Abstract
BACKGROUND: The diagnosis of monoclonal B-cell lymphocytosis (MBL) is used to characterize patients who have a circulating population of clonal B-cells, a total B-cell count of <5 x 109/L, and no other features of another B-cell lymphoproliferative disorder. In most patients the immunophenotype is similar to that of chronic lymphocytic leukemia with co-expression of CD19 and CD5. The natural history of CLL-phenotype MBL is unclear. We used the Mayo Clinic hematopathology database to identify patients with CLL-phenotype MBL and abstracted clinical information on natural history and prognostic parameters from clinical and research records.
METHODS: Using hematopathology records, we identified a cohort of 1820 patients seen at Mayo Clinic between August 1998 and May 2006 who underwent investigation using peripheral blood flow cytometry and who were found to have a clonal B-cell population of CLL phenotype. After elimination of patients with advanced stage (Rai I-IV), previously treated CLL, and individuals with an established diagnosis of CLL/MBL >1 year prior to flow, 636 unique patients with isolated lymphocytosis were identified. Based on our prior analysis (Leukemia Research 32:1458) demonstrating that nearly all patients with an ALC >10x109/L have a B-cell count >5x109/L, we focused the remaining analysis on the 405/636 patients who had an ALC <10x109/L and the necessary raw data from flow cytometry analysis to determine the B-cell count.
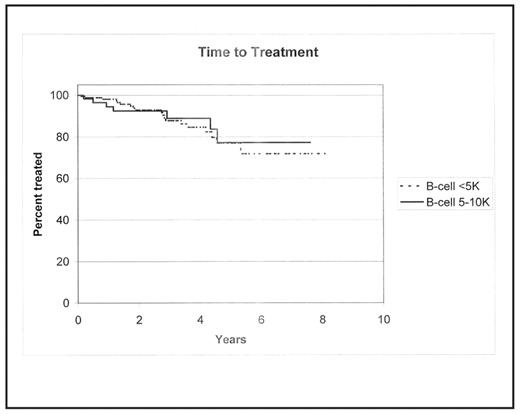
RESULTS: Among the 405 individuals with an ALC <10x109/L, 306 (76%) had a B-cell count <5x109/L at the time of flow and met the current criteria for the diagnosis of MBL (BJH 130:325). Median age at the time of MBL diagnosis was 70 years (range 34 – 93). A slight male preponderance was observed (59% male). B-cell counts ranged from 0.02 to 4.99x109/L and ALC ranged from 0.3–9.6 x109/L. CD38 status was available for 268 (88%) MBL patients of whom 20% were CD38 positive using the 30% threshold. Cytogenetic analysis by fluorescent in situ hybridization (FISH) was available in 130 (42%) MBL patients. Using the hierarchical classification system of Dohner and colleagues, 57 (44%) were 13q-, 23 (18%) were trisomy 12, 5 (4%) were 11q-, 4 (3%) were 17p-, and 39 (30%) had no defect detected. ZAP-70 status was available for 77 (25%) patients of whom 13% were ZAP-70+ positive. Patients underwent sequential monitoring with a median follow-up of 1.7 yrs (range 0–8.1 yrs). Time from diagnosis to treatment for patients meeting criteria for MBL (n=306) as compared to Rai stage 0 CLL patients with B-cell counts between 5.0 and 10.0 x109/L (n=99) was not significantly different and is shown in Figure 1 (p=0.87). For individuals with MBL, survival free of treatment was 98% (95%CI: 96–100%) at 1 year, 93% (95%CI: 89–98%) at 2 years, and 77% (95%CI: 67–89%) at 5 years. While gender (p=0.10), and B-cell count as a continuous variable (p=0.15) were not found to be associated with time to treatment (TTT) among MBL patients, age (p=0.02, HR=0.94, 95% CI: 0.89–0.99) and CD38 status (p<0.02, HR: 3.3, 95% CI: 1.2–9.2) did show a relationship with TTT.
CONCLUSIONS: Although we observed a low rate of progression among individuals meeting criteria for MBL, TFS was similar to individuals meeting current criteria for Rai stage 0 CLL who had B-cell counts between 5.0 – 10.0 x109/L . Among individuals meeting criteria for MBL, younger patients and those who were CD38 positive had a shorter time to treatment. Additional studies are needed to determine what B-cell count or other characteristics should be used to distinguish between MBL and Rai stage 0 CLL.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal