Abstract
Background: Recent literature suggests that statins may have anticancer potential. This effect is thought to be mediated through 2 primary mechanisms - impairment of protein prenylation and interference with the formation of cholesterol-rich lipid microdomains, or “lipid rafts” within the cell membrane. Both of these processes are critical for signaling activity of numerous proteins important for lymphomagenesis and tumor survival. Recent data, however, suggest that statin use may directly inhibit rituximab binding to CD20 and therefore rituximab efficacy. These findings raised significant concerns about statin use during rituximab treatment. Here we report on statin use and clinical outcome in a cohort of FL and DLBCL treated patients, most of whom were treated with rituximab containing regimens.
Methods: 293 newly diagnosed FL patients and 228 newly diagnosed DLBCL patients were prospectively enrolled in our Lymphoma SPORE registry from 9/2002 through 6/2007. Pathology was centrally reviewed. All patients were followed for retreatment, progression-free and overall survival. Statin use at the time of diagnosis and time of initial treatment was abstracted from the medical record. An event was defined by disease progression, retreatment, or death due to any cause.
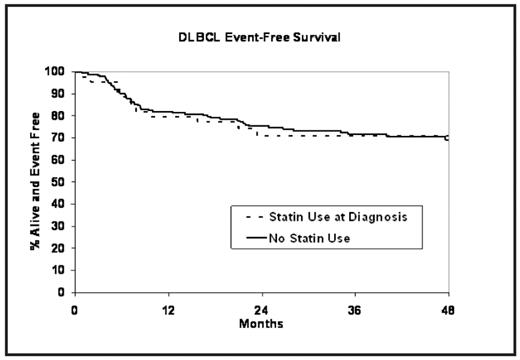
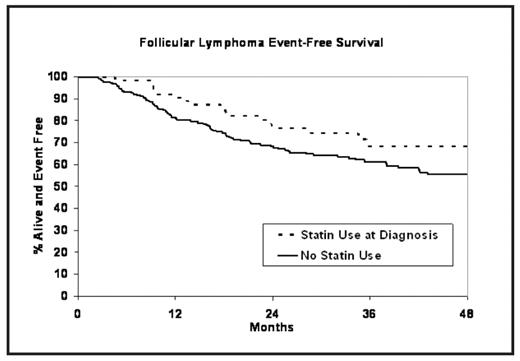
Results: 19% of FL patients and 22% of DLBCL patients were on statins at diagnosis; 16% and 19% were on statins during treatment, respectively. Initial therapy for the FL patients was observation (40%), R-CHOP (19%), R-CVP (12%), rituximab alone (8%), CVP (7%), RT (6%), and other (8%). All DLBCL patients received rituximab with CHOP or a CHOP-like regimen. At a median follow-up of 36 months (range 3–73), 109 (37%) and 65 (29%) of FL and DLBCL patients had an event; 19 (6%) and 46 (20%) of FL and DLBCL patients died, respectively. After adjusting for FLIPI, grade, and initial therapy type, statin use at diagnosis was associated with better event-free survival (HR = 0.57, 95% CI: 0.34–0.95, p=0.03) in FL patients. Statin use during treatment in FL patients was also associated with better event-free survival, though not statistically significant (HR = 0.67, 95% CI: 0.39–1.16, p=0.15). The improvement in EFS for FL patients was consistent across initial therapies, including observation. Statin use was not associated with IPI-adjusted overall survival or event-free survival in DLBCL (all p > 0.50).
Conclusions: Statin therapy does not appear to be associated with inferior clinical outcome in DLBCL treated with rituximab and CHOP or CHOP-like therapy. Therefore direct inhibition of rituximab binding to CD20 may have limited clinical significance or/and may be overcome by inhibitory impact of statins on cell signaling. The latter possibility is supported by our observation that statin use is associated with improved event-free survival in follicular lymphoma.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal