Abstract
Expression of the arterial marker molecule ephrinB2 in endothelial cells is a prerequisite for adequate remodeling processes of the developing or angiogenic vasculature. Although its role in these processes has been extensively studied, the impact of ephrinB2 on the remodeling of adult arteries is largely unknown. To this end, we analyzed its expression during a biomechanically induced arteriolar remodeling process known as arteriogenesis and noted a significant increase in ephrinB2 expression under these conditions. By examining those biomechanical forces presumed to drive arteriogenesis, we identified cyclic stretch as a critical inducer of ephrinB2 expression in endothelial cells. Subsequent functional analyses in vitro revealed that endothelial cells expressing ephrinB2 limit the migration of smooth muscle cells, thereby enhancing segregation of both cell types. Moreover, MCP-1 induced transmigration of monocytes through a monolayer of endothelial cells overexpressing a truncated variant of ephrinB2 was clearly impeded. Taken together, these data suggest that expression of ephrinB2 in adult endothelial cells is up-regulated during arterial remodeling and controlled by cyclic stretch, a well-known inducer of such processes. This stretch-induced ephrinB2 expression may be pivotal for arteriogenesis as it limits smooth muscle cell migration within defined borders and controls monocyte extravasation.
Introduction
The ephrins comprise a family of membrane-associated ligands that bind to the largest family of receptor tyrosine kinases, the Eph receptors.1 EphrinB2 and EphB4 have been designated as the first marker molecules for arteriovenous differentiation with ephrinB2 expressed exclusively by arterial and EphB4 by venous endothelial cells. Deficiency of any of these molecules is incompatible with life. Thus, disruption of the corresponding genes in mice leads to comparable phenotypes with early embryonic lethality because of severe defects in arteriovenous remodeling.2-4 In line with these studies, the ephrinB/EphB system has been shown to act as a bidirectional communication interface.1,5 Direct cell-to-cell contact enables binding of ephrinB2 to corresponding EphB receptors inducing an EphB-mediated forward but also an ephrinB2-stimulated reverse signaling event. This kind of signaling establishes the mechanistic basis of border formation between arterial and venous endothelial cells through restriction of cellular intermingling.6,7
Despite its role as arterial marker molecule, ephrinB2 abundance has been shown to be dependent on microenvironmental cues. Angiogenic activation, shear stress, smooth muscle cell (SMC) contact, and vascular endothelial cell growth factor (VEGF) have all been shown to modulate ephrinB2 expression in endothelial cells.8-13 Likewise, arterial endothelial cells partially lose their ephrinB2 phenotype, whereas subpopulations of venous endothelial cells up-regulate ephrinB2 expression on prolonged periods in culture.13 Interestingly, ephrinB2 is located at the luminal and junctional endothelial cell surface and associates context-dependently with CD31.13 The functional consequences of an increased ephrinB2 protein expression in endothelial cells may therefore not be limited to an enhanced EphB-dependent propulsive stimulation6,7 but may also enable costimulation of circulating leukocytes.14,15
Although there is emerging evidence that endothelial cell ephrinB2 has many more functions than originally assumed, only little is known about its role during remodeling processes of the adult arterial vasculature. In this regard, we hypothesized that adaptive arterial remodeling of the adult vascular system is accompanied by up-regulation of ephrinB2 playing a decisive role in this process. As a well-known example of such an adaptive remodeling process, we studied the expression of ephrinB2 during arteriogenesis. This process is defined as the transformation of preexisting arterioles to arteries and thought to be influenced by biomechanical forces,16 which already have been shown to affect ephrinB2 expression during vascular development.10 Herein, we report that ephrinB2 is up-regulated during arteriogenesis, which may be triggered by cyclic stretch. In addition, our results indicate that the increase in ephrinB2 abundance in endothelial cells not only affects SMC migration but also supports monocyte recruitment and activation, processes known to be a prerequisite for arteriogenesis to occur.
Methods
An expanded Methods section is available on the Blood website (see the Supplemental Materials link at the top of the online article). The isolation of both human umbilical vein endothelial cells (HUVECs) and human thymus smooth muscle cells (HTSMCs) was approved by the local ethics committee (Heidelberg, Germany) and conformed to the principles outlined in the Declaration of Helsinki (1997).
Animal models
All animal studies were performed with permission of the Regional Council Karlsruhe and conformed to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (National Institutes of Health Publication No. 85-23, revised 1996). Five- to 6-month-old male C57/B6 mice were anesthetized with isoflurane, and the femoral artery was ligated just distal to the origin of the deep femoral artery. On day 7 after surgery, the mice were killed, perfused with colored pigment, and the hindlimbs were processed for morphologic and histologic examination.
Morphologic analysis
Immunohistochemical and immunfluorescence staining for ephrinB2 was performed on 4-μm paraffin sections using the polyclonal goat antimouse ephrinB2 antibody (R&D Systems, Wiesbaden, Germany) or, as control antibody, a goat antirabbit antibody (Dako Denmark A/S, Glostrup, Denmark) in combination with an enhanced detection method (Envision, Dako) and 3,3-diaminobenzidine or tyramide-Cy3 (PerkinElmer, Rodgau, Germany) according to the manufacturer's instructions.
Analysis of SMC migration and coculture spheroids
Porcine aortic endothelial cells (PAECs) overexpressing ephrinB2, EphB4, and truncated ephrinB2 were generated as described previously.6 SMC spheroids were generated and analyzed as described previously.17,18 Migration of HTSMCs interacting with PAECs was assessed by determining the circumference of at least 3 SMC spheroids per experimental group subtracting the initial spheroid circumference.
Separation of HTSMCs and PAECs was studied in coculture spheroids, which were fixed in zinc fixative, embedded in paraffin, cross-sectioned, and subsequently stained for the endothelial cell marker CD31. Separation of both cell types was analyzed by determining the number of CD31-positive endothelial cells, which were not attached to the PAEC monolayer on the surface and located in the center of the spheroid. At least 5 randomly selected spheroids in 3 sections per experimental group were analyzed.
Transmigration assay
PAECs or HUVECs were seeded onto porous cell culture inserts (BD Biosciences, Heidelberg, Germany). Transmigration of 106 THP-1 cells or human monocytes seeded into the upper chamber was enhanced by supplementing the medium in the lower chamber with 100 ng/mL MCP-1 (R&D Systems).
RT-PCR and decoy oligodeoxynucleotide technique
Reverse transcription (RT) and polymerase chain reaction (PCR) for human ephrinB2 and ribosomal protein L32 (RPL32) cDNA as well as preparation of the AP-1 decoy oligodeoxynucleotides was performed as described previously.19-21
Statistical analysis
All results are expressed as mean plus or minus SD. Differences between experimental groups were analyzed by Student t test. P values less than .05 were considered statistically significant.
Results
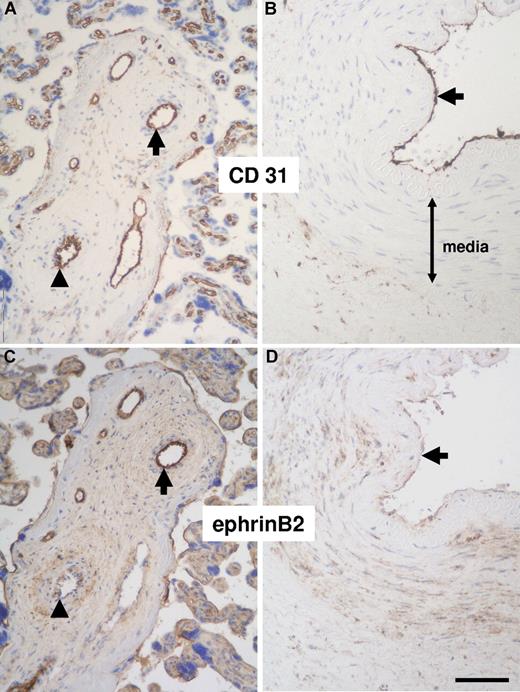
EphrinB2 protein abundance in arterial endothelial cells depends on local hemodynamics
Although ephrinB2 mRNA expression is well described throughout the literature, only little is known about ephrinB2 protein abundance in the human vasculature. To compare the ephrinB2 expression status in human embryonic (developing, ie, remodeling) and adult (quiescent) vasculature, we analyzed its abundance by immunohistochemistry in placenta tissue and coronary arteries. Surprisingly, ephrinB2 was not evenly expressed throughout the placental arterial vascular entity. Analyzing the lumen to media ratio of those blood vessels, which could clearly be identified as arteries by their morphology, we found that endothelial cells in arteries with enlarged diameter show a much more intense ephrinB2 staining (Figure 1A,C arrow) than those in arteries with a low lumen to media ratio (Figure 1A,C arrowhead; lumen to media ratio of arteries with strong or weak ephrinB2 staining: 1.96 ± 0.98 vs 0.53 ± 0.26; n = 13, P < .001). Furthermore, ephrinB2 expression was rather weak in adult arterial endothelial cells (Figure 1B,D arrows).
Immunohistochemical detection of ephrinB2 in serial sections of human arteries. Most endothelial cells from placenta arteries strongly express ephrinB2 (A,C, ⬆), whereas those in arteries with a reduced lumen-to-media ratio only weakly stain for ephrinB2 (A,C, ▴). Endothelial cells in adult coronary arteries show a markedly diminished expression of ephrinB2 (B,D, ⬆; endothelial cell staining intensity in panels C,D). Smooth muscle cells located in the media of adult coronary arteries are partially positive for ephrinB2 (D; scale bar represents 100 μm).
Immunohistochemical detection of ephrinB2 in serial sections of human arteries. Most endothelial cells from placenta arteries strongly express ephrinB2 (A,C, ⬆), whereas those in arteries with a reduced lumen-to-media ratio only weakly stain for ephrinB2 (A,C, ▴). Endothelial cells in adult coronary arteries show a markedly diminished expression of ephrinB2 (B,D, ⬆; endothelial cell staining intensity in panels C,D). Smooth muscle cells located in the media of adult coronary arteries are partially positive for ephrinB2 (D; scale bar represents 100 μm).
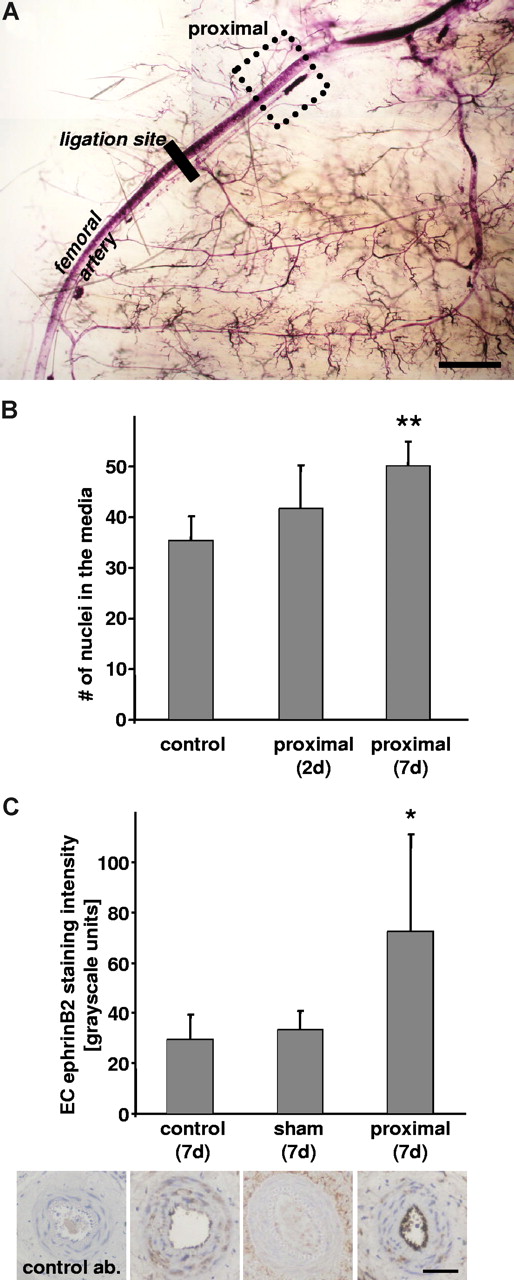
As these observations suggested that the degree of ephrinB2 abundance may be the result of different perfusion conditions, we tested whether a change in perfusion does affect ephrinB2 expression in arterial endothelial cells through occlusion of the murine femoral artery (Figure 2A). This intervention leads to an overall reduction in blood flow accompanied by a decrease in shear stress, whereas pressure and thus circumferential wall strain are increased proximal to the site of occlusion as a result of the accumulating volume. Both changes in the biomechanical load of the vessel wall may contribute to its adaptive remodeling as suggested by the observed increase in the number of SMC nuclei in the media proximal to the site of occlusion (Figure 2B). Similar to the findings in human adult arteries, ephrinB2 abundance in adult mouse femoral arteries was rather low. Disruption of regular perfusion, however, resulted in a marked increase in ephrinB2 abundance in the proximal femoral artery endothelial cells (Figure 2C). Additional immunohistochemical analyses revealed that the expression of EphB4, a high affinity receptor for ephrinB2, is not up-regulated in arteries under these conditions (data not shown).
EphrinB2 expression after ligation of the femoral artery. Femoral arteries from adult NMRI mice were analyzed proximal to the site of occlusion (A; scale bar represents 1 mm). Stenosis results in remodeling of the arterial vessel wall as evidenced by the increase in the number of nuclei in the media (B; n = 5, **P < .01 vs control). Staining of corresponding paraffin-embedded cross-sections revealed that endothelial cell ephrinB2 expression is very low under control and sham conditions but significantly up-regulated in the proximal part of the ligated artery (C; *P < .05 vs control, n = 5; scale bar represents 50 μm). The use of a control antibody did not yield any appreciable immunoreactivity (C, left image).
EphrinB2 expression after ligation of the femoral artery. Femoral arteries from adult NMRI mice were analyzed proximal to the site of occlusion (A; scale bar represents 1 mm). Stenosis results in remodeling of the arterial vessel wall as evidenced by the increase in the number of nuclei in the media (B; n = 5, **P < .01 vs control). Staining of corresponding paraffin-embedded cross-sections revealed that endothelial cell ephrinB2 expression is very low under control and sham conditions but significantly up-regulated in the proximal part of the ligated artery (C; *P < .05 vs control, n = 5; scale bar represents 50 μm). The use of a control antibody did not yield any appreciable immunoreactivity (C, left image).
EphrinB2 expression is increased in arterioles undergoing arteriogenesis
Based on the aforementioned results, we hypothesized that disturbance of arterial homeostasis through biomechanical induction of remodeling affects ephrinB2 expression in endothelial cells. To verify this hypothesis, we used the mouse hindlimb ischemia model where arteriolar remodeling after ligation of the femoral artery can be monitored. This biomechanically induced process is referred to as arteriogenesis and characterized by a time-dependent progressive increase in the diameter of collateral arterioles running in parallel to the femoral artery (Figure 3A-C). Detailed immunofluorescence (Figure 3D-L) as well as RT-PCR analyses (Figure 3M) revealed that expression of ephrinB2 in arteriolar endothelial cells is significantly up-regulated during arteriogenesis.
Morphologic analysis of collateral arteries in transparent mouse hindlimbs. Arteries were visualized by pigment perfusion in sham-operated (A) and ligated (B) hindlimbs. Diameter of collateral arterioles (A,B, ) was significantly increased (C, *P < .05 vs sham, n = 5) 7 days after ligation of the femoral artery. Immunofluorescence staining of ephrinB2 (Cy3) in collateral arterioles (D,F) was quantified by morphometry (L). In contrast to control conditions (D,L; *P < .05 vs sham, n = 4), endothelial cell ephrinB2 staining intensity (arrow) was significantly increased if the collateral arterioles underwent arteriogenic remodeling (F, arrow). CD31 immunofluorescence (Cy2) was used as a control to validate integrity of the endothelial cell monolayer (E,G; scale bars represent 10 μm). A species-matched control antibody did not produce any detectable immunostaining in collaterals from sham-operated (H, control antibody: red fluorescence; I, CD31: green fluorescence) or from ligated hindlimbs (J, control antibody; K, CD31; scale bars represent 10 μm). Individual collateral arterioles were isolated and subjected to RT-PCR analysis, which confirmed the increased expression of ephrinB2 in collateral arterioles undergoing arteriogenic remodeling (M, RT-PCR analysis of CD31 was used as an endothelial cell–specific internal standard).
Morphologic analysis of collateral arteries in transparent mouse hindlimbs. Arteries were visualized by pigment perfusion in sham-operated (A) and ligated (B) hindlimbs. Diameter of collateral arterioles (A,B, ) was significantly increased (C, *P < .05 vs sham, n = 5) 7 days after ligation of the femoral artery. Immunofluorescence staining of ephrinB2 (Cy3) in collateral arterioles (D,F) was quantified by morphometry (L). In contrast to control conditions (D,L; *P < .05 vs sham, n = 4), endothelial cell ephrinB2 staining intensity (arrow) was significantly increased if the collateral arterioles underwent arteriogenic remodeling (F, arrow). CD31 immunofluorescence (Cy2) was used as a control to validate integrity of the endothelial cell monolayer (E,G; scale bars represent 10 μm). A species-matched control antibody did not produce any detectable immunostaining in collaterals from sham-operated (H, control antibody: red fluorescence; I, CD31: green fluorescence) or from ligated hindlimbs (J, control antibody; K, CD31; scale bars represent 10 μm). Individual collateral arterioles were isolated and subjected to RT-PCR analysis, which confirmed the increased expression of ephrinB2 in collateral arterioles undergoing arteriogenic remodeling (M, RT-PCR analysis of CD31 was used as an endothelial cell–specific internal standard).
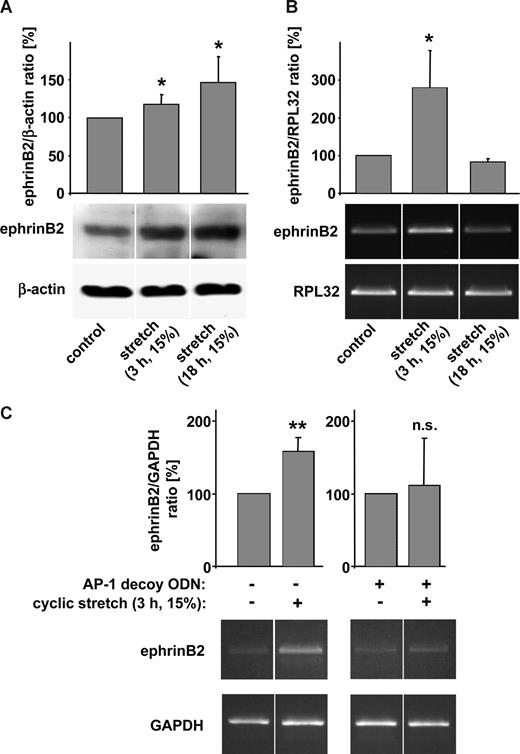
Cyclic stretch up-regulates ephrinB2 expression in endothelial cells of different origin
To decipher the mechanism by which ephrinB2 is up-regulated during arteriogenesis, we focused on those biomechanical forces that are thought to trigger this process: fluid shear stress and circumferential wall strain (stretching of vascular cells). As an increase in shear stress (from 3 to 12 dyne/cm2) failed to induce ephrinB2 expression in endothelial cells (data not shown) and actually may down-regulate it,11 we investigated whether cyclic stretch affects ephrinB2 expression in these cells. HUVECs up-regulated ephrinB2 expression in response to cyclic stretch both on the protein and on the mRNA level (Figure 4A,B). Prolonged exposure to cyclic stretch (up to 18 hours) resulted in a further increase in ephrinB2 protein, whereas ephrinB2 mRNA levels returned to baseline. In contrast to ephrinB2, expression of the ephrinB2 receptors EphB1, EphB2, and EphB3 was not affected by cyclic stretch in these cells (data not shown). Similar effects of cyclic stretch on the expression of ephrinB2 were found in human aortic as well as human saphenous vein endothelial cells (Figure S1).
Expression of ephrinB2 in stretch-stimulated endothelial cells. Human umbilical vein endothelial cells (HUVECs) were exposed to cyclic stretch (15%, 0.5 Hz) for 3 and 18 hours, respectively. EphrinB2 protein abundance (A) as well as mRNA expression (B) analyses revealed that cyclic stretch up-regulates ephrinB2 in these cells (A, *P < .05 vs control, n = 5; B, *P < .05 vs control; n = 3). β-Actin as well as the housekeeping gene RPL32 were used as internal standards. (C) Exposure of HUVECs to cyclic stretch (15%, 0.5 Hz, 3 hours) resulted in an increased expression of ephrinB2 mRNA that was completely abrogated after pretreatment with an AP-1 decoy oligodeoxynucleotide (ODN; 10 μM, 4-hour preincubation; **P < .01; n = 3; n.s., not significant). Messenger RNA expression of the housekeeping gene GAPDH was used as an internal standard.
Expression of ephrinB2 in stretch-stimulated endothelial cells. Human umbilical vein endothelial cells (HUVECs) were exposed to cyclic stretch (15%, 0.5 Hz) for 3 and 18 hours, respectively. EphrinB2 protein abundance (A) as well as mRNA expression (B) analyses revealed that cyclic stretch up-regulates ephrinB2 in these cells (A, *P < .05 vs control, n = 5; B, *P < .05 vs control; n = 3). β-Actin as well as the housekeeping gene RPL32 were used as internal standards. (C) Exposure of HUVECs to cyclic stretch (15%, 0.5 Hz, 3 hours) resulted in an increased expression of ephrinB2 mRNA that was completely abrogated after pretreatment with an AP-1 decoy oligodeoxynucleotide (ODN; 10 μM, 4-hour preincubation; **P < .01; n = 3; n.s., not significant). Messenger RNA expression of the housekeeping gene GAPDH was used as an internal standard.
We next analyzed the transcriptional mechanism underlying the stretch-induced increase in endothelial cell ephrinB2 expression by blocking the activity of AP-1. This well-known transcription factor is involved in a broad spectrum of cellular stress responses, including those associated with the exposure to cyclic stretch.21-23 Blocking its activity using a specific decoy oligodeoxyonucleotide abrogated the increase in ephrinB2 expression in stretch-stimulated endothelial cells (Figure 4B).
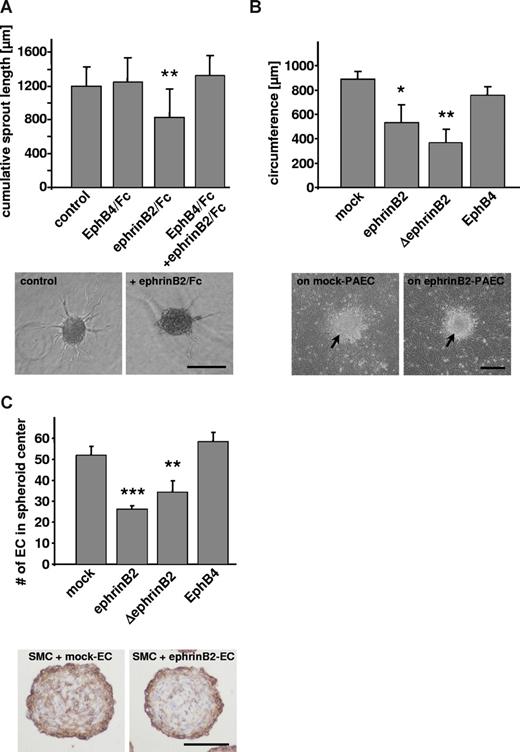
EphrinB2 expression in endothelial cells limits SMC migration and enhances their segregation from endothelial cells
Both reorganization of SMCs in the media of collateral arterioles as well as the recruitment of monocytes are hallmarks of arteriogenesis and need to be tightly orchestrated to ensure an adequate remodeling of the vessel wall. Because previous experiments showed that ephrinB2-induced forward EphB4 signaling is sufficient to induce the separation of EphB and ephrinB2 expressing cells by limiting their migration,6,7 we studied the effects of ephrinB2 on those cell types that may come into contact with endothelial cells during arteriolar remodeling, namely, SMCs and monocytes.
We noted that the presence of ephrinB2 in collagen matrices inhibits HTSMC migration (Figure 5A). Similar results were obtained using a lateral sheet migration model (migration distance after 48 hours: 870 ± 33 μm vs 735 ± 10 μm, n = 3; P < .05 control vs ephrinB2-treated cells). In contrast to migration, proliferation of HTSMCs was not affected by ephrinB2 (cell number after 48 hours: 100% ± 14.4% vs 116.4% ± 12.9%, n = 7; control vs ephrinB2-treated cells; with control cell number set to 100%).
Analysis of ephrinB2-induced effects on the migration and spreading of human thymus smooth muscle cells (HTSMCs) as well as the organization of porcine aortic endothelial cells (PAECs) and HTSMCs in 3-dimensional coculture spheroids. (A) The length of sprouts originating from the spheroids was reduced on treatment with dimeric ephrinB2 (**P < .01 vs control, representing one of 3 experiments with similar results; scale bar represents 200 μm). This effect could be blocked by simultaneous stimulation with dimeric ephrinB2 (2 μg/mL) and its receptor EphB4 (6 μg/mL). (B) Spreading of HTSMCs originating from spheroids (⬆), which were seeded on top of a confluent monolayer of PAECs, was inhibited if the smooth muscle cells were surrounded by PAECs overexpressing ephrinB2 or ΔephrinB2 (**P < .01, *P < .05 vs PAEC-mock, n = 3; scale bar represents 200 μm). (C) Mock, ephrinB2, ΔephrinB2, or EphB4-transfected PAECs were cocultured with HTSMCs in 3-dimensional spheroids. Overexpression of ephrinB2 or ΔephrinB2 in PAECs (PAEC-ephrinB2) enhanced the segregation of both cell types (***P < .001, **P < .01 vs PAEC-mock; n = 3; bottom panel shows CD31-stained cross sections of a paraffin-embedded PAEC-mock/HTSMC (left) and a PAEC-ephrinB2/HTSMC (right) coculture spheroid; scale bars represent 100 μm).
Analysis of ephrinB2-induced effects on the migration and spreading of human thymus smooth muscle cells (HTSMCs) as well as the organization of porcine aortic endothelial cells (PAECs) and HTSMCs in 3-dimensional coculture spheroids. (A) The length of sprouts originating from the spheroids was reduced on treatment with dimeric ephrinB2 (**P < .01 vs control, representing one of 3 experiments with similar results; scale bar represents 200 μm). This effect could be blocked by simultaneous stimulation with dimeric ephrinB2 (2 μg/mL) and its receptor EphB4 (6 μg/mL). (B) Spreading of HTSMCs originating from spheroids (⬆), which were seeded on top of a confluent monolayer of PAECs, was inhibited if the smooth muscle cells were surrounded by PAECs overexpressing ephrinB2 or ΔephrinB2 (**P < .01, *P < .05 vs PAEC-mock, n = 3; scale bar represents 200 μm). (C) Mock, ephrinB2, ΔephrinB2, or EphB4-transfected PAECs were cocultured with HTSMCs in 3-dimensional spheroids. Overexpression of ephrinB2 or ΔephrinB2 in PAECs (PAEC-ephrinB2) enhanced the segregation of both cell types (***P < .001, **P < .01 vs PAEC-mock; n = 3; bottom panel shows CD31-stained cross sections of a paraffin-embedded PAEC-mock/HTSMC (left) and a PAEC-ephrinB2/HTSMC (right) coculture spheroid; scale bars represent 100 μm).
Subsequently, we hypothesized that expression of ephrinB2 by endothelial cells may similarly limit SMC migration. To test this, HTSMC spheroids were seeded onto a confluent monolayer of PAECs. Mock or EphB4-transfected endothelial cells did not affect SMC spreading into the endothelial cell monolayer, whereas endothelial cells overexpressing ephrinB2 or a truncated variant of ephrinB2 (ΔephrinB2) significantly limited this process (Figure 5B; further details about the different PAEC lines used for this study are summarized in Figure S2).
Based on these results, we further hypothesized that limitation of SMC migration by ephrinB2 may support the organization of endothelial cells and SMCs during remodeling processes of the vessel wall. To test this idea, we studied the segregation of PAECs and HTSMCs (expressing EphB1, EphB2, and EphB3; data not shown) in 3-dimensional coculture spheroids. Segregation of both cell types, usually establishing a surface endothelial cell monolayer enclosing a core of SMCs, was significantly enhanced with endothelial cells overexpressing ephrinB2 (Figure 5C). This effect was observed even after truncation of the cytoplasmic domain of ephrinB2 (ΔephrinB2), which abrogates reverse signaling.
EphrinB2 affects MCP-1-induced monocyte transmigration through an endothelial cell monolayer
Further analyses on the functional role of ephrinB2 during arteriogenesis were mainly inspired by the finding that monocytes isolated from human buffy coat as well as THP-1 cells stably express a comparable pattern of EphB receptors (Figure S3), enabling the interaction with ephrinB2, which is preferentially localized at the apical surface of endothelial cells (Figure S4). Considering the expression of MCP-1 as a prerequisite for monocyte recruitment during arteriogenesis,24,25 we studied the effects of endothelial cell ephrinB2 expression on MCP-1–induced migration of THP-1 cells. This human monocyte/macrophage cell line was chosen because it resembles the EphB expression pattern and the behavior of human monocytes but shows a more homogeneous response to stimuli.
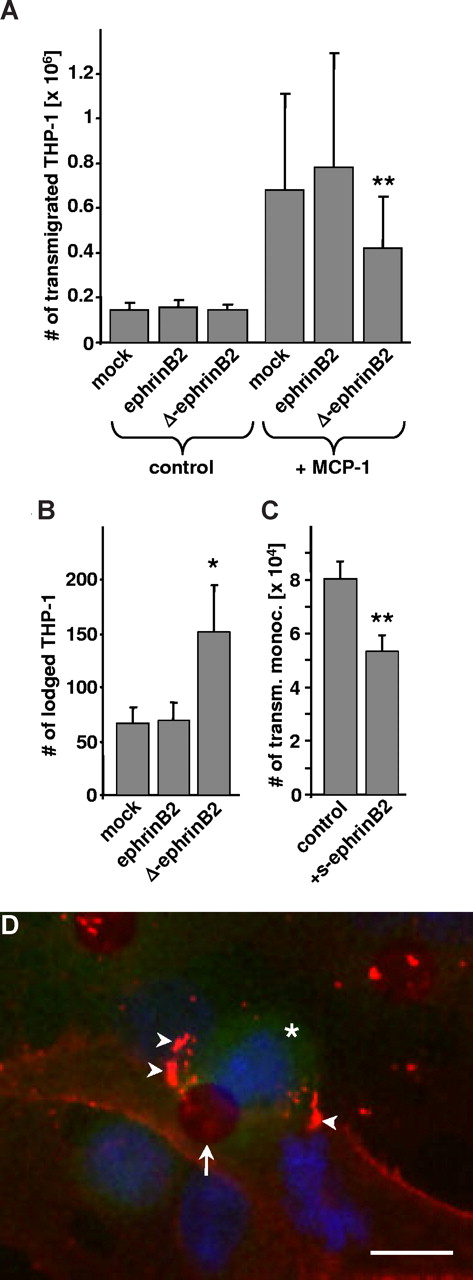
Basal transmigration of THP-1 cells through a monolayer of PAECs was not affected by the presence of ephrinB2 or ΔephrinB2 (Figure 6A). Subsequently, migration was stimulated with MCP-1 resulting in a 5-fold increase in the total number of transmigrated THP-1 cells, hence making this assay more sensitive to reveal a disturbed passage through the PAEC monolayer. Interestingly, overexpression of the truncated variant of ephrinB2 in the PAECs significantly inhibited THP-1 cell transmigration (Figure 6A). Additional analyses of the PAEC monolayer using a human-specific anti-CD31 antibody (detects only THP-1 cells) indicated that a significant proportion of the THP-1 cells was lodged in the ΔephrinB2-overexpressing PAEC monolayer (Figure 6B). Together with the reduced number of transmigrated THP-1 cells, this finding points toward a decelerated passage time. Similarly, blocking of ephrinB2 binding sites with soluble monomeric ephrinB2 inhibited the MCP-1–induced transmigration of human monocytes through a HUVEC monolayer (Figure 6C). In contrast, monomeric ephrinB2 did not affect the MCP-1–stimulated transmigration of human monocytes through a porous membrane, which was not covered by endothelial cells (data not shown).
Analysis of the transmigration of THP-1 cells through a monolayer of mock, ephrinB2, or ΔephrinB2-transfected PAECs. (A) Basal penetration through mock-transfected PAECs was 5-fold increased after MCP-1 stimulation and significantly inhibited by PAECs overexpressing ΔephrinB2 (**P < .01 vs MCP-1 stimulated mock-transfected PAECs; n = 8). (B) The number of MCP-1 stimulated THP-1 cells that were lodged in the PAEC monolayer was significantly increased if ΔephrinB2 was overexpressed by the PAECs (*P < .05 vs mock-transfected PAEC). (C) The MCP-1–induced transmigration of human monocytes through a HUVEC monolayer was inhibited by treatment with 4 μg/mL soluble monomeric ephrinB2 (**P < .01 vs control, n = 3). (D) An EphB4 receptor body–based immunofluorescence technique was applied to visualize the accumulation of ephrinB2 (D; arrowheads, red fluorescence) in ephrinB2-overexpressing PAECs after contact with THP-1 cells (D; * green fluorescence; scale bar represents 10 μm) transmigrating through a pore (D; arrow) in the porous membrane.
Analysis of the transmigration of THP-1 cells through a monolayer of mock, ephrinB2, or ΔephrinB2-transfected PAECs. (A) Basal penetration through mock-transfected PAECs was 5-fold increased after MCP-1 stimulation and significantly inhibited by PAECs overexpressing ΔephrinB2 (**P < .01 vs MCP-1 stimulated mock-transfected PAECs; n = 8). (B) The number of MCP-1 stimulated THP-1 cells that were lodged in the PAEC monolayer was significantly increased if ΔephrinB2 was overexpressed by the PAECs (*P < .05 vs mock-transfected PAEC). (C) The MCP-1–induced transmigration of human monocytes through a HUVEC monolayer was inhibited by treatment with 4 μg/mL soluble monomeric ephrinB2 (**P < .01 vs control, n = 3). (D) An EphB4 receptor body–based immunofluorescence technique was applied to visualize the accumulation of ephrinB2 (D; arrowheads, red fluorescence) in ephrinB2-overexpressing PAECs after contact with THP-1 cells (D; * green fluorescence; scale bar represents 10 μm) transmigrating through a pore (D; arrow) in the porous membrane.
To show that ephrinB2 is indeed involved in the transmigration process, we analyzed ephrinB2 distribution in endothelial cells on contact with THP-1 cells. By applying immunofluorescence techniques, we detected an accumulation of ephrinB2 in PAECs, which were in contact with the transmigrating THP-1 cells (Figure 6D arrowheads).
Discussion
Molecules with expression restricted to either arterial or venous endothelial cells are referred to as arteriovenous marker molecules and play a critical role in determining the corresponding endothelial cell lineages during embryonic development.26 Although detectable in murine endothelial cells of adult arteries,8 the expression level of the arterial endothelial cell marker ephrinB2 seems to be dependent on extracellular determinants as it is up-regulated by VEGF, contact to SMCs or hypoxia.13,27 Here we show that ephrinB2 protein abundance is rather low in endothelial cells of human or mouse arteries but strongly increased in arteries of the human placenta with enlarged diameter or segments of mouse arteries that had been exposed to a ligature-induced alteration of blood flow and pressure. Consequently, we hypothesized that these differences reflect the hemodynamic situation with low ephrinB2 abundance under normal perfusion conditions and an induction of ephrinB2 expression resulting from an increased perfusion pressure.
In line with this idea, it has been emphasized that biomechanical forces may act as critical determinants of the endothelial cell ephrinB2 phenotype.10 To analyze the mechanism of ephrinB2 up-regulation in more detail, we ligated arteries in hindlimbs altering the hemodynamic situation in preexisting collateral arterioles, which subsequently underwent adaptive remodeling referred to as arteriogenesis.28 Analyses of these collateral arterioles 7 days after ligation revealed that ephrinB2 expression in endothelial cells is up-regulated during this process. Both shear stress and circumferential wall strain have been proposed as important “molding forces” for arteriogenic remodeling.29,30 Because VEGF expression, which could easily explain the up-regulation of ephrinB2, is not affected at sites of collateral vessel growth31 and increased shear stress down-regulates rather than up-regulates endothelial cell ephrinB2 abundance,11 we focused on the effects of cyclic stretch, which corresponds to the rhythmic changes in circumferential wall strain in the arterial vessel wall. In contrast to shear stress, this biomechanical force affects endothelial cells and SMCs alike.
Exposure to cyclic stretch indeed up-regulated ephrinB2 expression in cultured endothelial cells irrespective of their embryonic, arterial, or venous origin. Further experiments, using an appropriate decoy oligonucleotide,21 indicated that neutralization of the well-known mechanosensitive transcription factor AP-122,23 inhibits this stretch-induced increase in ephrinB2 expression. This finding is further supported by an in silico analysis of the promoter of the human ephrinB2 gene, which revealed 2 putative AP-1 binding sites at positions −696 and −1268 upstream of the transcription start site (data not shown). In addition, gel shift analyses of stretched HUVECs revealed a nuclear translocation of AP-1 after 90 minutes, fitting well to the kinetics of the stretch-induced increase in ephrinB2 mRNA after approximately 3 hours (data not shown).
Thus, a prototypic stretch-dependent signal transduction pathway appears to govern endothelial cell ephrinB2 expression under these conditions. This mechanism may also explain the increase in ephrinB2 abundance in endothelial cells of the proximal femoral artery on occlusion, which is accompanied by a volume-dependent increase in pressure and hence circumferential wall strain. To our knowledge, this is the first report identifying cyclic stretch as a determinant of the endothelial cell ephrinB2 phenotype, which may also be of functional relevance for the arteriovenous differentiation of endothelial cells during embryonic development. Based on our data, a rise in blood pressure during the development of the vascular system may affect the arteriovenous differentiation of endothelial cells in a similar way as changes in blood flow. In line with our finding, it has also been reported that endothelial cells in pulmonary-to-aortic valve transposition grafts become ephrinB2-positive over time,32 further suggesting that (pressure-induced) deformation is capable of changing ephrinB2 abundance in adult endothelial cells. Likewise, venous endothelial cells can be induced to up-regulate ephrinB2 expression when exposed to cyclic stretch, as shown herein.
The functional relevance of changes in ephrinB2 abundance in adult blood vessels is largely unknown. It has been reported that endothelial cells expressing ephrinB2 segregate from EphB4-expressing endothelial cells and become susceptible to EphB4-dependent angiogenic activation.6,7 Similarly, angiogenesis has been repeatedly observed to be associated with an up-regulation of ephrinB2 expression8,9 and can be disturbed by treatment with soluble monomeric EphB4 receptors.33,34 Moreover, SMC ephrinB2 deficiency or its ectopic overexpression leads to functional failure of blood vessels resulting from defective association between endothelial and mural cells or insufficient SMC recruitment to the vessel wall, respectively.35,36 Thus, ephrinB2-dependent signaling plays a critical role in the formation and integrity of the vessel wall.
Here we demonstrate ephrinB2 up-regulation during arteriogenesis, an adaptive remodeling process that is dependent on the migration as well as proliferation of SMCs to finally enlarge the vessel diameter. Because the integrity of the vessel wall has to be preserved throughout the remodeling process, SMC migration must be tightly regulated and limited to defined borders. Based on a 3-dimensional spheroid model, we found that segregation of endothelial cells and SMCs is enhanced if the endothelial cells overexpress ephrinB2 irrespective of whether they express the full-length or truncated ephrinB2 variant. Earlier experiments have shown that repulsive forward EphB4 signaling is sufficient to induce endothelial cell segregation.6 This may also explain the observed inhibition of SMC migration on contact with ephrinB2 or ΔephrinB2 overexpressing endothelial cells as well as the enhanced segregation of both cell types on coculture in 3-dimensional spheroids. These findings therefore suggest that ephrinB2-mediated interactions between mural and endothelial cells reduce the migration of vascular SMCs, thus ensuring adequate and stable coverage of the maturing vasculature, as recently proposed.35 Following up on this idea, ephrinB2 expression in endothelial cells may actually stabilize the organization of the vessel wall by defining a border for migratory activity of SMCs during remodeling.
With respect to the fact that arteriogenic remodeling is usually associated with and critically dependent on MCP-1–dependent monocyte recruitment,24,25,37 we also studied to what extent endothelial cell ephrinB2 expression is mechanistically involved in the interaction of these cells with monocytes. This approach was also spurred by the finding that monocytes express EphB receptors, which may interact with endothelial ephrinB2 located at their apical surface. Both findings concur with earlier reports on the expression of Eph/ephrin family members in leukocytes and their putative functional relevance14,16,38 as well as with the luminal localization of ephrinB2 in HUVECs.13
Against the background of these results, we observed that mock or full-length ephrinB2-transfected endothelial cells do not affect monocyte transmigration, indicating that basal ephrinB2 abundance is sufficient for this process to occur. In contrast, MCP-1–stimulated transmigration of monocytes through a monolayer of PAECs is disturbed when these cells overexpress the truncated variant of ephrinB2, pointing toward reverse ephrinB2 signaling in endothelial cells as a critical factor for leukocyte diapedesis. Presumably, the mass of truncated ephrinB2 in the transfected PAECs prevents the binding of leukocyte EphB to other functional endogenous ephrinB2 binding sites on the PAECs, thus precluding a compensatory mechanism. Likewise, blocking of ephrinB2 binding sites with monomeric soluble ephrinB2 (which does not induce EphB forward signaling because it cannot cluster EphB receptors) inhibited the transmigration of human monocytes through a monolayer of HUVECs, which typically express high levels of ephrinB2.6,13 Furthermore, MCP-1–induced transmigration of human monocytes through an ephrinB2-coated porous membrane had no effect on their transmigratory activity, suggesting that ephrinB2 reverse signaling in endothelial cells rather than EphB forward signaling in monocytes affects their diapedesis.
Previous experiments on the binding of soluble EphB4 to ephrinB2-overexpressing endothelial cells suggest that ephrinB2 accumulates and becomes internalized on EphB4 receptor binding, whereas ΔephrinB2 is lodged in intercellular junctions.13 Accordingly, we detected an accumulation of ephrinB2 in endothelial cells on contact with monocytes indicative of an interplay between the endothelial cell ephrinB2 ligand and a monocyte EphB receptor. Interestingly, monocytes were trapped during penetration of the ΔephrinB2-overexpressing endothelial cell monolayer. This behavior copies the phenotype of CD31-deficient mice whose leukocytes are arrested between endothelial cells and the basal membrane during inflammation-induced recruitment.39 Based on earlier work showing that ephrinB2 associates context-dependently with CD31,13 these results point toward an ephrinB2/CD31-dependent monocyte transmigration mechanism, which is currently under investigation.
Taken together, the present findings show that (1) the level of ephrinB2 expression in arterial endothelial cells may change depending on the local hemodynamics, (2) ephrinB2 is up-regulated during arteriogenic remodeling of collateral arterioles presumably because of an increase in wall tension, and (3) this molecule affects SMC migration and leukocyte transmigration. These findings put ephrinB2 into a new functional context, playing a role in the adaptive remodeling of adult arteries.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Ms Lorena Urda and Gudrun Scheib for excellent technical assistance and Dr Frederik Marme and Dr Markus Hönicka for supplying human placenta and coronary tissue.
This work was supported by the Deutsche Forschungsgemeinschaft (SFB TR23 projects A3 and C5). H.G.A. is supported by an endowed chair from the Aventis Foundation.
Authorship
Contribution: T.K. designed and performed part of the research, analyzed the data, performed the statistical analysis, and drafted the manuscript; J.B. performed part of the research and collected data; D.P. and H.G.A. contributed vital new reagents and critically reviewed the manuscript; and M.H. designed part of the research, interpreted the data, and revised the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Markus Hecker, University of Heidelberg, Institute of Physiology and Pathophysiology, Division of Cardiovascular Physiology, Im Neuenheimer Feld 326, 69120 Heidelberg, Germany; e-mail: hecker@physiologie.uni-hd.de.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal