Abstract
The utility of International Prognostic index (IPI) in the era of immunochemotherapy could not be determined by the available randomized trials. Recently, the study of British Columbia group suggested that a revised IPI (R-IPI) which redistributed the IPI factors into 3 distinct prognostic groups provided a more clinically useful prediction of outcome for patients with diffuse large B-cell lymphoma (DLBCL). We investigated the clinical outcomes of R-CHOP chemotherapy in patients with DLBCL for determining which has a more differential potential of predicting the prognosis among R-IPI or standard IPI.
Patients and Methods: We analyzed a total of 348 patients with newly diagnosed DLBCL from National University Hospitals of Southern Korea (NUHSK) between September 2002 and July 2008. R-CHOP conducted standard doses of chemotherapy and rituximab (375 mg/m2) administered a 21-day interval. The limited-stage patients were treated with 3rd or 4th chemotherapy followed by involved field radiation therapy (IFRT) and the advanced-stage patients were treated with six to eight cycles of chemotherapy.
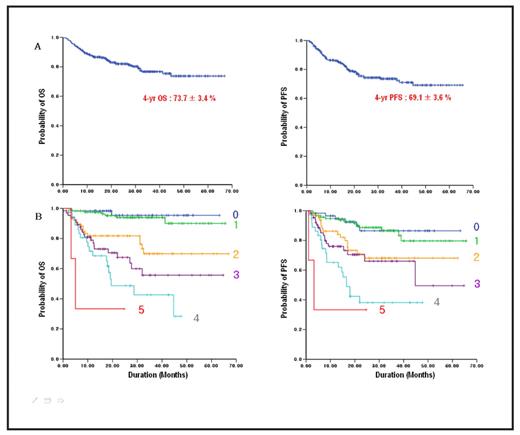
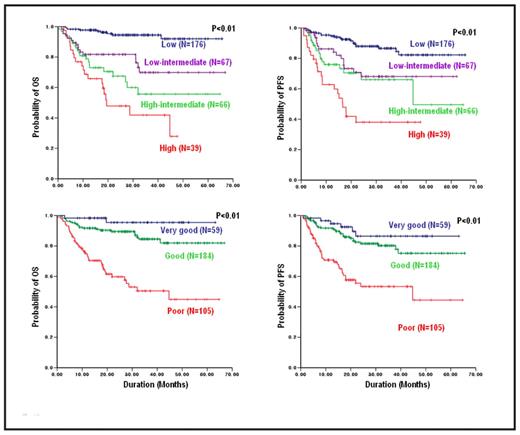
Results: The median age was 61 years (range, 18–85) with 51.6% of patients aged above 60. After a median follow-up of 25 months (range, 2-66.8), 280 patients (80.5%) were alive and 76 patients (21.8%) had relapsed or progressed. 16 patients (4.6%) underwent autologous stem cell transplantation (ASCT). The 4-year probability of overall survival (OS) and progression-free survival (PFS) were 73.7 ± 3.4 % and 69.1 ± 3.6 %, respectively (Fig. 1A). The distribution of patients and 4-year OS rates according to IPI factors were followings; 16.7% patients had zero risk factor with 95.4%, 33.9% patients had 1 factor with 90.0%, 19.3% patients had 2 factors with 69.9%, 19.0% patients had 3 factors with 55.7%, 10.3% patients had 4 factors with 28.4% and 0.9% patients had 5 factors without reached 4-year OS rates (Fig. 1B). Both standard IPI and revised IPI showed a significant potential as prognostic variable in OS and PFS. However, the standard IPI distinguished clinical outcomes between patients with 3 risk factors and patients with 4–5 risk factors. In addition, there was no survival difference between patients with zero risk factor and patients with 1 risk factor (Fig. 2).
Conclusion: The standard IPI had more differentiation potency in predicting prognosis than R-IPI in patients with DLBCL treated with R-CHOP chemotherapy.
Overall outcomes (A) and outcomes according to the number of IPI factors (B)
Comparison of OS and PFS according to the standard IPI and revised IPI
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal