Abstract
Vascular endothelial growth factor (VEGF)–A regulates vascular development and angiogenesis. VEGF isoforms differ in ability to bind coreceptors heparan sulfate (HS) and neuropilin-1 (NRP1). We used VEGF-A165 (which binds HS and NRP1), VEGF-A121 (binds neither HS nor NRP1), and parapoxvirus VEGF-E-NZ2 (binds NRP1 but not HS) to investigate the role of NRP1 in organization of endothelial cells into vascular structures. All 3 ligands induced similar level of VEGFR-2 tyrosine phosphorylation in the presence of NRP1. In contrast, sprouting angiogenesis in differentiating embryonic stem cells (embryoid bodies), formation of branching pericyte-embedded vessels in subcutaneous matrigel plugs, and sprouting of intersegmental vessels in developing zebrafish were induced by VEGF-A165 and VEGF-E-NZ2 but not by VEGF-A121. Analyses of recombinant factors with NRP1-binding gain- and loss-of-function properties supported the conclusion that NRP1 is critical for VEGF-induced sprouting and branching of endothelial cells. Signal transduction antibody arrays implicated NRP1 in VEGF-induced activation of p38MAPK. Inclusion of the p38MAPK inhibitor SB203580 in VEGF-A165–containing matrigel plugs led to attenuated angiogenesis and poor association with pericytes. Our data strongly indicate that the ability of VEGF ligands to bind NRP1 influences p38MAPK activation, and formation of functional, pericyte-associated vessels.
Introduction
Vascular endothelial growth factor (VEGF)–A regulates endothelial cell function by binding to 2 structurally similar receptor tyrosine kinases, denoted VEGF receptor-1 and -2 (VEGFR-1 and -2).1 VEGFR-2 is the main transducer of VEGF-A effects on endothelial cell differentiation, proliferation, migration, and formation of the vascular tube. The signal transduction properties of VEGFR-2 regulating these responses are incompletely understood, although the contributions of different phosphorylation sites are being unraveled.2 Replacement of tyrosine 1173 (Y1175 in the human sequence) in VEGFR-2 for phenylalanine results in loss of binding of phospholipase Cγ1 (PLCγ1) and the adaptor molecule Shb.1 Signaling downstream of Y1173 is of critical importance in VEGF-A165–induced proliferation.3 In accordance, mutant vegfr2Phe1173 embryos die at E9.5, displaying a phenotype mimicking that of vegfr2−/− embryos.4 In addition, Y949 (Y951 in the human sequence) in the kinase insert regulates binding of the adaptor molecule T cell–specific adaptor and Src activation,2 whereas Y1212 (Y1214) regulates activation of p38 mitogen-activated protein kinase (MAPK).5
Differential splicing of the vegfa gene regulates interactions with coreceptors heparan sulfate proteoglycans (HSPGs) and neuropilins (NRPs).6 VEGF-A165 (VEGF-A164 in mice) includes exon 7 and binds with high affinity to HSPGs and NRPs, whereas VEGF-A121 (VEGF-A120 in mice) lacks this exon and should bind to none of the coreceptors. However, recent data indicate the involvement of exon 8 in the vegfa gene in NRP1 binding7 ; consequently, VEGF-A121 may also interact with NRP1.8
NRP1 and NRP2 are transmembrane proteins with small cytoplasmic domains lacking intrinsic catalytic function.9 The NRPs were first identified as receptors for the soluble class 3 semaphorins, which serve in axon guidance.10,11 Subsequently, NRP1 was shown to bind exon 7–containing VEGF-A isoforms, such as VEGF-A165.12 Targeted inactivation of the mouse nrp1 gene leads to severe defects in both neuronal and vascular development.13 Recently, blocking VEGF-A–binding to NRP1 was shown to be additive to blocking VEGF-A–binding to VEGFR-2, in inhibition of tumor growth.14 HSPGs are trans-membrane, glycosyl-phosphatidylinositol-anchored or secreted proteins with covalently linked HS chains. HSPGs modulate the activity of a large number of secreted signaling molecules, by stabilizing the ligand/receptor complex.15 The mode of presentation of VEGF by HS regulates VEGFR-2 turnover and the longevity of downstream signaling.16
The aim of the present study was to deduce the contribution of NRP1 to VEGF-A/VEGFR-2 signaling during vessel formation. For this purpose, we compared the properties of VEGF-A165 and VEGF-A121 with those of VEGF-E-NZ2, a pox virus–derived VEGF-homolog,17 which is structurally highly related to VEGF-A.18 This strategy, combined with the use of gain- and loss-of-function VEGF variants, allowed us to distinguish the role of NRP1 binding separate from HS binding. Our data indicate that ligand binding to NRP1 is of critical importance for proper organization of endothelial cells to form the vascular tube.
Methods
Antibodies, growth factors, and inhibitors
The following antibodies were used: anti–Flk-1 (C-1158), antineuropilin (H-286), antineuropilin (C-19), anti-βactin (C-11; Santa Cruz Biotechnology, Santa Cruz, CA); anti–mouse VEGFR2 (#AF644), anti–human VEGFR2 (R&D Systems, Minneapolis, MN); purified rat anti–mouse Flk-1 monoclonal, primary rat anti–mouse CD31 (BD Biosciences, San Jose, CA); antiphosphoVEGF receptor 2/3 (Calbiochem, San Diego, CA); anti-p44/42 MAP kinase, antiphospho-p44/42 MAP kinase (Thr202/Tyr204), anti-p38 MAP kinase (L53F8) mouse monoclonal, anti-Akt (#9272), phospho-Akt (Ser473; Cell Signaling Technology, Danvers, MA). IRDye 800–conjugated protein A-purified murine monoclonal antiphosphotyrosine, IRDye 800–conjugated affinity purified anti–goat IgG (Rockland Immunochemicals, Gilbertsville, PA); mouse monoclonal antiphosphotyrosine 4G10 (Upstate Biotechnology, Charlottesville, VA); mouse IgM antiheparan sulfate (HepSS1; Seikagaku Biobusiness, Tokyo, Japan); enhanced chemiluminescence (ECL) anti–rabbit IgG, horseradish peroxidase-linked whole antibody (GE Healthcare, Little Chalfont, United Kingdom); anti–goat IgG-peroxidase (A4174), mouse monoclonal anti–α-smooth muscle actin-fluorescein isothiocyanate conjugate (Sigma-Aldrich, St Louis, MO); Alexa 680 goat anti–mouse IgG, Alexa 555 goat anti–rat IgG, Alexa 488 donkey anti–rabbit IgG, Alexa 555 donkey anti–goat IgG, Alexa 555 goat anti–mouse IgM, Alexa 488 donkey anti–rat IgG, Alexa 594 donkey anti–rat IgG (Invitrogen, Carlsbad, CA); biotinylated goat anti–rat IgG (Vector Laboratories, Burlingame, CA). Rabbit antiserum (RS-2) was raised against the kinase insert domain of human VEGF receptor-2.19 Anti–mouse NRP1 antibody was kindly provided by Dr Hajime Fujisawa (21st Century COE Program, Division of Biological Science, Nagoya University Graduate School of Science, Nagoya, Japan).
VEGF-A165 was from PeproTech (Rocky Hill, NJ) and VEGF-A121 from R&D Systems. The VEGF-A121 from R&D Systems is truncated in the C-terminus and contains a VEGF-A112 form, but as described in “Discussion,” we kept the designation “VEGF-A121” in this study. VEGF-E-NZ2 was produced as described.18
VEGF-E-NZ2 and VEGF-A-NZ2 were cloned into the pPICZAlphaA (Invitrogen) and carried an amino-terminal His6-tag.20 VEGF-A-NZ2 denotes canine VEGF-A120 onto which a C-terminal extension (TTPPTTTRPPRRRR), corresponding to the NRP1-binding domain from VEGF-E-NZ2, has been fused. A loss-of-function VEGF-E-NZ2 variant was created by introducing E instead of R at position 126 (VEGF-E-R126E). See Cébe-Suarez et al,21 for basic characterization of gain- and loss-of-function properties of VEGF-A-NZ2 and VEGF-E-R126E. All proteins carried an alpha factor secretory signal for export into the extracellular milieu. Pichia pastoris strain X33 was transfected and tested for expression of the transgene on induction for 2 to 4 days with 0.5% methanol. Secreted protein was purified by immobilized metal-ion affinity chromatography and polished on Superdex 200 (GE Healthcare). The correctness of the proteins was verified by amino-terminal sequencing.
The p38MAPK inhibitor SB203580 (Calbiochem) was used at concentrations of 5 to 10 μM (IC50, 34-600 nM). The activity of stress kinases, such as JNK or p42 MAPK, should not be affected under 100 μM of SB203580. The inhibitor was dissolved in dimethyl sulfoxide, which was diluted to a final concentration less than 0.01%.
Tissue culture
Porcine aortic endothelial (PAE)/VEGFR-2 cells have been described.12 PAE/VEGFR-2, NRP1 cells were established by transfection of PAE/VEGFR-2 cells with human NRP1 cDNA in pcDNA3.1 mixed with pSuper.retro.puro (Oligoengine, Seattle, WA), using Lipofectamine (Invitrogen). R1/SVJ 129 murine embryonic stem (ES) cells were kindly provided by Dr Andras Nagy (Samuel Lunenfeld Research Institute, Mount Sinai Hospital, Toronto, ON). Creation of embryonic stem cell aggregates (embryoid bodies; EBs) and their differentiation in 2- or 3-dimensional (2D or 3D) cultures have been described.16
Peroxidase/fluorescent immunostaining of embryoid bodies
EBs in 2D cultures or in 3D collagen I were fixed and permeabilized in zinc fix (0.1 M of Tris-HCl, pH 7.5, 3 mM of calcium acetate, 23 mM of zinc acetate, 37 mM of zinc chloride, 0.2% Triton X-100), and blocked in Tris-buffered saline (TBS)/0.05% to 0.1% Tween-20/3% bovine serum albumin (BSA/TBS-t). For fluorescent staining, EBs were fixed in zinc fix solution or 4% p-formaldehyde/TBS and permeabilized in TBS/0.2% Triton X-100/3% BSA. Samples were incubated with primary and secondary antibodies in BSA/TBS-t. Peroxidase staining was developed using horseradish peroxidase-conjugated streptavidin (Vector Laboratories) and the chromogen substance (AEC kit; Vector Laboratories). Mounting was done using Ultramount aqueous permanent mounting medium (Dako, Glostrup, Denmark). Samples were inspected using a Nikon Eclipse E1000 microscope with a Nikon Eclipse DXM 1200 camera (Nikon, Tokyo, Japan) or a Zeiss LSM 510 META confocal microscope (Carl Zeiss, Oberkochen, Germany). Quantification of CD31-positive area was performed using the Easy Image Analysis software (Tekno Optik, Stockholm, Sweden).
Immunoprecipitation/immunoblotting
Cells were lysed in 1% NP40 and processed for immunoprecipitation/immunoblotting as described.2 p38MAPK activity was measured by immune complex kinase assay using the p38MAP kinase assay kit (Cell Signaling Technology) with an immobilized phosphop38MAPK antibody and activating transcription factor-2 (ATF-2) protein as a substrate, and blotting with a phospho-ATF-2 antibody. Blots were developed using ECL (GE Healthcare) or using an Odyssey infrared imaging system. Densitometric analysis of fluorographs was performed using the ImageJ 1.31 software (http://rsb.info.nih.gov/ij/download.html), and results are given as mean plus or minus SD.
Filter binding assay
HS was purified from PAE/VEGFR-2 cells after 16 hours metabolic labeling with [35S]sulfate (PerkinElmer Life and Analytical Sciences, Waltham, MA). Triplicate samples of ligands (26.2 nmol) were incubated with 4 × 103 cpm [35S]HS in 200 μL of phosphate-buffered saline, and passed through a nitrocellulose filter using a multiwell vacuum-assisted filtration apparatus. After washing away unbound [35S]HS, filters were incubated in 2 M of NaCl to dissociate the HS. Protein-bound [35S]HS retained on the filter was determined using a Wallac 1414 liquid scintillation counter (PerkinElmer Life and Analytical Sciences).
Matrigel plug assay
Animal work was approved by the Uppsala University board of animal experimentation and performed according to the United Kingdom Co-ordinating Committee on Cancer Research guidelines for the welfare of animals in experimental neoplasia. Six-week-old female nude mice were anesthetized with isoflurane (Forene; Abbott Scandinavia, Solna, Sweden) and subcutaneously injected with 350 μL of matrigel (BD Biosciences) supplemented with sphingosine-1-phosphate (S1P; Avanti Polar Lipids, Alabaster, AL) with or without 2 μg (130 nM) of VEGF-A165, VEGF-A121, and VEGF-E-NZ2. When indicated, 10 μM of SB203580 was included in the matrigel together with S1P and VEGF-A165. Mice were killed 7 days later, and matrigel plugs with surrounding skin and muscles were retrieved and fixed in 4% paraformaldehyde, followed by whole mount staining. The angiogenic response was detected by immunostaining using rat antimouse CD31 (BD Biosciences) and fluorescein isothiocyanate-conjugated mouse anti–α-smooth muscle actin (ASMA), followed by incubation with Alexa 594 donkey antirat IgG (Invitrogen, Molecular Probes, Eugene, OR). Samples were analyzed using a Zeiss LSM 510 META confocal microscope. Three to 6 matrigel plugs/condition were inspected on 2 independent occasions.
Microscopy
Samples were analyzed using a Nikon Eclipse E1000 microscope with a Nikon Eclipse DXM 1200 camera (Nikon) or a LSM 510 META confocal microscope (Carl Zeiss). The following objectives were used: Nikon Plan Apochromat 2×/0.1, 4×/0.2, 10×/0.45, 20×/0.75; Zeiss confocal Fluar 20×/0.75 UV E) and Plan Apochromat 63×/1.4 oil immersion. The following software programs were used: ACT-1 (Nikon) and Laser Scanning Microscope LSM 510 version 3.2 (Carl Zeiss). Processing of microphotographs was done using Adobe Photoshop (Adobe Systems, San Jose, CA). Measurement of vascular density was done by calculating the stained area using Image Analysis 2000 software (Rainfall, Stockholm, Sweden).
Antibody array screening
Serum-starved PAE/VEGFR-2, NRP1 cells treated with 2 nM of VEGF-A165 or -A121 for 5 minutes were lysed in a 0.5% Triton X-100–containing buffer. The antibody array membrane (HM3000 Signal Transduction AntibodyArray; Hypromatrix, Worcester, MA) was treated in blocking buffer containing 0.01% Tween-20 followed by incubation with sample diluted in 1% dry milk/phosphate-buffered saline for 2 hours. The filter was blotted with IRDye 800–conjugated protein A-purified murine monoclonal antiphospho- tyrosine antibody followed by scanning using the Odyssey infrared imaging system and analysis using the ImageJ 1.31 software (http://rsb.info.nih.gov/ij/download.html). Phosphotyrosine spots with 2-fold higher background were excluded. Of the 400 antibodies on the filter, 113 captured molecules that are not known as substrates for tyrosine kinases; 205 potential tyrosine kinase substrates were not phosphorylated by VEGF-A165. Of the remaining 82 molecules, 24 were determined to be substrates, whereas 58 could potentially be phosphorylated at low stoichiometry but must be excluded because of uneven background.
Zebrafish procedures
Flil-Green fluorescent protein (GFP) zebrafish embryos,22 maintained at the Boston Children's Hospital breeding colony (28.5°C, 14 hours light/10 hours dark cycle), were collected from the natural mating of breeding pairs, staged as described. Embryos older than 24 hours postfertilization (hpf) were raised in 0.2 mM of 1-phenyl-2-thio-urea (Sigma-Aldrich) to prevent pigment formation. Vegfa morpholino (MO; directed against the AUG initiation codon)23 was diluted in Danieau buffer and injected into the embryo blastomere at the 1 to 4 cell stage. VegfeNZ2 cDNA18 and zebrafish vegfa121 and 165 were amplified by PCR and subcloned into pcDNA3.1/V5-His TOPO vector (Invitrogen). To avoid inhibiting translation of exogenous recombinant mRNA by MO in the MO-mRNA coinjection experiments, the signal peptide sequences of the vegfs were replaced through PCR, with the Ig kappa signal sequence, followed by subcloning into the pcDNA3.1/V5-His/TOPO vector. The expected expression, secretion, and activity of VEGF-A produced from these constructs were verified in an in vitro cell culture system. The Ig kappa signal sequence-V5 tagged-vegfa121, 165, or vegfeNZ2 were subcloned into the pXT7 vector (Promega) and used to make recombinant mRNA by mMessage-mMachine kit (Ambion, Austin, TX). Between 50 and 500 pg mRNA was injected/embryo. Living zebrafish embryos were visualized using a stereomicroscope (Olympus, Tokyo, Japan) and photographed.
Results
VEGFR-2 activation and contribution of coreceptors
We wished to study the contribution of NRP1 to VEGFR-2 signal transduction. To control formation of VEGFR-2 signaling complexes to include NRP1 or not, we used a panel of different naturally occurring VEGFs, or chimeric and point-mutated VEGFs, as outlined in Figure 1A. The VEGFs were first tested on PAE cells that lack endogenous VEGFR-2 and NRP1.12,24 Cells were transfected to stably express the human VEGFR-2 alone (PAE/VEGFR-2) or together with NRP1 (PAE/VEGFR-2, NRP1 cells; Figure 1B,C). The PAE cell clones expressed HS of similar composition and at equal levels (Figure S1, available on the Blood website; see the Supplemental Materials link at the top of the online article); therefore, the contribution of HS should be comparable in the subsequent analyses.
VEGF-A165, VEGF-A121, and VEGF-E-NZ2 interaction with VEGFR-2, HS, and NRP1. (A) Schematic outline of VEGF ligands used in this study with VEGF-A exon structure and bindings sites for VEGFR-2, HS, and NRP1 indicated. VEGF-A165 and VEGF-A121 were purchased or produced in-house by expressing canine cDNAs in Pichia pastoris. Similar results were obtained irrespective of source. VEGF-E-NZ2, VEGF-E-R126E (loss-of-function for NRP1 binding), and VEGF-A-NZ2 (gain-of-function for NRP1 binding) were also produced in Pichia pastoris (“Methods”). (B) PAE/VEGFR-2, NRP1 cells treated with 2 nM of VEGF-A165, VEGF-A121, or VEGF-E-NZ2 for 5 minutes were characterized by immunoprecipitation (IP)/immunoblotting (IB). Tyrosine phosphorylation of immunoprecipitated VEGFR-2 was detected by immunoblotting with antiphosphotyrosine mAb 4G10. Expression of VEGFR-2 and NRP1 was shown by immunoblotting on total cell lysates. The extent of VEGFR-2/NRP1 complex formation was assessed by immunoprecipitation of VEGFR-2 followed by immunoblotting for NRP1. The basal degree of complex formation in the absence of growth factors was set to 1. (C) PAE cells transfected with human VEGFR-2 and treated with 2 nM of the 3 VEGF ligands were analyzed for VEGFR-2 tyrosine phosphorylation as in panel B. Tyrosine phosphorylation of VEGFR-2 was induced by VEGF-A165 and VEGF-A121 but only inefficiently by VEGF-E-NZ2. Bottom panel shows equal VEGFR-2 loading. (D) [35S]HS retention on nitrocellulose filter as a consequence of specific binding to VEGF-A165. [35S]HS was not retained by incubation with VEGF-A121 or VEGF-E-NZ2.
VEGF-A165, VEGF-A121, and VEGF-E-NZ2 interaction with VEGFR-2, HS, and NRP1. (A) Schematic outline of VEGF ligands used in this study with VEGF-A exon structure and bindings sites for VEGFR-2, HS, and NRP1 indicated. VEGF-A165 and VEGF-A121 were purchased or produced in-house by expressing canine cDNAs in Pichia pastoris. Similar results were obtained irrespective of source. VEGF-E-NZ2, VEGF-E-R126E (loss-of-function for NRP1 binding), and VEGF-A-NZ2 (gain-of-function for NRP1 binding) were also produced in Pichia pastoris (“Methods”). (B) PAE/VEGFR-2, NRP1 cells treated with 2 nM of VEGF-A165, VEGF-A121, or VEGF-E-NZ2 for 5 minutes were characterized by immunoprecipitation (IP)/immunoblotting (IB). Tyrosine phosphorylation of immunoprecipitated VEGFR-2 was detected by immunoblotting with antiphosphotyrosine mAb 4G10. Expression of VEGFR-2 and NRP1 was shown by immunoblotting on total cell lysates. The extent of VEGFR-2/NRP1 complex formation was assessed by immunoprecipitation of VEGFR-2 followed by immunoblotting for NRP1. The basal degree of complex formation in the absence of growth factors was set to 1. (C) PAE cells transfected with human VEGFR-2 and treated with 2 nM of the 3 VEGF ligands were analyzed for VEGFR-2 tyrosine phosphorylation as in panel B. Tyrosine phosphorylation of VEGFR-2 was induced by VEGF-A165 and VEGF-A121 but only inefficiently by VEGF-E-NZ2. Bottom panel shows equal VEGFR-2 loading. (D) [35S]HS retention on nitrocellulose filter as a consequence of specific binding to VEGF-A165. [35S]HS was not retained by incubation with VEGF-A121 or VEGF-E-NZ2.
VEGFR-2 activation by the different VEGF ligands used (initially VEGF-A165, VEGF-A121, and VEGF-E-NZ2) was tested. In the presence of NRP1, the 3 ligands induced similar extent of VEGFR-2 tyrosine phosphorylation, indicative of its activation (Figure 1B). In dose-response analyses, VEGFR-2 tyrosine phosphorylation was similarly induced by the 3 ligands over a 0.2- to 5-nM concentration range (data not shown).
VEGF-E-NZ2 is known to bind to NRP1,17 as well as to VEGFR-2. In agreement, complex formation between VEGFR-2 and NRP1 was induced in PAE/VEGFR-2, NRP1 cells by VEGF-E-NZ2 as well as by VEGF-A165, but not by VEGF-A121 (Figure 1B). In the absence of NRP1, VEGF-E-NZ2 was several-fold less effective in activation of VEGFR-2 compared with the other ligands (Figure 1C). Therefore, VEGFR-2/NRP1 complex formation is important in VEGF-E-NZ2–induced VEGFR-2 activation. In agreement, the ability of VEGF-E-NZ2 to compete with 125I-VEGF-A165 for binding to PAE cells expressing VEGFR-2 or NRP1 individually or in combination was guided by NRP1 (Figure S2A-C).
The ability of the 3 VEGF ligands to bind to HS was examined using a nitrocellulose filter binding assay,25 where 35S-labeled HS produced by PAE/VEGFR-2 cells was retained on the filter only when in complex with protein. As shown in Figure 1D, HS was retained on the filter when bound to VEGF-A165, whereas VEGF-E-NZ2 and VEGF-A121 failed to bind and retain HS. Similar data were obtained when analyzing the capacity of the VEGF ligands to retain radiolabeled heparin (Figure S1C). We conclude that, in this simple cell model, binding of VEGF ligands (such as VEGF-A121 and VEGF-E-NZ2) to HS was not required for acute VEGFR-2 activation. This does not exclude that binding of VEGFR-2 to HS would be important in receptor activation. Moreover, because VEGF-E-NZ2 binds strongly to NRP1 but not to HS, it was possible to study the specific contribution of NRP1 to VEGFR-2 signaling.
Vascularization in differentiating embryonic stem cells and subcutaneous matrigel plugs
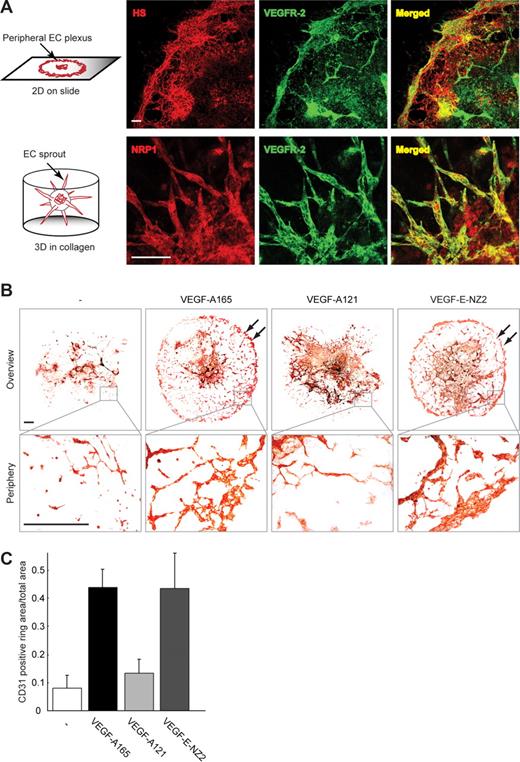
It has been shown that inclusion of NRP1 in the VEGFR-2 signaling complex promotes more efficient endothelial cell migration.12 In agreement, migration of PAE cells toward the NRP1-binding VEGFs was enhanced when cells coexpressed VEGFR-2 and NRP1 (data not shown). We now wished to examine the effects of the ligands in a more complex model. Hallmarks of vasculogenesis and angiogenesis are faithfully recapitulated in EBs, that is, differentiating embryonic stem cells subjected to 2D culture, or to 3D culture in collagen I.26 HS expression colocalized with immunostaining for VEGFR-2 in these cultures (Figure 2A top). NRP1 immunostaining showed coexpression of NPR1 and VEGFR-2 in angiogenic sprouts (Figure 2A bottom).
Embryoid body vessel development in response to different VEGF ligands. (A) Coexpression of HS and VEGFR-2 in 2D embryoid body (EB) cultures (top panels) and coexpression of NRP1 and VEGFR-2 in angiogenic sprouts in 3D EB cultures (bottom panels). Schematic representation of 2D (top) and 3D (bottom) cultures is shown to the far left. Scale bar represents 100 μm. (B) Formation of peripheral CD31-positive capillary plexus in 2D embryoid body cultures (↙ in top panels, see bottom panels for higher magnification) was induced in response to treatment with VEGF-A165 and VEGF-E-NZ2, but not VEGF-A121 or vehicle. Scale bar represents 300 μm. (C) Quantification of the CD31-positive peripheral capillary plexus area in panel B. The outer rim (defined as the outer 12.5% segment of the EB diameter) was quantified using the Image analysis 2000 software.
Embryoid body vessel development in response to different VEGF ligands. (A) Coexpression of HS and VEGFR-2 in 2D embryoid body (EB) cultures (top panels) and coexpression of NRP1 and VEGFR-2 in angiogenic sprouts in 3D EB cultures (bottom panels). Schematic representation of 2D (top) and 3D (bottom) cultures is shown to the far left. Scale bar represents 100 μm. (B) Formation of peripheral CD31-positive capillary plexus in 2D embryoid body cultures (↙ in top panels, see bottom panels for higher magnification) was induced in response to treatment with VEGF-A165 and VEGF-E-NZ2, but not VEGF-A121 or vehicle. Scale bar represents 300 μm. (C) Quantification of the CD31-positive peripheral capillary plexus area in panel B. The outer rim (defined as the outer 12.5% segment of the EB diameter) was quantified using the Image analysis 2000 software.
EBs in 2D cultures treated with VEGF-A165 and VEGF-E-NZ2 presented the typical vascular plexus in the periphery of the culture (Figure 2B). In contrast, VEGF-A121 failed to induce formation of vessel structures (Figure 2C for quantification); instead, endothelial cells appeared arrested in sheets of cells in the EB center. Flow-sorting of dispersed EBs after treatment with VEGF-A165, VEGF-A121, and VEGF-E-NZ2 showed a 1.8- to 2.7-fold increase in the number of endothelial cells compared with untreated EBs. These data clearly demonstrate bioactivity by all 3 VEGF ligands in this model (Figure S3).
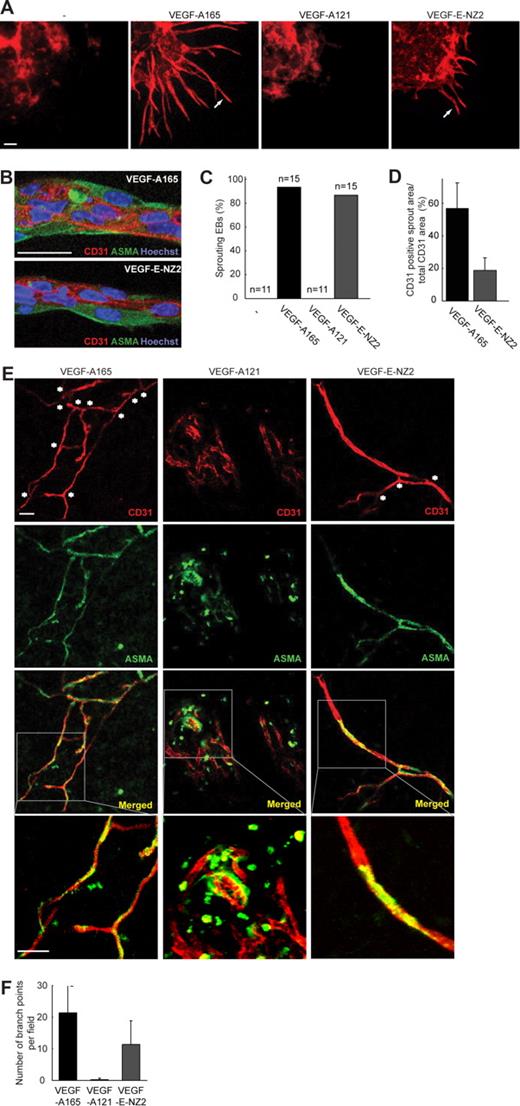
Angiogenic sprouting of EBs in 3D culture was induced by the NRP1-binding VEGF-A165 and VEGF-E-NZ2 but not by VEGF-A121 (Figure 3A,B; quantification in Figure 3C). Quantification of the sprout area showed that fewer endothelial cells were located in invading sprouts in the VEGF-E-NZ2 cultures than in the VEGF-A165 cultures (Figure 3D). Although the VEGF-E-NZ2–induced sprouts were shorter, the VEGF-A165– and VEGF-E-NZ2–induced sprouts showed a similar organization of CD31-positive endothelial cells surrounded by ASMA-positive pericyte-like cells (Figure 3B).
Sprouting angiogenesis and vessel formation in response to the different VEGF ligands. (A) Sprouting of EBs in 3D collagen cultures was induced in response to VEGF-A165 and VEGF-E-NZ2 (arrows) but not to VEGF-A121 or vehicle, as visualized by anti-CD31 immunostaining. The core of the EB is shown in the top left corner of each panel. Scale bar represents 100 μm. (B) Details of angiogenic sprouts formed in VEGF-A165–treated (top) or VEGF-E-NZ2–treated (bottom) EBs. Immunostaining shows expression of CD31 (red) and ASMA (green). Hoechst 33 342 (blue) staining indicates nuclei. Scale bar represents 100 μm. (C) Quantification of the number of EBs forming angiogenic sprouts in response to vehicle, VEGF-A165, VEGF-A121, or VEGF-E-NZ2. (D) Quantification of CD31-positive area in angiogenic sprouts in relation to total CD31 area. (E) Subcutaneous matrigel plugs containing VEGF-A165, VEGF-A121, or VEGF-E-NZ2, implanted for 7 days in nude mice. Whole-mount fixation was followed by staining for expression of CD31 (red) and ASMA (green) and analysis by confocal microscopy. Asterisks indicate branch points in VEGF-A165– and VEGF-E-NZ2–containing matrigel plugs. Microphotographs show projections of z-stacks of 50 μm. Bottom row of panels shows magnifications of areas indicated by white boxes in the merged panels above. Scale bars represent 50 μm. (F) Quantification of branch points in the different conditions by manual marking and counting of multiple samples (n = 4/condition).
Sprouting angiogenesis and vessel formation in response to the different VEGF ligands. (A) Sprouting of EBs in 3D collagen cultures was induced in response to VEGF-A165 and VEGF-E-NZ2 (arrows) but not to VEGF-A121 or vehicle, as visualized by anti-CD31 immunostaining. The core of the EB is shown in the top left corner of each panel. Scale bar represents 100 μm. (B) Details of angiogenic sprouts formed in VEGF-A165–treated (top) or VEGF-E-NZ2–treated (bottom) EBs. Immunostaining shows expression of CD31 (red) and ASMA (green). Hoechst 33 342 (blue) staining indicates nuclei. Scale bar represents 100 μm. (C) Quantification of the number of EBs forming angiogenic sprouts in response to vehicle, VEGF-A165, VEGF-A121, or VEGF-E-NZ2. (D) Quantification of CD31-positive area in angiogenic sprouts in relation to total CD31 area. (E) Subcutaneous matrigel plugs containing VEGF-A165, VEGF-A121, or VEGF-E-NZ2, implanted for 7 days in nude mice. Whole-mount fixation was followed by staining for expression of CD31 (red) and ASMA (green) and analysis by confocal microscopy. Asterisks indicate branch points in VEGF-A165– and VEGF-E-NZ2–containing matrigel plugs. Microphotographs show projections of z-stacks of 50 μm. Bottom row of panels shows magnifications of areas indicated by white boxes in the merged panels above. Scale bars represent 50 μm. (F) Quantification of branch points in the different conditions by manual marking and counting of multiple samples (n = 4/condition).
To validate the embryoid body data in an in vivo model, we used nude mice to study vascularization of subcutaneous matrigel plugs containing VEGF-A165, VEGF-A121, or VEGF-E-NZ2. Whole-mount CD31 immunostaining of the matrigel showed formation of branched vessels surrounded by ASMA-positive cells in plugs containing VEGF-A165 and VEGF-E-NZ2 (Figure 3E; quantification in Figure 3F). The extent of branching was higher for VEGF-A165, but there was a clear and reproducible effect of VEGF-E-NZ2 on endothelial cell organization. Plugs containing VEGF-A121 showed a markedly different pattern with clusters of endothelial cells that lacked close association with ASMA-positive perivascular cells. These data show that the NRP1-binding ligands VEGF-A165 and VEGF-E-NZ2 possessed the ability to induce endothelial cell organization in 2D and 3D EB cultures as well as in the subcutaneous matrigel plug in vivo assay. Although the non–NRP1-binding ligand VEGF-A121 induced potent VEGFR-2 activation, it failed to promote organization of endothelial cells.
Vessel formation induced by the 3 ligands in zebrafish embryos
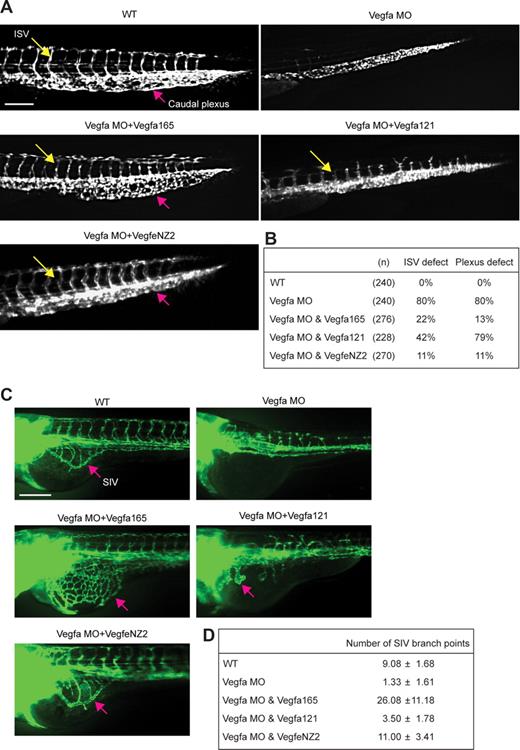
The zebrafish embryo has emerged as a useful tool to study vertebrate cardiovascular development.27,28 During zebrafish development, the intersegmental vessels (ISVs) originate bilaterally from the dorsal aorta and the posterior cardinal vein beginning around 20 hpf.29,30 ISV formation is marked by a stereotyped pattern of sprouting and dorsal migration of individual ECs at each somite boundary. To further study the angiogenic potential of the 3 VEGF ligands, zebrafish embryos expressing GFP under control of the endothelial cell–specific promoter fli1,22 were treated with vegfa morpholinos with and without concomitant injection of vegfa165, vegfa121, or vegfeNZ2 mRNA. Knockdown by vegfa morpholinos resulted in complete loss of ISV sprouting and formation of the caudal plexus; both processes were fully rescued by injection of vegfa165 mRNA (Figure 4A; Figure 4B, quantification of embryo phenotype). Injection of vegfeNZ2 mRNA also resulted in rescue of both ISV and caudal plexus formation. Although VEGF-A165 often caused hypervascularity, the vascular pattern of VEGF-E-NZ2–expressing embryos was closer to that of wild-type embryos. In contrast, there was only partial ISV rescue with VEGF-A121 and a close to complete failure in caudal plexus formation. Subintestinal veins (SIVs) associated with the yolk sac displayed poorly organized vessels with thick diameter in the VEGF-A121–expressing zebrafish (Figure 4C), whereas vessels in VEGF-E-NZ2–treated and wild-type SIV showed similar morphology. Expression of VEGF-A165 also induced efficient rescue, often resulting in hypervascular SIV (Figure 4C; for quantification of SIV branch points, see Figure 4D). We conclude that ISV sprouting and SIV vascularization in zebrafish were induced by VEGF-A165 and VEGF-E-NZ2, but poorly if at all, by VEGF-A121.
VEGF-A121 fails to rescue ISV sprouting and caudal plexus remodeling defect in vegfa knockdown zebrafish. (A) Vegfa MO (9 ng) alone alternatively vegfa MO (9 ng) combined with vegfa mRNA encoding VEGF-A165, VEGF-A121 (100 pg each), or VEGF-E-NZ2 (200 pg, which was required to reach full effect), was injected into fli1-GFP transgenic zebrafish. At 2.5 dpf, wild-type (WT) zebrafish embryos showed axial vessels, ISV (yellow arrow), and DLAV (dorsal longitudinal anastomotic vessel). The caudal plexus in the tail appeared as a mesh-like structure (red arrow). Vegfa MO-injected zebrafish showed decreased ISV formation and lack of plexus formation. Coinjection of vegfa MO with vegfa121 mRNA resulted in partial ISV rescue, although vessels appeared thicker and stunted compared with WT. Coinjection of vegfa MO and vegfeNZ2 resulted in normal size ISV and caudal plexus, whereas injection of vegfa165 tended to result in hypervascularization. (B) Quantification of vascular defects in zebrafish lacking VEGF-A expression (vegfa MO), and after rescue by expression of VEGF-A165, VEGF-A121, or VEGF-E-NZ2. (C) Coinjection of vegfa MO and vegfa121 mRNA at 3.5 dpf showed thick, less branched vessels in the SIV (red arrow), compared with rescue by vegfa165 or vegfeNZ2. (D) Quantification of SIV branch points in the different conditions.
VEGF-A121 fails to rescue ISV sprouting and caudal plexus remodeling defect in vegfa knockdown zebrafish. (A) Vegfa MO (9 ng) alone alternatively vegfa MO (9 ng) combined with vegfa mRNA encoding VEGF-A165, VEGF-A121 (100 pg each), or VEGF-E-NZ2 (200 pg, which was required to reach full effect), was injected into fli1-GFP transgenic zebrafish. At 2.5 dpf, wild-type (WT) zebrafish embryos showed axial vessels, ISV (yellow arrow), and DLAV (dorsal longitudinal anastomotic vessel). The caudal plexus in the tail appeared as a mesh-like structure (red arrow). Vegfa MO-injected zebrafish showed decreased ISV formation and lack of plexus formation. Coinjection of vegfa MO with vegfa121 mRNA resulted in partial ISV rescue, although vessels appeared thicker and stunted compared with WT. Coinjection of vegfa MO and vegfeNZ2 resulted in normal size ISV and caudal plexus, whereas injection of vegfa165 tended to result in hypervascularization. (B) Quantification of vascular defects in zebrafish lacking VEGF-A expression (vegfa MO), and after rescue by expression of VEGF-A165, VEGF-A121, or VEGF-E-NZ2. (C) Coinjection of vegfa MO and vegfa121 mRNA at 3.5 dpf showed thick, less branched vessels in the SIV (red arrow), compared with rescue by vegfa165 or vegfeNZ2. (D) Quantification of SIV branch points in the different conditions.
Gain-of-function and loss-of-function analyses
We next examined the properties of a gain-of-function fusion protein, VEGF-A-NZ2, composed of the NRP1-binding domain from VEGF-E-NZ2, fused to the canine VEGF-A120 backbone. Moreover, a loss-of-function mutant was created by mutating R126 to E in the NRP1-binding domain in VEGF-E-NZ2 (Figure 5A).21 As shown in Figure 5A, VEGF-A-NZ2 induced tyrosine phosphorylation of VEGFR-2 in PAE/VEGFR-2, NRP1 cells to an extent similar to VEGF-A121. The loss-of-function mutant VEGF-E-R126E also induced tyrosine phosphorylation of VEGFR-2, although a higher concentration (5 nM) was required to achieve full effect. Coimmunoprecipitation of VEGFR-2 and NRP1 was efficiently induced by VEGF-A165, VEGF-E-NZ2, and VEGF-A-NZ2, but not by VEGF-A121 or by VEGF-E-R126E (Figure 5A).
Rescue of NRP1 binding and vessel branching by VEGF-A-NZ2. (A) PAE/VEGFR-2, NRP1 cells treated with different VEGF-A isoforms (Figure 5A) were subjected to immunoprecipitation (IP) of VEGFR-2, followed by immunoblotting (IB) for phosphotyrosine and NRP1 (as indicated). VEGFs were added at 2 nM; in addition, VEGF-E-R126E was added at 2 and 5 nM to saturate receptor activation. To control for loading, blotting for VEGFR-2 and NRP1 on total lysates is shown. Note that VEGF-A165, VEGF-A-NZ2, and VEGF-E-NZ2 induced efficient coprecipitation of NRP1 and VEGFR-2. The loss-of-function VEGF-E-R126E did not induce complex formation, even at the higher concentration of the factor. (B) EB cultures in 2D and 3D conditions as indicated were treated with VEGF-E-NZ2 or the loss-of-function VEGF-E-R126E. Only VEGF-E-NZ2 allowed formation of a capillary plexus in the 2D condition and sprouting angiogenesis in the 3D condition. Scale bars represent 100 μm. (C) Subcutaneous matrigel plugs containing VEGF-A121 or the gain-of-function VEGF-A-NZ2, implanted for 7 days in nude mice. Whole-mount fixation was followed by staining for expression of CD31 (red) and ASMA (green) and analysis by confocal microscopy. Microphotographs show z-stacks of 108 μm. VEGF-A-NZ2, but not VEGF-A121, showed formation of branched, pericyte-embedded vessels. Scale bar represents 50 μm. (D) Quantification of branch points in panel C by manual marking and counting of multiple matrigel plug samples (n = 5/group).
Rescue of NRP1 binding and vessel branching by VEGF-A-NZ2. (A) PAE/VEGFR-2, NRP1 cells treated with different VEGF-A isoforms (Figure 5A) were subjected to immunoprecipitation (IP) of VEGFR-2, followed by immunoblotting (IB) for phosphotyrosine and NRP1 (as indicated). VEGFs were added at 2 nM; in addition, VEGF-E-R126E was added at 2 and 5 nM to saturate receptor activation. To control for loading, blotting for VEGFR-2 and NRP1 on total lysates is shown. Note that VEGF-A165, VEGF-A-NZ2, and VEGF-E-NZ2 induced efficient coprecipitation of NRP1 and VEGFR-2. The loss-of-function VEGF-E-R126E did not induce complex formation, even at the higher concentration of the factor. (B) EB cultures in 2D and 3D conditions as indicated were treated with VEGF-E-NZ2 or the loss-of-function VEGF-E-R126E. Only VEGF-E-NZ2 allowed formation of a capillary plexus in the 2D condition and sprouting angiogenesis in the 3D condition. Scale bars represent 100 μm. (C) Subcutaneous matrigel plugs containing VEGF-A121 or the gain-of-function VEGF-A-NZ2, implanted for 7 days in nude mice. Whole-mount fixation was followed by staining for expression of CD31 (red) and ASMA (green) and analysis by confocal microscopy. Microphotographs show z-stacks of 108 μm. VEGF-A-NZ2, but not VEGF-A121, showed formation of branched, pericyte-embedded vessels. Scale bar represents 50 μm. (D) Quantification of branch points in panel C by manual marking and counting of multiple matrigel plug samples (n = 5/group).
The effect of the loss-of-function mutant VEGF-E-R126E was tested in 2D and 3D EB cultures. As shown in Figure 5B, the loss-of-function mutant failed to induce formation of the peripheral capillary plexus in the 2D EB cultures and angiogenic sprouting in the 3D cultures, respectively, whereas both these processes were invariably induced by VEGF-E-NZ2.
The effect of the gain-of-function VEGF-A-NZ2 was compared with that of the wild-type VEGF-A121 in inducing vascularization of subcutaneous matrigel plugs. As shown in Figure 5C (quantification in Figure 5D), VEGF-A-NZ2, but not VEGF-A121, induced formation of branched and pericyte-embedded vessels in the plugs. VEGF-A-NZ2 also induced sprouting in 3D EB cultures, although less efficiently than VEGF-A165.21
Differential activation of p38MAPK
To identify signal transduction pathways contributing to the different biologic activities of the VEGF ligands, signal transduction antibody arrays were performed. Filter arrays comprising 400 different signal transduction antibodies were incubated with cell lysates from PAE/VEGFR-2, NRP1 cells treated with VEGF-A165 or VEGF-A121, followed by detection using phosphotyrosine antibodies. The list of phosphorylated signaling molecules differently induced by VEGF-A165 and VEGF-A121 (Table 1) included 2 receptor-proximal substrates, p38MAPK and phospholipase C-γ (PLC-γ).
Signal transduction antibody array
| Designation . | Description . | VEGF-A165/VEGF-A121 (fold) . |
|---|---|---|
| Stat2 | Signal transducer and activator of transcription 2, 113 kDa | 9.17 |
| Stat6 | Signal transducer and activator of transcription 6, interleukin-4 induced | 5.36 |
| Ret | Ret proto-oncogene | 3.23 |
| ZO-1 | Tight junction protein 1 (zona occuludens 1) | 2.58 |
| Flt3/2 | fms-related tyrosine kinase 3/2 | 2.38 |
| TP73 | Tumor protein p73 | 2.16 |
| VAV | Vav oncogene | 2.06 |
| p38 | Mitogen activated protein kinase 14 | 1.99 |
| VEGFR-1 | fms-related tyrosine kinase 1 | 1.66 |
| SHIP | Inositol polyphosphate-5-phosphatase, 145 kDa | 1.66 |
| PLC-γ | Phospholipase C-γ | 1.60 |
| PECAM-1 | Platelet/endothelial cell adhesion molecule 1 | 1.49 |
| Stat1 | Signal transducer and activator of transcription 1, 91 kDa | 1.42 |
| c-Fgr | Gardner-Rasheed feline sarcoma viral (v-fgr) oncogene homolog | 1.36 |
| c-Cbl | Cas-Br-M (murine) ecotropic retroviral transforming sequence | 1.31 |
| Tuberin | Tuberous sclerosis 2 | 1.24 |
| P63 | Tumor protein p73-like | 1.17 |
| ERK2 | Mitogen-activated protein kinase 1 | 0.93 |
| Ets-1/2 | v-ets erythroblastosis virus E26 oncogene homolog 1/2 | 0.86 |
| HSP-70 | Heat shock 70 kDa protein | 0.81 |
| c-Jun | Jun oncogene | 0.80 |
| c-Src | v-src sarcoma (Schmidt-Ruppin A-2) viral oncogene homolog (avian) | 0.74 |
| lkB kinase-β | Inhibitor of kappa light polypeptide gene enhancer in B-cells, kinase beta | 0.74 |
| DSG | Desmoglein | 0.51 |
| Designation . | Description . | VEGF-A165/VEGF-A121 (fold) . |
|---|---|---|
| Stat2 | Signal transducer and activator of transcription 2, 113 kDa | 9.17 |
| Stat6 | Signal transducer and activator of transcription 6, interleukin-4 induced | 5.36 |
| Ret | Ret proto-oncogene | 3.23 |
| ZO-1 | Tight junction protein 1 (zona occuludens 1) | 2.58 |
| Flt3/2 | fms-related tyrosine kinase 3/2 | 2.38 |
| TP73 | Tumor protein p73 | 2.16 |
| VAV | Vav oncogene | 2.06 |
| p38 | Mitogen activated protein kinase 14 | 1.99 |
| VEGFR-1 | fms-related tyrosine kinase 1 | 1.66 |
| SHIP | Inositol polyphosphate-5-phosphatase, 145 kDa | 1.66 |
| PLC-γ | Phospholipase C-γ | 1.60 |
| PECAM-1 | Platelet/endothelial cell adhesion molecule 1 | 1.49 |
| Stat1 | Signal transducer and activator of transcription 1, 91 kDa | 1.42 |
| c-Fgr | Gardner-Rasheed feline sarcoma viral (v-fgr) oncogene homolog | 1.36 |
| c-Cbl | Cas-Br-M (murine) ecotropic retroviral transforming sequence | 1.31 |
| Tuberin | Tuberous sclerosis 2 | 1.24 |
| P63 | Tumor protein p73-like | 1.17 |
| ERK2 | Mitogen-activated protein kinase 1 | 0.93 |
| Ets-1/2 | v-ets erythroblastosis virus E26 oncogene homolog 1/2 | 0.86 |
| HSP-70 | Heat shock 70 kDa protein | 0.81 |
| c-Jun | Jun oncogene | 0.80 |
| c-Src | v-src sarcoma (Schmidt-Ruppin A-2) viral oncogene homolog (avian) | 0.74 |
| lkB kinase-β | Inhibitor of kappa light polypeptide gene enhancer in B-cells, kinase beta | 0.74 |
| DSG | Desmoglein | 0.51 |
Quantification of tyrosine phosphorylation of different signaling molecules in PAE/VEGFR-2, NRP1 cells treated with VEGF-A165 or VEGF-A121 for 5 minutes. Lysates of differently treated cells were incubated on signal transduction antibody arrays. The difference in fold induction in response to VEGF-A165 over VEGF-A121 is shown. Protein designation and description are given according to Entrez.
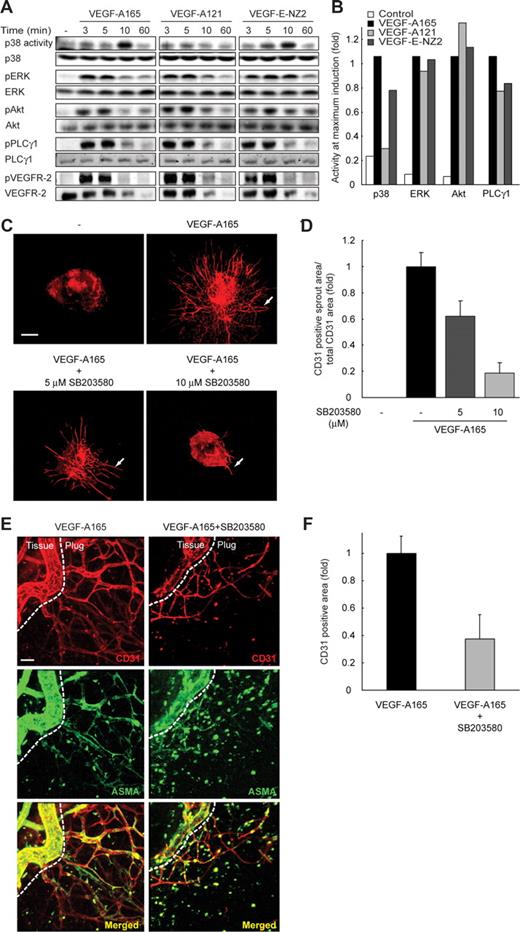
The array was followed up by analysis of p38MAPK activation in PAE/VEGFR-2, NRP1 cells treated with VEGF-A165, VEGF-A121, or VEGF-E-NZ2 (Figure 6). The NRP1-binding VEGF-A165 and VEGF-E-NZ2, but not VEGF-A121, induced a potent activation of p38MAPK at 10 minutes of treatment. PLC-γ, on the other hand, was tyrosine phosphorylated relatively equally by all 3 VEGF ligands (quantification in Figure 6B). All 3 ligands also induced VEGFR-2 tyrosine phosphorylation and activation of the Erk1 and Akt pathways equally well (Figure 6B). Activation of STAT2 and 6 (Table 1) was also examined, but we could not confirm VEGF-induced tyrosine phosphorylation of STAT molecules (data not shown).
p38MAPK induction by VEGF-A165 and VEGF-E-NZ2, but not by VEGF-A121. (A) PAE/VEGFR-2, NRP1 cells were incubated for different time periods with 2 nM of VEGF-A165, VEGF-A121, or VEGF-E-NZ2, followed by analyses, as indicated, for induction of p38MAPK, phospho (p)Erk, pAkt, pPLCγ, and pVEGFR-2 as well as unphosphorylated counterparts. An exogenous substrate (ATF-250 ) was used to measure p38MAPK activity, whereas phospho-specific antibodies were used to measure induction of Erk, Akt, PLCγ, and VEGFR-2. (B) Quantification of immunoblots shown in panel A, of induced bands at the time point of maximal induction (3, 5, or 10 minutes; see blot in panel A), in relation to relevant controls (eg, p38MAPK activity in relation to p38MAPK loading control, etc). The effect of VEGF-A165 is set to 1 for the different conditions. (C) 3D embryoid body cultures treated with VEGF-A165 in the absence and presence of 5 or 10 μM SB203580 show dose-dependent reduction in angiogenic sprouting (arrows). Scale bar represents 300 μm. (D) Quantification of CD31-sprout area in panel C. (E) Endothelial cell organization and pericyte association in subcutaneous matrigel plugs containing VEGF-A165 (left panels) or VEGF-A165 combined with 10 μM of SB203580 (right panels). Plugs were retrieved after 7 days and analyzed by whole-mount immunostaining to detect CD31 (red) and ASMA (green) followed by confocal microscopy. Microphotographs show projections of z-stacks of 90 μm. Scale bar represents 50 μm. (F) Quantification by CD31-positive area in VEGF-A165 and VEGF-A165/10 μM of SB203580-containing matrigel plugs.
p38MAPK induction by VEGF-A165 and VEGF-E-NZ2, but not by VEGF-A121. (A) PAE/VEGFR-2, NRP1 cells were incubated for different time periods with 2 nM of VEGF-A165, VEGF-A121, or VEGF-E-NZ2, followed by analyses, as indicated, for induction of p38MAPK, phospho (p)Erk, pAkt, pPLCγ, and pVEGFR-2 as well as unphosphorylated counterparts. An exogenous substrate (ATF-250 ) was used to measure p38MAPK activity, whereas phospho-specific antibodies were used to measure induction of Erk, Akt, PLCγ, and VEGFR-2. (B) Quantification of immunoblots shown in panel A, of induced bands at the time point of maximal induction (3, 5, or 10 minutes; see blot in panel A), in relation to relevant controls (eg, p38MAPK activity in relation to p38MAPK loading control, etc). The effect of VEGF-A165 is set to 1 for the different conditions. (C) 3D embryoid body cultures treated with VEGF-A165 in the absence and presence of 5 or 10 μM SB203580 show dose-dependent reduction in angiogenic sprouting (arrows). Scale bar represents 300 μm. (D) Quantification of CD31-sprout area in panel C. (E) Endothelial cell organization and pericyte association in subcutaneous matrigel plugs containing VEGF-A165 (left panels) or VEGF-A165 combined with 10 μM of SB203580 (right panels). Plugs were retrieved after 7 days and analyzed by whole-mount immunostaining to detect CD31 (red) and ASMA (green) followed by confocal microscopy. Microphotographs show projections of z-stacks of 90 μm. Scale bar represents 50 μm. (F) Quantification by CD31-positive area in VEGF-A165 and VEGF-A165/10 μM of SB203580-containing matrigel plugs.
We tested the ability of VEGF-A165 to induce p38MAPK in PAE/VEGFR-2 cells lacking NRP1 (Figure S4A). Interestingly, in the absence of NRP1, the ability of VEGF-A165 to induce p38MAPK was markedly reduced and similar to the effect of VEGF-A121. Phosphorylation at Y1212 in VEGFR-2 has been implicated in p38MAPK activation downstream of VEGFR-2.31 However, activation of p38MAPK was still induced by VEGF-A165 and VEGF-E-NZ2 but not VEGF-A121, in PAE cells expressing NRP1 combined with a mutant Y1212F VEGFR-2 (Figure S4B).
To validate the involvement of p38MAPK in sprouting angiogenesis, EBs were treated with a combination of VEGF-A165 and the specific p38MAPK inhibitor SB203580. This pyridinyl imidazole compound is a specific p38MAPK α and β isoform inhibitor; at higher concentrations, it may also inhibit phosphoinositide-dependent protein kinase 1.32 Vascular sprouting by EBs in 3D collagen gels was suppressed to 62% and 19% of that seen in the VEGF-A165–treated EBs, by SB203580-treatment at 5 and 10 μM, respectively (Figure 6C,D). These results indicate that activation of p38MAPK may be critical in formation of vascular sprouts. Treatment of cells with either SB203580 or the inert analog SB202474 did not impair VEGFR-2 tyrosine phosphorylation in the EBs (Figure S5A; quantification in Figure S5B).
Further in vivo indications for a role of p38MAPK in endothelial organization were obtained by inclusion of 10 μM of p38MAPK inhibitor in subcutaneous matrigel plugs containing VEGF-A165. This resulted in decreased vessel formation and a marked deterioration in association of ASMA-positive cells to the vessel structures (Figure 6E; quantification in Figure 6F). This pattern was reminiscent of endothelial organization in VEGF-A121–containing matrigel plugs (Figure 3E). Our data suggest that NRP1 forms a complex with VEGFR-2 in a ligand-specific manner to induce downstream signal transduction regulating activation of p38MAPK and vessel organization.
Discussion
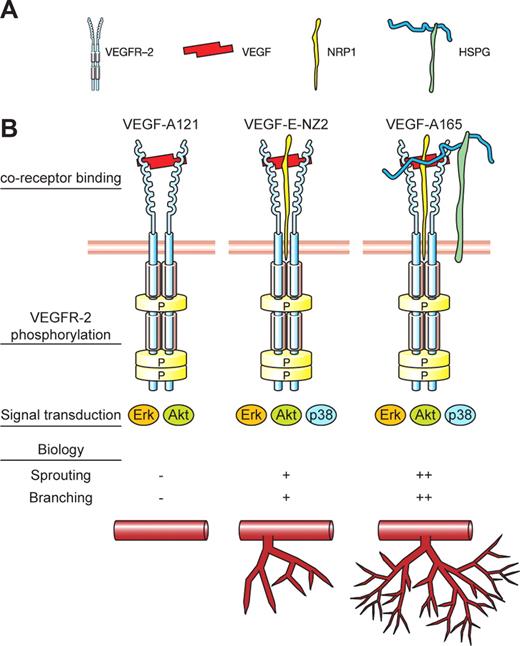
Here, we show that the responsiveness of endothelial cells to different VEGFs is guided by their ability to bind NRP1 (Figure 7, schematic summary of data). We show that VEGF-A165 and VEGF-E-NZ2 (which bound to NRP1 and induced p38MAPK activation), mediated angiogenic sprouting and endothelial cell organization in vitro and in vivo. The more efficient response by VEGF-A165 compared with VEGF-E-NZ2 in most assays may be the result of both higher affinity for binding to VEGFR-2 and binding to HS. In contrast, although VEGF-A121 activated VEGFR-2 efficiently, it did not induce a stable complex between VEGFR-2 and NRP1, and it failed to induce p38MAPK activity and a proper organization of endothelial cells into branched, pericyte-embedded vessel structures.
Schematic outline of the contribution of ligand binding to HS and NRP1 in endothelial cell responses. (A) Outline of symbols used in panel B. (B) Depiction of VEGF/VEGF receptor complexes induced by VEGF-A165, VEGF-A121, and VEGF-E-NZ2. Note that we do not exclude that HS as well as NRP1 may bind directly to VEGFR-2, but for simplicity, this is not shown. P in yellow symbols in VEGFR-2 indicates major phosphorylation sites.2 Below is shown a summary of the data in this study in terms of signal transduction (activation of Erk1/2, Akt, and p38MAPK) and biologic readout (sprouting, branching).
Schematic outline of the contribution of ligand binding to HS and NRP1 in endothelial cell responses. (A) Outline of symbols used in panel B. (B) Depiction of VEGF/VEGF receptor complexes induced by VEGF-A165, VEGF-A121, and VEGF-E-NZ2. Note that we do not exclude that HS as well as NRP1 may bind directly to VEGFR-2, but for simplicity, this is not shown. P in yellow symbols in VEGFR-2 indicates major phosphorylation sites.2 Below is shown a summary of the data in this study in terms of signal transduction (activation of Erk1/2, Akt, and p38MAPK) and biologic readout (sprouting, branching).
Mice expressing only VEGF-A120 die around or shortly after birth because of systemic vasculature insufficiency with irregular, less branched, and dilated vessels.33,34 Still, vasculogenesis proceeds in these mice and endothelial cells are able to organize into vessel structures, although to different extents in different organs. Vessels in tumors expressing VEGF-A120,35 or a matrix metalloproteinase-digested form of VEGF-A of 113 amino acid residues,36 are characterized by markedly reduced branching. However, in other models, such as in transplantation of myoblasts expressing different VEGF isoforms into the mouse hindlimb or ear, vessels of similar morphology are induced.37 All these models are long-term with complex biology, and it remains to be shown whether other angiogenic growth factors in part compensate to normalize the vasculature when only VEGF-A120/121 is expressed.
It furthermore remains to be clarified to which extent the degree of protein processing, in addition to splicing, regulates VEGF-A biology. Thus, MMP-dependent processing of different VEGF-A isoforms may result in an ultimate VEGF-A113 form with distinct biologic properties in vitro and in vivo.36 A recent report8 described certain VEGF-A121 preparations capable of binding NRP1 and to induce endothelial cell sprouting in vitro, whereas a commercial preparation, labeled as VEGF-A121, contained a VEGF-A112 form that did not bind NRP1. This is the preparation we have used in this study. We confirm that it fails to bind NRP1 and show that it potently induces VEGFR-2 activation and biologic responsiveness of in vitro cultured endothelial cells. Thus, this preparation served the purpose of providing a VEGF-A form that binds and activates VEGFR-2 without including NRP1 in the signaling complex. In addition, we have tested canine VEGF-A120. This preparation behaved in all aspects similarly to the commercial VEGF-A112 as both activated VEGFR-2 efficiently but failed to induce angiogenic sprouting in matrigel plugs (data not shown). In contrast, the gain-of-function VEGF-A-NZ2 chimeric factor, which binds NRP1 but not HS, induced formation of branched vessel structures in matrigel plugs (Figure 5C).
HS expression is a strict requirement for VEGF signaling,16 but the exact contribution remains to be clarified. Binding of growth factors to HS allows for creation of protein gradients, whereas lack of HS binding promotes free diffusion and a wider distribution. However, at least in certain in vivo models, the tissue localization of the non–HS-binding VEGF-A121 was similar to that of the longer HS-binding VEGF isoforms VEGF-A165 and 189.37 In the complete absence of cellular HS expression, VEGF fails to induce VEGFR-2 activation.38 VEGF-induced endothelial organization does not require binding of the ligand to HS, as exemplified here by the non–HS-binding ligand VEGF-E-NZ2 and the gain-of-function VEGF-A-NZ2. HS binding may contribute to the higher potency of VEGF-A165 compared with VEGF-E-NZ2 in the embryoid body sprouting, matrigel plug assays and in formation of the ISVs and SIVs in the zebrafish. Moreover, it is possible that HS binds also to VEGFR-2,38 which may be critical in stabilization of the signaling complex.
There is ample genetic evidence supporting a critical role for neuropilins in vasculogenesis and angiogenesis. NRP1−/− mice die at E10.5 to E12.5 because of defects in vascular and neural development.13 Endothelial-specific NRP1 targeting reproduces the vascular defects, enforcing an important role for NRP1 in endothelial cell function.39 Moreover, morpholino-knockout of NRP1 in zebrafish leads to loss of both ISV and SIV formation.40 In accordance, neutralization of NRP1 is additive to VEGF-A neutralization in suppressing vascular remodeling and tumor growth.14 Interestingly, vessels in tissues treated with neutralizing NRP1 antibodies showed defects in branching and deficient pericyte coating. On binding of Sema3A, neuropilins couple to plexins to regulate chemorepulsion of axons.41,42 The C-terminal 3 amino acid residues of NRP1 and NRP2, SEA, may associate with the PDZ-containing protein GIPC/synectin, which interacts with RGS-GAIP, a GTPase-activating protein for Gαi subunits.43 Whether VEGF-binding to NRP1 leads to VEGFR-2–dependent activation of this pathway has not been settled. Of note, endothelial cells expressing a fusion protein composed of the extracellular domain of the EGF receptor and the intracellular domain of NRP1 respond to EGF by enhanced migration.44
Competition between VEGF and Sema3A for partially overlapping binding sites on NRP1 has been shown to modulate VEGF-responsiveness of endothelial cells.45 We did not see a block in VEGF-A165–induced EB vascularization in the presence of a 500-fold molar excess of Sema3A (Figure S6). NRP1 may be modified by chondroitin and heparan sulfation.46 The consequence of binding of VEGF-A165 to NRP1 HS chains rather than to the NRP1 protein core is not clear. Possibly, such HS-dependent binding to NRP1 would preclude competition between VEGF-A165 and Sema3A. That semaphorin signaling through NRP1 may be dispensable in microvessel development and patterning was indicated by a recent study showing undisturbed vascular development in sema3a−/− embryos.47
NRP1 has been implicated in VEGF-induced in vitro tubulogenesis by renal epithelial cells,48 but the molecular mechanisms have not been explored. Our data show that p38MAPK may have a critical function downstream of NRP1. Gene inactivation of p38MAPKα (one of 4 family members denoted α, β, γ, δ, of which α and β are ubiquitously expressed) results in lethality at E10.5 to E11.5 because of placental defects and, dependent on the genetic background, to disturbed vascular development in embryo and yolk sac.49 Endothelial cell migration has been shown to involve p38MAPK activation in a pathway involving Nck and Fyn, downstream of Y1214 (corresponding to human Y1212) in the VEGFR-2 C-terminal tail.31 We still detected potent activation of p38MAPK in response to VEGF-A165 and VEGF-E-NZ2 treatment of PAE cells expressing a mutant Y1212F VEGFR-2 (Figure S4B). This may be the result of a direct contribution of NRP1 to p38MAPK activation. Along this line, we previously reported that vascularization of the chicken chorioallantoic membrane is disturbed in the presence of the p38MAPK inhibitor SB202190, resulting in disorganized and lumen-less vessels.50 Our present data show lack of endothelial cell organization in response to VEGF-A121, which failed to bind NRP1 and activate p38MAPK. Interestingly, neutralization with NRP1-blocking antibodies was reported to reduce the ability of VEGF-A165 to induce p38MAPK activation.14 Knowledge on how p38MAPK contributes to the 3D architecture in building of a vascular tube may lay the groundwork for future refinement of angiogenic therapy.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Ms Irja Johansson and Inger Eriksson for expert technical assistance.
This work was supported by the Swedish Cancer foundation (L.C.-W.), the Swedish Research Council (L.C.-W., L.K.), the Novo Nordisk foundation (L.C.-W.), Gustaf V:S 80-years fund (L.K.), the EC 6th framework project Lymphangiogenomics (L.C.-W.), National Institutes of Health CA373392 and CA45448 (M.K.), and the Dutch Cancer Society (L.A.v.M.).
National Institutes of Health
Authorship
Contribution: H.K., X.L., K.G., K.B.-H., L.K., M.K., and L.C.-W. designed the experiments; H.K., X.L., L.A.v.M., K.G., L.J., S.C.-S., A.S., and D.E. performed experiments; and H.K., X.L., L.A.v.M., L.K., K.B.-H., M.K., and L.C.-W. wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Lena Claesson-Welsh, Rudbeck Laboratory, Department of Genetics and Pathology, Uppsala University, Dag Hammarskjöldsv 20, 751 85 Uppsala, Sweden; e-mail: lena.claesson-welsh@genpat.uu.se.
References
Author notes
*H.K. and X.L. contributed equally to this study.

![Figure 1. VEGF-A165, VEGF-A121, and VEGF-E-NZ2 interaction with VEGFR-2, HS, and NRP1. (A) Schematic outline of VEGF ligands used in this study with VEGF-A exon structure and bindings sites for VEGFR-2, HS, and NRP1 indicated. VEGF-A165 and VEGF-A121 were purchased or produced in-house by expressing canine cDNAs in Pichia pastoris. Similar results were obtained irrespective of source. VEGF-E-NZ2, VEGF-E-R126E (loss-of-function for NRP1 binding), and VEGF-A-NZ2 (gain-of-function for NRP1 binding) were also produced in Pichia pastoris (“Methods”). (B) PAE/VEGFR-2, NRP1 cells treated with 2 nM of VEGF-A165, VEGF-A121, or VEGF-E-NZ2 for 5 minutes were characterized by immunoprecipitation (IP)/immunoblotting (IB). Tyrosine phosphorylation of immunoprecipitated VEGFR-2 was detected by immunoblotting with antiphosphotyrosine mAb 4G10. Expression of VEGFR-2 and NRP1 was shown by immunoblotting on total cell lysates. The extent of VEGFR-2/NRP1 complex formation was assessed by immunoprecipitation of VEGFR-2 followed by immunoblotting for NRP1. The basal degree of complex formation in the absence of growth factors was set to 1. (C) PAE cells transfected with human VEGFR-2 and treated with 2 nM of the 3 VEGF ligands were analyzed for VEGFR-2 tyrosine phosphorylation as in panel B. Tyrosine phosphorylation of VEGFR-2 was induced by VEGF-A165 and VEGF-A121 but only inefficiently by VEGF-E-NZ2. Bottom panel shows equal VEGFR-2 loading. (D) [35S]HS retention on nitrocellulose filter as a consequence of specific binding to VEGF-A165. [35S]HS was not retained by incubation with VEGF-A121 or VEGF-E-NZ2.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/112/9/10.1182_blood-2007-12-125856/5/m_zh80200825320001.jpeg?Expires=1764961129&Signature=BSc6mOkavKLNmZcDcaHbw57j6Mt9bi~8gGo4nRKvRiY4CO4rFZ6U-DtJM5iJ9-2Cht6yLO4W6npOWh8Es-AwykQII31DGDZ1zdX9YkXidJmxhHFhJRoT8I~lW0Pb~moYrkcEAlF1ItO~NsFMnBhSx~m1vf5DixrUWgtO1RbFtbPKBTeL~rZXQyVNBFVgAyneRkPX20ECBnPmCcxsgJ1kSYVNeDsHQT-VfShRYeF01Yhb4tc98sujNj7Q0mJyk~9WRKnUQRhZ1l1e1nJReFGV5CtAFlp~b9s-YWt846CNLmH1cpVURW4N8e68~RSw6U1BdgHzQFM7DHr0JDviWo9ThA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal