Abstract
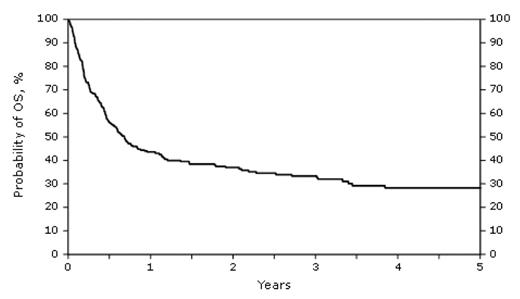
The prognosis of patients (pts) with NHL who relapse after autoHCT is poor. Myeloablative allogeneic hematopoietic stem cell transplantation has been utilized in these pts since the allograft is tumor free and may induce a graft-versus-tumor effect. Unfortunately, this approach results in prolonged survival for only a minority of pts. NMHCT is increasingly utilized in this setting since it affords the potential benefits of myeloablative transplantation and may reduce morbidity and treatment-related mortality (TRM). Reports using this approach show conflicting results but are limited by small numbers of pts. The purpose of this study was to determine the outcome of pts with NHL who underwent NMHCT after autoHCT failure including TRM, progression/relapse rate, overall survival (OS) and progression free survival (PFS). The study included 267 pts who underwent NMHCT for relapsed B cell NHL after autoHCT failure, from 1997 to 2006 and reported to the Center for International Blood and Marrow Transplant Research. Patients younger than 21, pts who underwent planned second transplants and recipients of cord blood transplants were excluded. The median age at NMHCT was 52 yrs (range 23–70); 64% were male and 61% had a Karnofsky Performance Score (KPS) of ≥ 90%. Fifty six percent of pts had diffuse large cell lymphoma, immunoblastic or follicular large cell lymphoma; 17% had follicular small or mixed NHL and 27% had mantle cell lymphoma. The time interval from 1st to 2nd transplant was < 1 year in 21% of pts, 1 to 2 years in 30% and > 2 years in 49% of pts. At the time of NMHCT, 63% had chemosensitive NHL, 31% resistant NHL and 6% were untreated after autoHCT. Multiple conditioning regimens were used including most frequently melphalan (25%) busulfan (21%) and fludarabine ± cyclophosphamide (26%). A fourth of the pts received 200 cGy of total body irradiation (TBI) as part of the conditioning regimen. The graft source was peripheral blood in 78% and 90% used unrelated donors. Median follow up of survivors was 37 months. TRM at 3 years was 42%. The cumulative incidence of disease progression at 3 years was 36%. The three-year probabilities of OS (figure 1) and PFS were 33% and 22%, respectively. The incidence of grade II-IV acute graft-versus-host disease (AGVHD) at 100 days was 39% and the incidence of chronic GVHD at 3 years was 41%. The most frequent causes of death were progression of NHL (29%), infection (19%), multiorgan failure (19%) and GVHD (14%). Factors associated with a lower risk of NHL progression or death include KPS ≥ 90%, interval between transplants >24 months, TBI as part of the conditioning regimen and complete remission at the time of NMHCT (figure 2). AGVHD decreased the risk of relapse (RR = 0.59, p=0.036)
Disclosures: No relevant conflicts of interest to declare.
supporting the role of a graft vs. lymphoma effect. We conclude that select pts with B cell NHL who undergo NMHCT for relapse after autoHCT attain a prolonged remission, despite the high TRM associated with this approach.
Author notes
Corresponding author


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal