Abstract
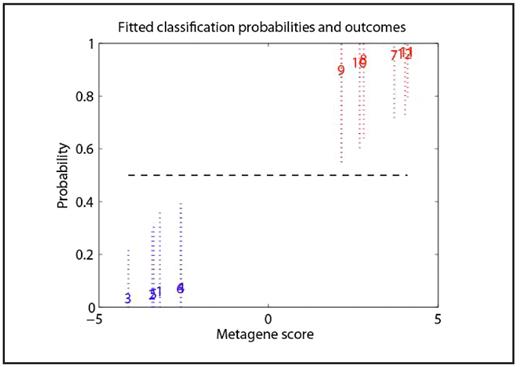
Pulmonary artery hypertension (PAH) occurs in 30–50% of adult patients with sickle cell disease (SCD), with mortality ranging from 16 to 50% and a median survival of 25 months. Our objective was to use gene expression profiling to develop a gene signature predictor for PAH through the analysis of gene expression of blood cells from SCD patients with or without PAH. We hypothesized that these gene signatures could allow us to identify patients at risk for PAH, as well as to generate hypotheses as to the pathophysiology of PAH in SCD. We used Affymetrix U133A2 GeneChip to determine the RNA expression of both whole blood and leukocytes using PAXgene and Leukolock methods, respectively. The study population included patients homozygous for HbS or with HbSβ0 thalassemia. Subjects with PAH were ≥18 years old, in steady state, and had PAH either by 2D echo (TR jet ≥ 2.7 m/sec) or right-sided catheterization (mean PA pressure ≥ 30 mmHg). Patients were excluded if they were pregnant, had co-existing rheumatologic conditions or other inflammatory diseases, were on chronic transfusion therapy or had had a vaso-occlusive episode in the previous 4 weeks. The control subjects were patients with SCD but without PAH (TR jet ≤ 1.8 m/sec or mean PA pressure <25 mmHg). Hierarchical clustering based on the gene expression pattern from 7 patients with PAH and 6 controls showed a trend for the clustering of SCD patients with PAH away from SCD patients without PAH. This trend was present for the gene expression in both whole blood and leukocytes. A Bayesian regression analysis was then performed to identify a set of predictor gene signatures for the PAH phenotype (Figure 1) in SCD. Finally, using gene set enrichment analysis, we found that the leukocytes from patients with PAH were highly enriched in the gene sets deriving from hematopoietic stem cells, corroborating the hypothesis of hyperhemolysis and higher blood cell turnover in this population. Other pathways showing upregulation in PAH were PTEN, TGFβ, cyclin D1, WNT and PPAR. Although these data are preliminary, they suggest that PAH in SCD does indeed have a distinct gene signature profile that may become useful in identifying risk for PAH prospectively, as well as in directing further investigation into the pathogenesis of PAH in SCD.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal