Abstract
Introduction: Tumor angiogenesis is gaining importance in hematological malignancies; it is balanced by many known and unknown positive and negative angiogenic factors. However, studies related to the prognostic significance of angiogenic factors and lymphoproliferative diseases are limited compared to solid tumors. This is a single institution study evaluating the prognostic impact of serum Endostatin, VEGF, and bFGF in non-Hodgkin’s lymphoma (NHL).
Patients and methods: Pretreatment serum level of Endostatin (S-Endostatin), VEGF (S-VEGF), and bFGF (S-bFGF) were measured by Enzyme-Linked Immunoabsorbant Assay (ELISA) on 136 NHL patients: 82 patients (60%) had aggressive NHL (diffuse large B cell lymphoma [DLBCL] or other aggressive non-DLBCL) and 54 patients (40%) had indolent lymphomas (follicular lymphoma [FL] or other indolent non-FL). For each angiogenic factor, univariate progression-free survival (PFS) and overall survival (OS) analyses were performed according to the quartiles of the distribution of serum level values. Each of the analyses was aimed to detect a trend between prognosis and the serum level of the angiogenic factor. Eight prognostic groups were defined according to the type of NHL and the prognostic indexes (International Prognostic Index [IPI] for DLBCL and aggressive non-DLBCL, and Follicular International Prognostic Index [FLIPI] for FL). Survival analyses stratified on the prognostic group were used to test the independent prognostic value of each angiogenic factor. Survival curves were compared with logrank tests. Distributions of serum level values were compared with Kruskal-Wallis tests. The median follow-up was 78 months.
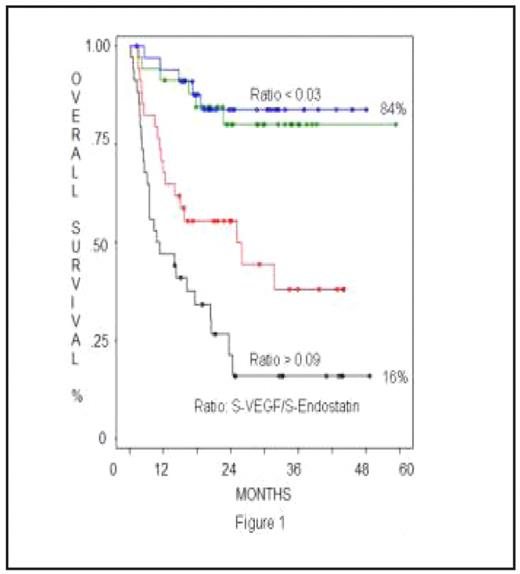
Results: Pretreatment angiogenic serum levels were not significantly different between all categories of NHL, except for VEGF level, which was slightly higher in the aggressive group compared to the indolent group (666 pg/ml vs. 465 pg/ml; p=0.03). Low S-Endostatin and high S-VEGF at diagnosis were associated with poor PFS (p=0.002 and p=10−4 respectively) and poor OS (p=0.04 and p=10−6 respectively). Patients with S-Endostatin within the lowest quartile had only 29% PFS and 49% OS in contrast to a 67% PFS and 82% OS among patients with Endostatin within the highest quartile. Similarly, patients with S-VEGF within the highest quartile had only 20% PFS and 26% OS in contrast to a 70% PFS and 85% OS among patients with VEGF within the lowest quartile. The VEGF/Endostatin ratio was used to combine the results from S-VEGF and S-Endostatin. The 4 groups corresponding to the quartiles of the distribution of VEGF/Endostatin ratio had different OS and PFS (p<10−6 for both); PFS and OS were respectively 15% and 16% for patients from the highest quartile VEGF/Endostatin ratio and 79% and 84% for those from the lowest quartile Figure 1. The independent prognostic impact of S-Endostatin, S-VEGF and VEGF/Endostatin ratio remained significant on PFS (p=0.0003, p=0.001 and p<10−6 respectively) and OS (p=0.01, p=10−4 and p<10−6 respectively) after stratification on the prognostic group. We did not find any relation between pretreatment S-bFGF and prognosis in our patients.
Conclusion: Our results showed that pretreatment serum levels of VEGF and Endostatin are significantly related to outcome in NHL patients; the higher the VEGF/Endostatin ratio is, the poorer the prognosis. A better understanding of angiogenesis in lymphoproliferative diseases is mandatory in order to develop new anti-angiogenic targeted therapeutic agents that can change the outcome of these patients.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal