Abstract
Aim: To develop and evaluate a DNA-based method for monitoring of MRD in CML
Background: At present, monitoring of MRD in CML uses RNA and reverse transcription (RT-PCR). This leads to a number of disadvantages, including the potential for RNA degradation, requirement for reverse transcription, difficulty in standardisation and only an indirect relationship between assay result and cell number.
Methods: A highly multiplexed, short-range PCR using six BCR primers and a pool of 282 ABL primers was used to amplify across the BCR-ABL translocation breakpoint and was followed by 2–3 rounds of “bottleneck PCR”, a technique recently-developed in our laboratory, which adjusts primer concentration so as to minimise non-specific amplification and facilitate highly multiplexed PCRs. The breakpoint was isolated and sequenced, patient-specific primers were synthesised, and MRD was quantified using 10 μg of DNA and a 3 round nested quantitative PCR incorporating a Taqman probe in the third round. Samples from patients on treatment were divided and assayed both by this technique and by RT-PCR. 10 μg of DNA from a normal individual was used in each assay as a control for non-specificity.
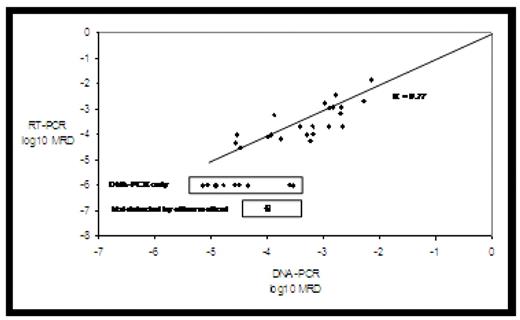
Results: The BCR-ABL breakpoint was successfully isolated and sequenced in 28 of the 29 patients studied and MRD was assayed in 38 samples from 24 patients. Follow-up samples from 4 patients were unavailable MRD was detected and measured by both methods in 22 samples, detected and measured only by DNA-PCR in 10 samples and not detected by either method in 6 samples. The limit of detection of RT-PCR was in accord with previous results which indicated it to be a mean decrease of 4.5-logs below baseline. The mean limit of detection of DNA-PCR was an MRD of 7.2 x 10−7. Assay precision was determined by performing independent replicate assays on different days and by different individuals on the 32 samples with MRD detectable by DNA-PCR. The median SD of a single assay was 0.15 log units with the range being 0.00 – 0.64 log units.
Conclusions
Monitoring of MRD by DNA-PCR is feasible in the great majority of patients with CML.
In terms of possible clinical benefits, DNA-PCR is more sensitive than RT-PCR, and provides a direct measure of leukemic cell number in the individual patient.
Use of DNA rather than RNA simplifies specimen collection and transport. In terms of laboratory benefits, DNA-PCR obviates reverse transcription and inter-laboratory standardisation.
The principal disadvantage of the method is the initial cost, although this may be able to be amortised over several assays if monitoring is ongoing.
Disclosures: Morley:Monoquant: Equity Ownership, Patents & Royalties. Bartley:Monoquant: Research Funding. Latham:Monoquant: Research Funding. Martin-Harris:Monoquant: Research Funding. Budgen:Monoquant: Research Funding. Wilczek:Monoquant: Research Funding. Branford:Novartis and Bristol Myers Squibb: Honoraria, Research Funding.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal