Abstract
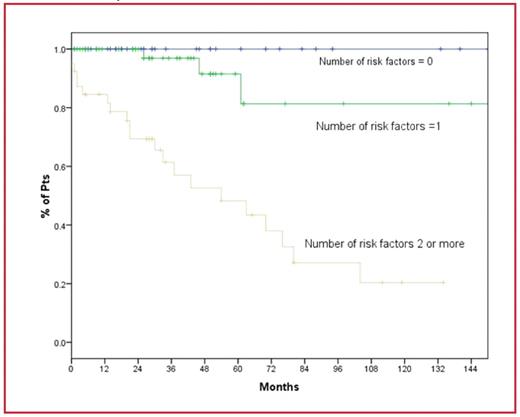
There is limited access to advanced molecular and immunophenotypic techniques such as immunoglobulin heavy chain variable mutational status and ZAP-70 expression analysis in many parts of the world. To facilitate the development of a clinical model based on readily available clinical and well-standardized pathological data, we analyzed the well known prognostic factors in chronic lymphocytic leukemia (CLL) and proposed a scoring system. We searched the CLL database and among 465 patients (pts) we included 128 pts where the staging, blood counts, immunophenotypic and follow up data are complete. The baseline characteristics of this group and the significance of the proposed factors on the progression-free survival on univariate analysis are summarized in the table. Progression–free survival (PFS) was defined as the time from diagnosis to the time where treatment for CLL is indicated and if no treatment id indicated, the time of last follow up. In this 5 point scoring system we added one point for the presence of each one of the following factors: male gender, Rai stage 1 or more, lymphocyte count of 20 ×109/l or higher, lymphocyte doubling time less than 12 m, CD 38 expression of 20% or more. We further lumped these groups into 3 groups: no risk factors, one risk factor and tow or more risk factors. Thirty eight patients (30%) were found to have no risk factors and their 5 and 10 year PFS was 100% and 100% respectively. Forty nine pts (38%) have at least one risk factor and their 5 and 10 y PFS was 92% and 81% respectively. Forty pts (31%) have two or more risk factors and their 5 and 10 y PFS was 48% and 20% respectively. Those differences in PFS were significant (p<0.00001). We conclude that readily available clinical and laboratory information in patients with CLL can be utilized to predict the risk of disease progression. Pts with no risk factors can be reliably reassured and do not require regular monitoring. Correlation of these findings with other molecular prognostic factors is needed.
Table: Risk factors for disease progression
| Parameter . | N (%) . | 5-y PFS . | 10-y PFS . | p value (UVA)* . |
|---|---|---|---|---|
| *Univariate analysis | ||||
| Sex: Male | 71 (56) | 67% | 43% | 0.01 |
| Female | 56 (44) | 91% | 73% | |
| Rai stage: 0 | 103 (80) | 87% | 77% | <0.0001 |
| 1,2,3,4 | 25 (20) | 49% | 18% | |
| Lymphocyte count: < 20×109/l | 108 (84) | 85% | 60% | <0.0001 |
| ≥20×109/l | 20 (16) | 40% | 40% | |
| Lymphocyte doubling time ≥ 12m | 111 (87) | 84% | 68% | 0.001 |
| <12 m | 17 (13) | 50% | 22% | |
| CD38 <20% | 99 (77) | 83% | 67% | 0.006 |
| ≥20% | 29 (23) | 62% | 36% | |
| Parameter . | N (%) . | 5-y PFS . | 10-y PFS . | p value (UVA)* . |
|---|---|---|---|---|
| *Univariate analysis | ||||
| Sex: Male | 71 (56) | 67% | 43% | 0.01 |
| Female | 56 (44) | 91% | 73% | |
| Rai stage: 0 | 103 (80) | 87% | 77% | <0.0001 |
| 1,2,3,4 | 25 (20) | 49% | 18% | |
| Lymphocyte count: < 20×109/l | 108 (84) | 85% | 60% | <0.0001 |
| ≥20×109/l | 20 (16) | 40% | 40% | |
| Lymphocyte doubling time ≥ 12m | 111 (87) | 84% | 68% | 0.001 |
| <12 m | 17 (13) | 50% | 22% | |
| CD38 <20% | 99 (77) | 83% | 67% | 0.006 |
| ≥20% | 29 (23) | 62% | 36% | |
Progression free survival based on the number of risk factors for disease progression (p<0.00001)
Progression free survival based on the number of risk factors for disease progression (p<0.00001)
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal