Abstract
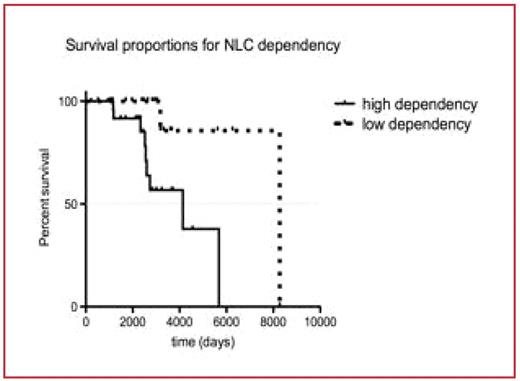
Chronic lymphocytic leukemia (CLL) cells often undergo spontaneous apoptosis in vitro unless co-cultured with accessory cells, such as nurselike cells (NLC), which likely also function in the leukemia-cell microenvironment to promote CLL-cell survival in vivo. However, we observed the CLL cells of different patients varied in their relative dependency on NLC for survival, even when examined on NLC derived from the same donor. We hypothesized that the relative dependency on NLC was an intrinsic characteristic for each CLL cell population and that measurement of the relative degree of NLC-dependency might serve to segregate patients into subgroups with different biologic or clinical behavior. To test this hypothesis, we assessed the cyropreserved primary leukemia cells of 45 untreated CLL patients for their relative dependency on NLC for survival in vitro. NLC were generated as described through co-culture of CLL B cells with isolated CD14+ blood mononuclear cells of healthy donors. The viability of CLL cells cultured with or without NLC was determined after two days co-culture and compared with that of the initial CLL cell viability, which typically was greater than 85%. To assess the survival support provided by NLC to the leukemia cells we determined the relative viability of leukemia cells alone was divided by the viability of CLL cells co-cultured with NLC. CLL NLC dependency index NLC was defined as 1-relative viability. We multiplied this result by 100 and then subtracted the product from 1 to derive the NLCdependency index. The NLC-dependency index for the CLL cells from different patients (n =16) ranged from 0.5–63.7 with a median of 26.9. In contrast, we observed relatively little variation in the NLC-dependency index for any one sample when measured in different experiments (2–4 assays/sample). Furthermore, the NLC-dependency index for CLL cells collected at different times from any one patient also was relatively constant, resulting in an intrapatient variation of in NLC-dependency index of only 5.6%. Using recursive partitioning, we examined the relationship between the NLC-dependency index and time from diagnosis to first treatment for 45 patients. This allowed us to determine the optimal threshold for segregating patients into groups with high versus low NLCdependency. A NLC-dependency of 26 was found the optimal cut point to segregate the 45 patients into 2 groups that exhibited different median times from diagnosis to initial therapy. Using this threshold, the NLC dependency index could reliably segregate the patients into the two categories of high versus low NLC-dependency, even when assessed on CLL cells collected at different time points. There was a significant association between a high NLC dependency index and expression of CD38 (spearman’s rho = 0.4, p=0.008). CD38 is noted to be a receptor for CD31, which is found expressed on NLC. Moreover, when we segregated patients into groups of low versus high NLC-dependency based upon the index cut-off of 26, we found a significant association between high NLC-dependency and expression of CD38 [Fisher’s exact test, p=0.017]. Furthermore, we observed that patients with CLL cells that had a high NLC-dependency index experienced a significantly shorter median survival (4137 days) than did those patients with CLL cells that had a low NLC-dependency index (8276 days), using the log rank test (p=0.0037). (See Figure) The overall survival hazard ratio for NLC dependency was 11.5 (Cox proportional hazards regression, p=0.021). This intriguing inverse relationship between the relative dependency of CLL cells on NLC for in vitro survival and overall patient survival suggests that the microenvironment might play a significant role in the pathophysiology and/or progression of CLL and that agents targeting the leukemia-cell microenvironment might be effective in patients with relatively aggressive disease.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal