Abstract
The survival of children with sickle cell disease (SCD) has improved over the past several decades, especially for very young children. However, we know less about mortality during adolescence, and we do not accurately know the current proportion of children born with SCD who survive to adulthood. The first report from the Dallas Newborn Cohort (DNC), which included follow-up through June 2002, estimated overall survival at 18 years of age to be 85.6% (95% C.I.: 73.4 – 97.8) for individuals with sickle cell anemia (SS) or sickle-β0-thalassemia (Sβ0) (
Blood 2004;103:4023–7
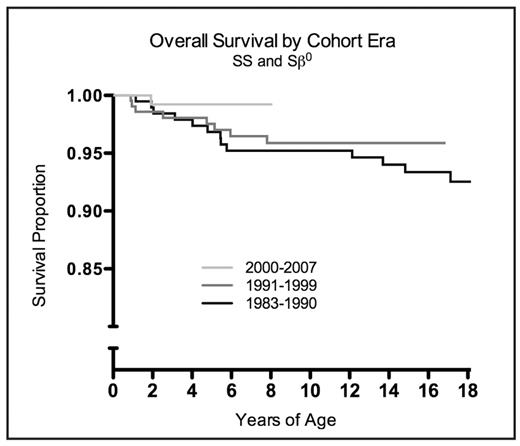
). The confidence interval of this estimate was wide because only 8 cohort subjects were 18 years old at the time. Here we update the survival analysis with 5 more years of accrual and follow-up to provide an accurate, contemporary estimate of mortality for patients with SCD through 18 years of age. The DNC includes all individuals with SS, Sβ0, sickle-hemoglobin C disease (SC), or sickle-β+-thalassemia (Sβ+) who were diagnosed by the newborn screening program of Texas (initiated November 1, 1983) and seen at least once in our center. Subjects were analyzed in two separate groups because of clinical similarity: SS/Sβ0 and SC/Sβ+. Overall survival was analyzed by the Kaplan-Meier method. Subjects were censored at the time of their last clinical encounter. Between July 2002 and July 2007 we identified 229 new members of the DNC and added 3,201 additional patient-years of follow-up. The cohort now includes 940 subjects (572 SS, 284 SC, 63 Sβ+, 21 Sβ0; 52.8% male), and it provides a total of 8,857 patient-years of follow-up (5,819 SS/Sβ0 patient-years, 3,039 SC/Sβ+ patient-years). Mean follow-up is 9.4 years (range 0.1– 20.6 years), and 97 subjects are now at least 18 years of age at last follow-up. To date, 92 subjects (9.8%) have been lost to follow-up (not seen for >5 years), and 33 subjects have died (30 SS/Sβ0, 3 SC/Sβ+). There were 7 new deaths in DNC patients since 2002, all of which occurred in patients who were 18 years of age or older. Of all deaths, 23 were SCD-related (5 acute chest syndrome, 5 sepsis, 4 multi-organ failure syndrome, 9 other), and 10 were apparently unrelated to SCD (4 trauma or accidental death, 6 unrelated medical conditions). All SC/Sβ+ deaths were apparently unrelated to SCD. Overall survival at 18 years was 93.9% (95% C.I. 90.3 – 96.2; 81 patients > 18 years of age) for SS/Sβ0 subjects and 98.4% (95% C.I. 94.4 – 99.5; 16 patients > 18 years) for SC/Sβ+ subjects. The overall incidence of death in the SS/Sβ0 and SC/Sβ+ subgroups was 0.52 and 0.10 per 100 patient-years, decreased from 0.59 and 0.24 in the original DNC analysis. Survival also appears to be improving across cohort eras (Figure). In conclusion, approximately 6% of children with SS or Sβ0 die during childhood, but almost all children with SC or Sβ+ live to become adults. Although early childhood mortality has greatly decreased, we show that many adolescents and young adults still die from SCD. Notably, acute chest syndrome and multi-organ failure have now surpassed sepsis as the leading causes of death. These data provide the accurate, contemporary foundation for the counseling of parents of newborns with SCD and for genetic counseling for prospective parents. Finally, given the marked decrease in early mortality we show here, new efforts to improve survival in SCD should focus on adolescents and young adults.Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author
2008, The American Society of Hematology
2008

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal