Abstract
Background: Primary systemic amyloidosis (AL) is an incurable plasma cell disorder associated with varying degree of organ infiltration with light chain derived amyloid protein and consequent organ dysfunction. Various acquired coagulopathies, predominantly Factor X (FX) deficiency have been previously described in AL. The factor deficiencies are thought to be due to the direct binding of blood coagulation proteins to amyloid fibrils. Little is known regarding the prognostic significance of abnormal coagulation parameters in AL patients (pts).
Methods: After Institutional Review Board approval, we performed a retrospective review of the medical records of 625 consecutive pts who had presented within 3 months of a diagnosis of AL to be evaluated at Mayo Clinic from June 2001 to June 2006. 540 pts had coagulation studies performed within 2 months of presentation. 51 of those pts were on oral anticoagulation and were excluded from the analysis.
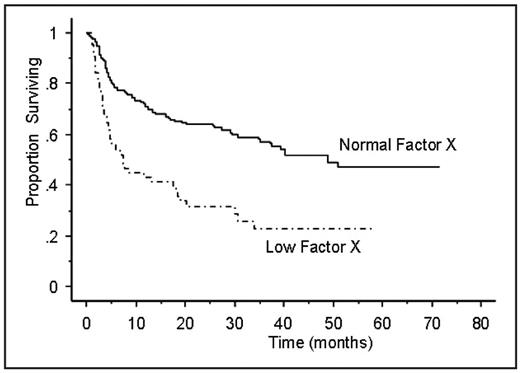
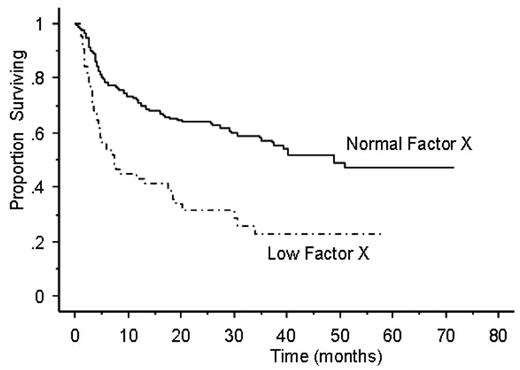
Results: Of the 489 pts included in the analysis, the median age was 62 years and 61% were male. The median overall survival (OS) of the entire cohort was 26.8 months. Table 1 lists the prevalence of abnormal coagulation tests in the remaining 489 patients. Prothrombin time (PT) was available in the majority of pts. 61 pts (12.6%) had elevated PT, and 63 pts (20.4%) had a decreased FX. 37 of the 61 pts with elevated PT had available FX levels, of which 31 (84%) of those had a decreased FX, suggesting that the cause of elevated PT was mostly due to a low FX. Indicators of hepatic involvement such as alkaline phosphatase and bilirubin levels were higher among the patients with prolonged PT and low FX. An elevated PT (more than 12.4 seconds) was strongly predictive of an adverse outcome, with a median OS of 8.7 months compared to a median OS of 29 months (p<0.0001) in pts with normal PT (Figure 1). Similarly, pts with decreased FX (less than 60% activity), was associated with significantly worse outcomes with a median OS of 14.9 months versus a median OS of 33 months (p<0.0001) in pts with normal FX (Figure 2). In a Cox proportional hazards model containing cardiac troponin (cTnT), NT-Pro BNP, serum alkaline phosphatase, and free light chain difference (involved minus uninvolved), prolonged PT or FX deficiency were independently prognostic for overall survival.
Conclusion: Abnormalities of PT and FX are seen in a sizable proportion of pts with newly diagnosed AL. An elevated PT and or FX deficiency appear to adversely affect the outcome of these patients. It is likely that the elevated PT in these patients relate to FX deficiency in the majority which in turn may reflect the amyloid ‘burden’. The effect of other organ involvement like the hepatic involvement may also have an impact on FX and PT.
Table 1. Prevalence of abnormal coagulation testing in patients with newly diagnosed primary systemic amyloidosis.
| Coagulation study . | N (Test results available) . | N of abnormal results . | (%) . |
|---|---|---|---|
| Elevated prothrombin time | 486 | 61 | 12.6 |
| Elevated activated partial thromboplastin time | 312 | 48 | 15.4 |
| Elevated thrombin time | 315 | 84 | 26.7 |
| Elevated fibrinogen | 140 | 118 | 84.3 |
| Decreased Factor II activity | 62 | 26 | 41.9 |
| Decreased Factor V activity | 63 | 9 | 14.3 |
| Decreased Factor VII activity | 63 | 17 | 27 |
| Decreased Factor X activity | 309 | 63 | 20.4 |
| Elevated D-dimer | 130 | 72 | 55.4 |
| Coagulation study . | N (Test results available) . | N of abnormal results . | (%) . |
|---|---|---|---|
| Elevated prothrombin time | 486 | 61 | 12.6 |
| Elevated activated partial thromboplastin time | 312 | 48 | 15.4 |
| Elevated thrombin time | 315 | 84 | 26.7 |
| Elevated fibrinogen | 140 | 118 | 84.3 |
| Decreased Factor II activity | 62 | 26 | 41.9 |
| Decreased Factor V activity | 63 | 9 | 14.3 |
| Decreased Factor VII activity | 63 | 17 | 27 |
| Decreased Factor X activity | 309 | 63 | 20.4 |
| Elevated D-dimer | 130 | 72 | 55.4 |
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal