Abstract
Background: a-thalassaemia is known to be prevalent in the Sultanate of Oman. However, there are no studies on the effects of a-thalassaemia on red cell indices in the new born children from the Sultanate of Oman.
Materials & Methods: In a prospective study over a period of 2 years, cord blood samples from 7837 neonates, from the two prominent cities i.e Muscat and Sohar in the Sultanate of Oman, were analyzed for complete blood counts [CBC] and high performance chromatography[HPLC]; as part of ongoing studies related to the national neonatal cord blood screening programme. HPLC was performed on the Biorad Variant II™ using the beta thalassaemia short programme for qualitative assessment and alpha thalassaemia short programme for quantitation of Haemoblobin Barts, which was considered as diagnostic of alpha thalassaemia on the cord blood samples.(Biorad Laboratories, Hercules, CA, USA) The positive samples were then further studied with molecular methods for confirmation by GAP PCR with direct sequencing and Genescan studies on ABI 3100 Genetic Analyzer®. (Applied Biosystems, Foster City, CA, USA)
Results: There were 4042 samples(51.58%) with normal HPLC (HbA + HbF). [Table] The remaining 3795 cases(48.42%) were associated elevated Hb Barts, indicative of the presence of a-thalassaemia. Amongst these subjects, 229 cases additionally also had HbS, 28 cases had HbD, 30 cases had HbE, and 3 cases had HbC. Overall, a total of 773 cases (9.86%) showed an abnormal hemoglobin like HbS(429), HbC(6), HbD(73), HbE (60)or beta thalassaemia(206).
Reference range for Cord Blood in Ethnic Omani newborn children(Mean ± SD)
| . | Hb . | RBC . | Hct . | MCV . | MCH . | MCHC . | RDW . | HbA . | HbF . |
|---|---|---|---|---|---|---|---|---|---|
| . | (g/dl) . | (×1012/L) . | (%) . | (fl) . | (pg) . | (g/dl) . | (CV%) . | % . | % . |
| †Significant (P<0.05) compared with Normal (A+F) | |||||||||
| #Barts Subgroups classified as per alpha thalassaemia short programme [Manufacturer’s instructions] | |||||||||
| Normal [A+F] | 15.38 ±2.04 | 4.69 ±0.68 | 50.5 ±7.18 | 107.66 ±7.75 | 33.61±4.07 | 30.98 ±3.44 | 17.01 ±2.17 | 22.88±8.03 | 77.02±8.04 |
| a-thal [A+F+Barts] | 14.79† ±2.9 | 5.09† ±0.77 | 49.7† ±7.4 | 97.29† ±13.8 | 29.74† ±11.8 | 30.39† ±3.6 | 18.09† ±2.56 | 25.74† ±9.05 | 73.96† ±8.91 |
| #Barts <1% N=625 | 15.81 ±1.58 | 4.54 ±0.52 | 47.92 ±5.03 | 105.72 ±5.64 | 34 ±2.27 | 33.03 ±1.23 | 16.27 ±1.24 | 23.78 ±8.6 | 81.55 ±10.2 |
| #Barts 1–3% N=1847 | 15.78 ±2.03 | 4.74 ±0.66 | 48.25 ±6.99 | 101.57 ±5.44 | 33.38 ±2.69 | 32.71 ±1.17 | 16.25 ±6.46 | 21.14 ±8.1 | 84.65 ±9.75 |
| #Barts 3–10% N=1323 | 14.96 ±2.01 | 5.29 ±0.69 | 47.46 ±6.8 | 89.87 ±5.39 | 28.47 ±2.1 | 31.65 ±1.39 | 17.3 ±1.82 | 24.11 ±8.5 | 81.42 ±9.5 |
| . | Hb . | RBC . | Hct . | MCV . | MCH . | MCHC . | RDW . | HbA . | HbF . |
|---|---|---|---|---|---|---|---|---|---|
| . | (g/dl) . | (×1012/L) . | (%) . | (fl) . | (pg) . | (g/dl) . | (CV%) . | % . | % . |
| †Significant (P<0.05) compared with Normal (A+F) | |||||||||
| #Barts Subgroups classified as per alpha thalassaemia short programme [Manufacturer’s instructions] | |||||||||
| Normal [A+F] | 15.38 ±2.04 | 4.69 ±0.68 | 50.5 ±7.18 | 107.66 ±7.75 | 33.61±4.07 | 30.98 ±3.44 | 17.01 ±2.17 | 22.88±8.03 | 77.02±8.04 |
| a-thal [A+F+Barts] | 14.79† ±2.9 | 5.09† ±0.77 | 49.7† ±7.4 | 97.29† ±13.8 | 29.74† ±11.8 | 30.39† ±3.6 | 18.09† ±2.56 | 25.74† ±9.05 | 73.96† ±8.91 |
| #Barts <1% N=625 | 15.81 ±1.58 | 4.54 ±0.52 | 47.92 ±5.03 | 105.72 ±5.64 | 34 ±2.27 | 33.03 ±1.23 | 16.27 ±1.24 | 23.78 ±8.6 | 81.55 ±10.2 |
| #Barts 1–3% N=1847 | 15.78 ±2.03 | 4.74 ±0.66 | 48.25 ±6.99 | 101.57 ±5.44 | 33.38 ±2.69 | 32.71 ±1.17 | 16.25 ±6.46 | 21.14 ±8.1 | 84.65 ±9.75 |
| #Barts 3–10% N=1323 | 14.96 ±2.01 | 5.29 ±0.69 | 47.46 ±6.8 | 89.87 ±5.39 | 28.47 ±2.1 | 31.65 ±1.39 | 17.3 ±1.82 | 24.11 ±8.5 | 81.42 ±9.5 |
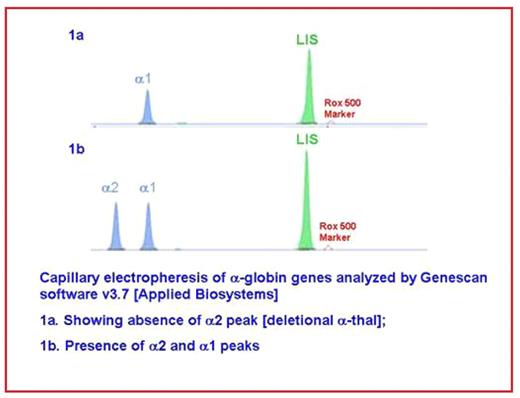
Hb Barts levels between 1–3% and 3–10% were seen amongst 48.68% and 34.87% cases respectively. Genescan studies revealed that 61.23% cases had nondeletional type and 38.77% subjects showed deletional.(-a3.7 ) types of a-thalassaemia.[figure] which were confirmed by GAP PCR for deletional cases whereas in non-deletional cases both a2 and a1 genes were selectively amplified and directly sequenced.
Conclusions : The incidence a-thalassaemia in this cohort of neonates was 48.42%. a-thalassaemia gene significantly reduced the MCV, MCH, MCHC, Hct, RBC count and the Hb and increased the RDW in the cord blood samples of neonates screened in this study. There was an excellent correlation between qualitative and quantitative estimation of Hb Barts by the two techniques. Importantly, we did not encounter any case of Hb H disease or hydrops faetalis in this study.
Disclosures: Alkindi:Sultan Qaboos University Hospital: Research Funding.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal