Abstract
Iron induced cardiomiopathy is the main cause of mortality in thalassemic population. Thus, the improvement of chelation regimens, to reduce cardiac disease, has the highest priority. Efficient evaluation of cardiac iron status and careful epidemiologic assessment of thalassemic patients play an important role in this matter. T2* magnetic resonance imaging (MRI) is a unique technique to quantify myocardial iron overload and useful to tailor the chelation therapy. Effective and reproducible assessment of myocardial iron loading using the multislice multiecho T2* approach for segmental and global myocardial iron distribution, has been demonstrated at the MRI centre in Pisa [1,2]. Aim of this work is to build within the MIOT (Myocardial Iron Overload in Thalassemia) project a reliable network of haematological and paediatric centers specializing in thalassemia care and MRI centers able to perform feasible and reproducible heart and liver iron overload assessments for a consistent number of thalassemia patients in a standardized and robust manner.
First, the transferability of the multislice multiecho T2* technique was assessed. Heart multislice multiecho T2* and liver multiecho T2* sequences were installed on 1.5 T MRI scanners (GE Healthcare) at six different sites in Italy. Five healthy subjects at each site (n=30) were scanned to verify the homogeneity of normal ranges (T2* lover limit of normal 20ms). Then, five thalassemia major (TM) patients were scanned at the reference site and were rescanned locally (n=25) within one month. T2* images were analysed using a previously validated software (HIPPO MIOT®). T2* values of healthy subjects showed inter-sites homogeneity. On TM patients, for global heart T2* values the correlation coefficient was 0.97, Coefficients of Variation (CoVs) ranged from 0.04 to 0.12 and Intraclass Coefficients (ICCs) ranged from 0.94 to 0.99. The mean CoV and ICC for segmental T2* distribution were 0.198 and 88, respectively.
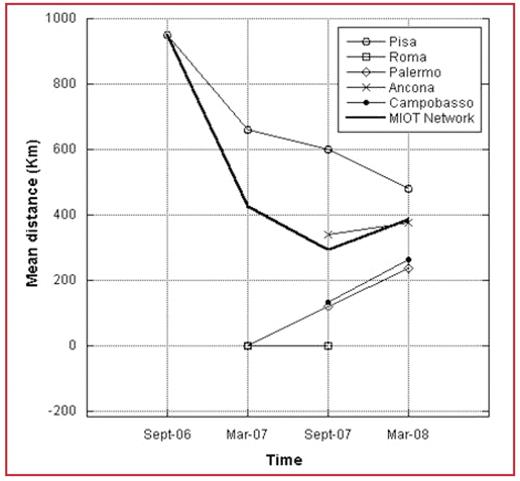
After the assessment of MRI technique reproducibility, patients enrolling started in September 2006. Since the project’s beginning, 695 thalassemia patients have been involved in the network. Six hundred and thirteen patients (88%) successfully underwent MRI examination. Each MRI center had a specific absorption capacity that seemed to remain constant over time, but the network was capable of sustaining an increasing number of patients due to continuous enrolment of new centers. The mean distance from the patients’ home locations to the MRI centers where the patients underwent the exams, which is considered an indicator of patient comfort, significantly decreased during the network’s evolution. In Figure, the average distances from the thalassemia centers which sent the patients for MRI examination are plotted versus time. With the activation of delocalized MRI centers, average distances tend to be comparable.
In conclusion, the multislice multiecho T2* technique is transferable among scanners with good reproducibility. The MIOT network seems to be a robust and scalable system in which T2* MRI-based cardiac and liver iron overload assessment is available, accessible and reachable for a significant and increasing number of thalassemia patients in Italy, reducing the mean distance from the patients’ locations to the MRI sites. A solid, wide and homogeneous database will constitute an important scientific resource, shortening the time scale for diagnostic, prognostic and therapeutical evidence-based research on the management of thalassemia disease.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal