2B mutations.
The present study compares for the first time the AUC and half-lives of FVIII and VWF after desmopressin in well-characterized type 1 VWD patients with different mutations. As previously reported,10,12,13 a possible increased VWF clearance was suspected in patients with R1205H, C1130F/G/R, and W1144G. Similarly, an increased clearance was possibly present in R1315C, R1379C, and K1794E mutations in A1-A3, in 3 patients with double mutations (Y1146C/S1378F, V1485fs/Y1584C, R2464C/Y1584C), and in 1 with no mutation. Again, almost all had abnormal multimers, apart from K1794E. However, since we did not carry out the propeptide assay, which is a reliable indicator of VWF turnover along with VWF:Ag measurement,13 and a prolonged timing of sampling after desmopressin these results should be confirmed.
Only patients with A1-A3 mutations and to a greater extent those with D′-D3 mutations had significantly smaller AUCs for all the measurements, while patients with double mutations had significantly smaller AUC for VWF:Ag only (Table 4). As previously demonstrated,10,12,24 only patients with mutations in the D′-D3 domains had significantly shorter FVIII and VWF half-lives compared with patients without mutations, while those with double mutation did for VWF:RCo only. Interestingly, while as expected patients with reduced VWF-FVIII binding had shorter FVIII:C half-lives, patients with mutations in the D4-CK domains had longer VWF:Ag half-lives (Table 4). The latter finding could be related to interindividual differences in multimeric composition changes of the VWF released, but this remains to be demonstrated by expression studies. Similarly, the delayed peak level in patients with mutations in the D1-D2 domain, which did not allow the determination of half-lives, could be related to a reduced sensitivity to proteolysis or to a mechanism of a slow release of mutant VWF, but again no inference on the pathophysiology can be derived from the present results.
In conclusion, response to desmopressin in patients with a diagnosis of VWD type 1 is largely affected by the basal multimeric pattern and the specific type and location of mutations in VWF, since most partial and nonresponders were clustered in D3 and especially in A1-A3 domains. However, other factors are also of importance as there was some variability of responses between some patients with the same type of mutation. This again reinforces the need for performing a desmopressin test-infusion in any patient with clinically significant type 1 VWD to plan its future use. Our study also indicates that minor multimeric abnormalities and reduced VWF:RCo/VWF:Ag ratio do not prevent testing these patients for response to desmopressin. Establishing the optimal interval between repeated infusions would require additional ad hoc pharmacokinetic studies based on the different half-life of the released VWF.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank E. Jennings, M. Makris, H. Powell, M. Walker, L. Marsden, A. Al-Buhairan, S. Joyce, A. Bowyer, J. Anson, A. Cappelletti, M. Bernardi, K. Bertoncello, R. Bader, M. T. Canciani, F. Gianniello, A.-S. Ribba, A. Stephanian, L. Hilbert, C. Caron, E. Gomez, V. van Marion, J. Lambert, F. Oyen, T. Obser, K. Will, W. Eberl, G. Auerswald, E. Christiansen, E. Drewke, J. Suttnar, J. Dudlova, C. Watson, J. Warren, S. Mughal, W. Lester, S. Enayat, G. Surdhar, and P. Short for their contribution to this study.
This work was supported by The European Community under the Fifth Framework Programme (QLG1-CT-2000-00387).
Authorship
Contribution: All authors participated in study design, data collection, and performance of laboratory analyses; G.C., S.L., A.B.F., A.T., A.G., U.B., D.M., C.M., J.G., J.E., R.S., I.P., and F.R. analyzed and interpreted results; G.C. and S.L. wrote the paper; all authors checked the final version of the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Giancarlo Castaman, Department of Hematology, San Bortolo Hospital, 36100 Vicenza, Italy; e-mail: castaman@hemato.ven.it.
References
Author notes
G.C. and S.L. contributed equally to this paper.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal