Abstract
We compared thalidomide-dexamethasone (TD) with melphalan-prednisolone (MP) in 289 elderly patients with multiple myeloma (MM). Patients received either thalidomide 200 mg plus dexamethasone 40 mg, days 1 to 4 and 15 to 18 on even cycles and days 1 to 4 on odd cycles, during a 28-day cycle or to melphalan 0.25 mg/kg and prednisolone 2 mg/kg orally on days 1 to 4 during a 28- to 42-day cycle. Patients achieving stable disease or better were randomly assigned to maintenance therapy with either thalidomide 100 mg daily and 3 MU interferon α-2b thrice weekly or to 3 MU interferon α-2b thrice weekly only. TD resulted in a higher proportion of complete and very good remissions (26% vs 13%; P = .006) and overall responses (68% vs 50%; P = .002) compared with MP. Time to progression (21.2 vs 29.1 months; P = .2), and progression-free survival was similar (16.7 vs 20.7 months; P = .1), but overall survival was significantly shorter in the TD group (41.5 vs 49.4 months; P = .024). Toxicity was higher with TD, particularly in patients older than 75 years with poor performance status. The study was registered at ClinicalTrials.gov as NCT00205751.
Introduction
Multiple myeloma is one of the most frequent hematologic cancers with an annual incidence of approximately 20 000 cases in the United States1 and 30 000 patients in Europe.2 Median survival is roughly 3.5 years with conventional therapy in usually less fit elderly patients and approximately 6.5 years in patients eligible for and treated with high-dose therapy and autologous transplantation.3 Survival rates have been constant over the past decades and have only very recently been improved.3,4 This coincided with increasing use of autologous transplantation and was seen in parallel with the introduction of thalidomide,5 but already before the approval of bortezomib and lenalidomide. Thalidomide exerts pleiotropic functions, including antiangiogenic, anti-inflammatory, and immunomodulatory activities, in vitro6 and substantial antimyeloma action in patients with previously untreated7 or relapsed or refractory disease.8 Thalidomide in combination with dexamethasone resulted in high response rates in young and also in longer progression-free survival in patients with variable age (31-86 years) but also in more toxicity than did treatment with dexamethasone only.9,10 When novel drugs are not available, melphalan and prednisone (MP) is still used as standard regimen.11 Recent studies used MP as the backbone for combination therapy with each of the new drugs.12-15
In the present investigation we evaluated the therapeutic potential and the toxicity of thalidomide-dexamethasone (TD) in comparison with MP as first-line treatment of elderly patients with multiple myeloma not eligible for high-dose therapy. In the second phase of the trial we compared thalidomide plus interferon α-2b with interferon α-2b alone as maintenance therapy; results of which will be presented after longer follow-up.
Methods
Patients
Patients with previously untreated active multiple myeloma not eligible for autologous transplantation with Durie Salmon stage II and III and, if they met the criteria of high risk, with stage I11 were enrolled between August 1, 2001, and October 31, 2007. Reasons for being not eligible for transplantation were age older than 65 years, or younger than age 65 but either with significant comorbidity, insufficient stem cells or because of patient's decision. Patients were treated in 26 centers in Austria, Czech Republic, Slovakia, Hungary, and Croatia and must have presented with adequate bone marrow (white blood cell count ≥ 3000/μL, platelets ≥ 100 000/μL) and hepatic function (SGOT, SGPT, and alkaline phosphatase < 3 times upper limit of normal), with Eastern Cooperative Oncology Group (ECOG) performance status of 3 or better and with a clear requirement for treatment, meaning that patients needed to be symptomatic from bone pain or present with anemia (hemoglobin < 10 g/dL) or both, impaired renal function (creatinine > 2.0 mg/dL), or hypercalcemia (calcium > 10.5 mg/L). Patients with extramedullary or solitary plasmacytoma without evidence of dissemination of disease or with smouldering myeloma, with more than 3 irradiation fields, congestive heart failure (New York Heart Association III and IV), acute infection, uncontrolled medical condition (eg, diabetes or glaucoma) were excluded. The study was approved by the ethical committees responsible for the participating study centers. All patients gave written informed consent before entering the study, in accordance with the Declaration of Helsinki.
Study design and procedures
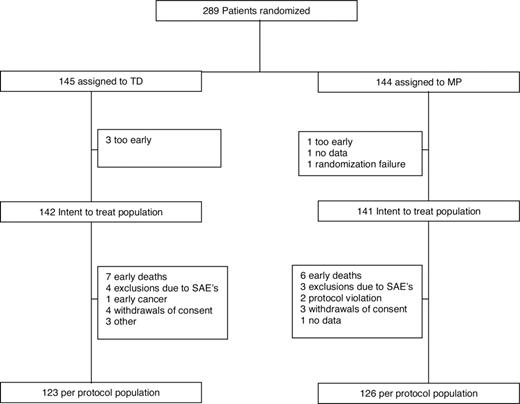
The study design comprised an induction and a maintenance phase. After registration in a centralized database, patients were randomly assigned to treatment (Figure 1). Patients were stratified according to Durie Salmon stage, type of M-component, creatinine concentration (≤ 2 mg/dL vs > 2 mg/dL) and study center, using a centralized and computerized randomization system. For induction therapy, patients received either melphalan 0.25 mg/kg and prednisolone 2 mg/kg orally on days 1 to 4 during a 28- to 42-day cycle or thalidomide 50 to 400 mg daily and dexamethasone 40 mg on days 1 to 4 and 15 to 18 on even cycles and on days 1 to 4 on odd cycles during a 28-day cycle. The duration of cycles could be extended to 6 weeks if required for resolution of toxicity. Patients were scheduled to receive a total of 9 induction cycles, but patients with very good partial remission (VGPR) or better could be stopped earlier, namely after administration of an additional 3 cycles after the ascertainment of VGPR. Investigators were encouraged to increase the dose of thalidomide up to 400 mg, if tolerated well by patients. Thalidomide was provided by Grünenthal (Aachen, Germany) for Austria, Slovakia, and Croatia, and by Lipomed (Arlesheim, Switzerland) for Czech Republic and Hungary. Patients who achieved stable disease or better underwent a second random assignment to maintenance therapy that consisted of either 100 mg thalidomide daily and 3 Mio U interferon α-2b (Schering-Plough, Kenilworth, NJ) thrice weekly or to 3 Mio U interferon α-2b thrice weekly. Patients were stratified by remission status, primary treatment, and treatment center. All patients were scheduled to receive 4 mg zoledronic acid (Novartis, Basel, Switzerland) in 4 weekly intervals continuously. After noticing an increased incidence of thromboembolic complications in the first 49 patients treated with TD, an amendment was issued making prophylaxis with low-molecular-weight heparin (LMWH) mandatory.
The primary objective was to compare progression-free survival and tolerance of both regimens, and the secondary objective was to evaluate response rates, time to response, and overall survival during both treatments. In addition, the effect of thalidomide in addition to interferon maintenance should be evaluated.
Assessments
At inclusion, baseline assessments included standard hematologic and chemistry analysis plus bone marrow biopsy and aspiration. In the induction phase, visits were planned every 4 weeks. Response assessment included measurement of serum paraprotein calculated by multiplying the proportion of monoclonal protein in the serum electrophoresis with the total protein level or in case of baseline paraprotein concentrations of less then 0.2 g/dL by immunologic techniques. In addition, 24-hour urine paraprotein excretion was determined. Immunofixation (IF) was used to identify IF-negative complete response. Radiologic investigations were performed as needed, and per protocol they were scheduled after termination of induction therapy and before enrollment into maintenance treatment. At this time a bone marrow biopsy and aspiration was repeated.
For evaluation of response, the European Group for Blood and Marrow Transplantation (EBMT) criteria16 plus an additional category of very good partial response were used. In short, a complete response required disappearance of myeloma protein in serum and urine by immunofixation maintained for a minimum of 6 weeks, less than 5% plasma cells in bone marrow, no increase in lytic bone lesions, and disappearance of soft tissue plasmacytomas. Very good partial response required a serum and urine M-component detectable by immunofixation but not on electrophoresis or a 90% or greater reduction in serum M-component plus urine M-component less than 100 mg/24 hours. A partial response needed a greater than 50% reduction in the concentration of serum monoclonal protein, or greater than 90% decrease in 24-hour urinary paraprotein reduction, or less than 200 mg maintained for a minimum of 6 weeks, greater than 50% reduction in plasma cells or soft tissue plasmacytomas or both, and no increase in lytic bone lesions. Minor response was defined as greater than 25% but less than a 50% reduction in serum paraprotein and a greater than 50% but less than a 90% reduction in 24-hour urinary paraprotein excretion, which still exceeds 200 mg/24 hours, maintained for a minimum of 6 weeks, a 25% to 49% reduction in plasma cells or soft tissue plasmacytomas or both, and no increase in lytic bone lesions. Stable disease did not meet criteria of either minimal response or progressive disease. Progressive disease required at least one of the following: a greater than 25% increase in serum paraprotein concentration with an absolute increase of at least 5 g/dL, a greater than 25% increase in 24-hour urinary paraprotein excretion with an absolute increase of more than 200 mg confirmed by at least one repeated investigation, a greater than 25% increase in plasma cells with an absolute increase of greater than 10%, progressive bone disease or increase in size or development of new soft tissue plasmacytoma, and hypercalcemia not attributable to other causes than myeloma. Best response was defined as the highest amount of disease improvement achieved by a patient at any visit from the start of therapy to the end of induction treatment.
Time to progression was calculated from the time of start of therapy to the time of progression of disease or death because of progression of myeloma, whereas progression-free survival was calculated from the time of start of therapy to the time of progressive disease or to death from any cause. Overall survival was calculated from the time of start of therapy until the date of death from any cause or the date the patient was last known to be alive.
Adverse events were assessed at each visit and graded according to the National Cancer Institute common toxicity criteria. Causes of death were recorded as attributable to myeloma, infection, cardiovascular complications, and other or unknown. Myeloma-related mortality was defined as death in patients fulfilling the criteria of progressive disease. In those patients the final cause of death could be a combination of progressive myeloma and cardiopulmonary, renal, or bone marrow failure; infection, including sepsis; or hypercalcemia. Thromboembolism was assessed by clinically objective evidence of thrombosis and by ultrasound scan and, if indicated, by pulmonary computed tomography scan.
Statistical analysis
The trial was originally designed to significantly detect a suspected superiority in progression-free survival (PFS) after 12 months of 65% versus 50% of the standard MP regimen over the innovative chemotherapy-free regimen with a power of 85% and a one-sided α-error level of 0.025, requiring a total number of 194 evaluable patients. The actually recruited number of cases is considerably higher, because more patients had been required to achieve a power of 80% for the second randomization of the trial, evaluating maintenance treatment. This resulted in an increase in power for the induction phase to approximately 95%.
Response and toxicity rates and counts were analyzed by Fisher exact, Cochran-Armitage trend, or Wilcoxon tests, as appropriate. Progression-free and overall survival, time to response, thrombotic events over time, as well as time to early death, were estimated by the product limit method.17 Univariate comparisons of these end points were performed using the log-rank test.18 The Cox proportional hazard model19 was applied for multivariate analyses of event-type data and logistic regression for early non–myeloma-related mortality. In both model types a stepwise backward model reduction after initially including all univariately significant characteristics was implemented. All P values reported are 2-sided. Except for the primary end point, all statistical tests are of exploratory nature, and no adjustments for multiplicity were applied. Subgroup analyses and analysis of thrombotic events, time to early non–myeloma-related death in the TD group, and outcome in different age groups were not prespecified prospectively.
Results
Patient characteristics
Baseline patient characteristics were well balanced between both treatment groups with the exception of a tendency for a higher proportion of patients older than 70 years and with performance status of 2 or greater in the TD group (Table 1).
Patient characteristics
| Variable . | TD . | MP . |
|---|---|---|
| No. of patients | 145 | 143* |
| Age, median (range) | 72 (54-86) | 72 (55-86) |
| 70-79 y, n %) | 87 (60) | 70 (49) |
| Older than 80 y, n (%) | 14 (10) | 16 (11) |
| Sex, f/m | 71/74 | 73/70 |
| WHO performance status ≥2, n (%) | 39 (27) | 27 (19)† |
| Stage, n (%) | ||
| I | 6 (4.1) | 5 (3.5) |
| II | 40 (27.5) | 44 (30.8) |
| III | 99 (68.3) | 94 (65.7) |
| M-component, n (%) | ||
| IgG | 91 (62.7) | 94 (65.7) |
| IgA | 33 (22.7) | 32 (22.4) |
| Light chain | 17 (11.7) | 15 (10.5) |
| IgD | 4 (2.7) | 2 (1.4) |
| Bone marrow plasma cell infiltration | ||
| n = 234 | 122 | 112 |
| Median (range) | 22 (4-90) | 25 (5-91) |
| Hemoglobin level, g/dL | ||
| n = 264 | 133 | 131 |
| Median (range) | 10.8 (6.0-15.2) | 10.8 (2.9-15.4) |
| β2-Microglobulin level, g/L | ||
| n = 245 | 122 | 123 |
| Median (range) | 4.22 (1.0-43.5) | 3.90 (1.40-41.8) |
| 3.5 g/L or less, n (%) | 50 (41) | 56 (46) |
| Greater than 3.5 g/L, n (%) | 72 (59) | 67 (54) |
| Albumin level, g/L | ||
| n = 251 | 125 | 126 |
| Median (range) | 36.9 (1.48-5.02) | 38.0 (0.95-5.37) |
| 35 g/L or less, n (%) | 55 (44) | 31 (25) |
| Greater than 35 g/L, n (%) | 70 (56) | 95 (75) |
| Creatinine level, mg/L | ||
| n = 250 | 128 | 122 |
| Median (range) | 11 (0.57-8.05) | 11 (0.62-4) |
| Calcium level, mmol/L | ||
| n = 241 | 122 | 119 |
| Median (range) | 2.31 (1.56-3.62) | 2.31 (1.76-3.41) |
| Variable . | TD . | MP . |
|---|---|---|
| No. of patients | 145 | 143* |
| Age, median (range) | 72 (54-86) | 72 (55-86) |
| 70-79 y, n %) | 87 (60) | 70 (49) |
| Older than 80 y, n (%) | 14 (10) | 16 (11) |
| Sex, f/m | 71/74 | 73/70 |
| WHO performance status ≥2, n (%) | 39 (27) | 27 (19)† |
| Stage, n (%) | ||
| I | 6 (4.1) | 5 (3.5) |
| II | 40 (27.5) | 44 (30.8) |
| III | 99 (68.3) | 94 (65.7) |
| M-component, n (%) | ||
| IgG | 91 (62.7) | 94 (65.7) |
| IgA | 33 (22.7) | 32 (22.4) |
| Light chain | 17 (11.7) | 15 (10.5) |
| IgD | 4 (2.7) | 2 (1.4) |
| Bone marrow plasma cell infiltration | ||
| n = 234 | 122 | 112 |
| Median (range) | 22 (4-90) | 25 (5-91) |
| Hemoglobin level, g/dL | ||
| n = 264 | 133 | 131 |
| Median (range) | 10.8 (6.0-15.2) | 10.8 (2.9-15.4) |
| β2-Microglobulin level, g/L | ||
| n = 245 | 122 | 123 |
| Median (range) | 4.22 (1.0-43.5) | 3.90 (1.40-41.8) |
| 3.5 g/L or less, n (%) | 50 (41) | 56 (46) |
| Greater than 3.5 g/L, n (%) | 72 (59) | 67 (54) |
| Albumin level, g/L | ||
| n = 251 | 125 | 126 |
| Median (range) | 36.9 (1.48-5.02) | 38.0 (0.95-5.37) |
| 35 g/L or less, n (%) | 55 (44) | 31 (25) |
| Greater than 35 g/L, n (%) | 70 (56) | 95 (75) |
| Creatinine level, mg/L | ||
| n = 250 | 128 | 122 |
| Median (range) | 11 (0.57-8.05) | 11 (0.62-4) |
| Calcium level, mmol/L | ||
| n = 241 | 122 | 119 |
| Median (range) | 2.31 (1.56-3.62) | 2.31 (1.76-3.41) |
WHO indicates World Health Organization.
Excludes a patient with randomization failure.
P = .123.
Response rates and time to response
Thalidomide-dexamethasone (TD) resulted in a similar rate of complete responses (2% vs 2%; P = 1.0), but a significantly higher rate of very good partial responses (24% vs 11%; P = .004), yielding a significantly higher proportion of patients with complete remission (CR) and VGPR (26% vs 13%; P = .006). Partial responses were observed in 42% of patients in the TD group and in 37% of patients in the melphalan-prednisolone (MP) group. The respective figures for minor response (MR) were 12% and 22%, respectively. Overall response rate was significantly higher during therapy with TD (68% vs 50%; P = .002). Median time to response and median time to best response were significantly shorter with TD (6 weeks [range, 1-47 weeks] vs 10 weeks [range, 2-51 weeks]; P < .001, respectively) compared with MP induction therapy (12 weeks [range, 2-51 weeks] vs 20 weeks [range, 4-74 weeks]; P < .001 and P < .001, respectively).
Time to progression and progression-free survival
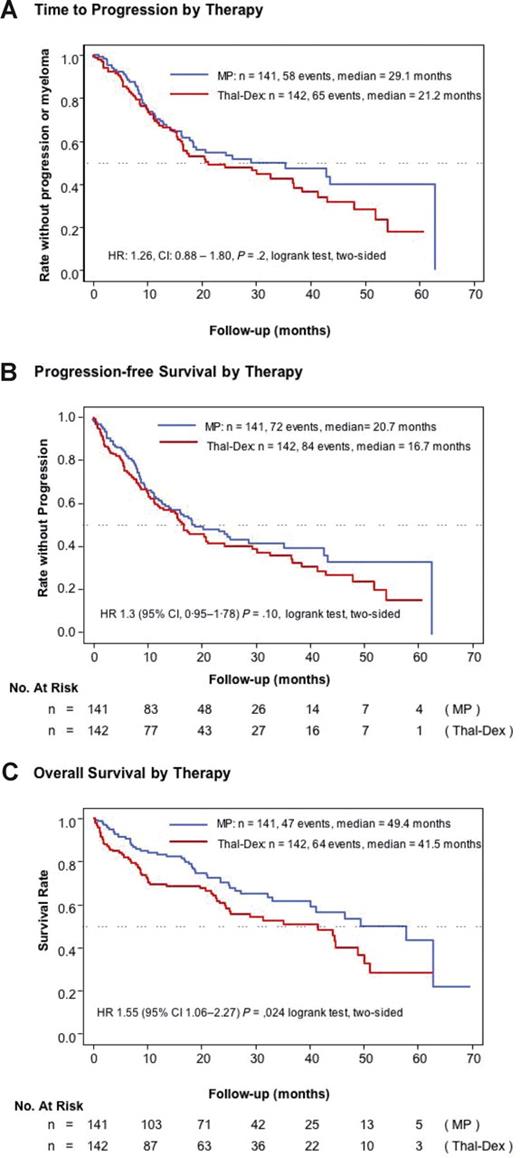
The median duration of follow-up from start of diagnosis was 28.1 months (range, 1-70 months). Progression of disease or death was noted in 84 (59.2%) patients on TD and in 72 (51.1%) patients on MP. The median time to progression (Figure 2A) was 21.2 months in the TD group and 29.1 months in the MP group (HR, 1.26; 95% confidence interval [CI], 0.88-1.80; log-rank test, P = .2). Median progression-free survival (Figure 2B) was 16.7 months and 20.7 months in the respective groups (HR, 1.30; CI, 0.95-1.78; log-rank test, P = .10). The estimated progression-free survival at 12 and 24 months, respectively, was 59% (CI, 51%-68%) and 41% (CI, 33%-51%) in patients on TD and 63% (CI, 55%-72%) and 48% months (CI, 40%-58%) in patients treated with MP.
Survival times. (A) Time to progression from entry into the trial in patients treated with thalidomide-dexamethasone or melphalan-prednisolone. (B) Progression-free survival from entry into the trial by treatment. (C) Overall survival from entry into the trial by treatment.
Survival times. (A) Time to progression from entry into the trial in patients treated with thalidomide-dexamethasone or melphalan-prednisolone. (B) Progression-free survival from entry into the trial by treatment. (C) Overall survival from entry into the trial by treatment.
Overall survival
Median overall survival was 41.5 months in patients treated with TD and 49.4 months in patients treated with MP (HR, 1.55; CI, 1.06-2.27; log-rank test, P = .024; Figure 2C). The estimated overall survival at 12 and 24 months, respectively, was 69% CI, 62%-78%) and 61% (CI, 52%-70%) in patients on TD and 83% (CI, 77%-90%) and 70% (CI, 62%-79%) in patients treated with MP.
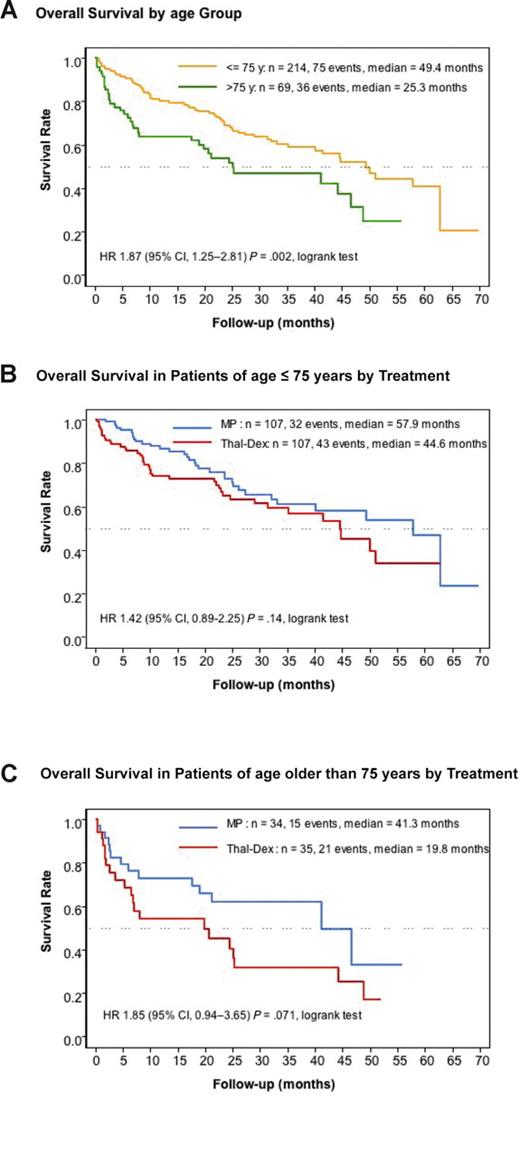
Overall survival was significantly shorter in the entire group of patients aged older than 75 years compared with younger patients aged 75 years or less (median, 25.3 vs 49.4 months; P = .002; Figure 3A). Overall survival tended to be shorter with TD in patients younger than 75 years median, 44.6 vs 57.9 months; P = .14; Figure 3B), but it was markedly (albeit not significantly) shorter in TD-treated patients older than 75 years (median, 19.8 vs 41.3 months; P = .071; Figure 3C).
Overall survival by age group. (A) Overall survival by treatment in patients of age 75 years or younger and in patients older than 75 years. (B) Overall survival in patients of age 75 years or younger by treatment. (C) Overall survival in patients older than 75 years by treatment.
Overall survival by age group. (A) Overall survival by treatment in patients of age 75 years or younger and in patients older than 75 years. (B) Overall survival in patients of age 75 years or younger by treatment. (C) Overall survival in patients older than 75 years by treatment.
Number and causes of deaths
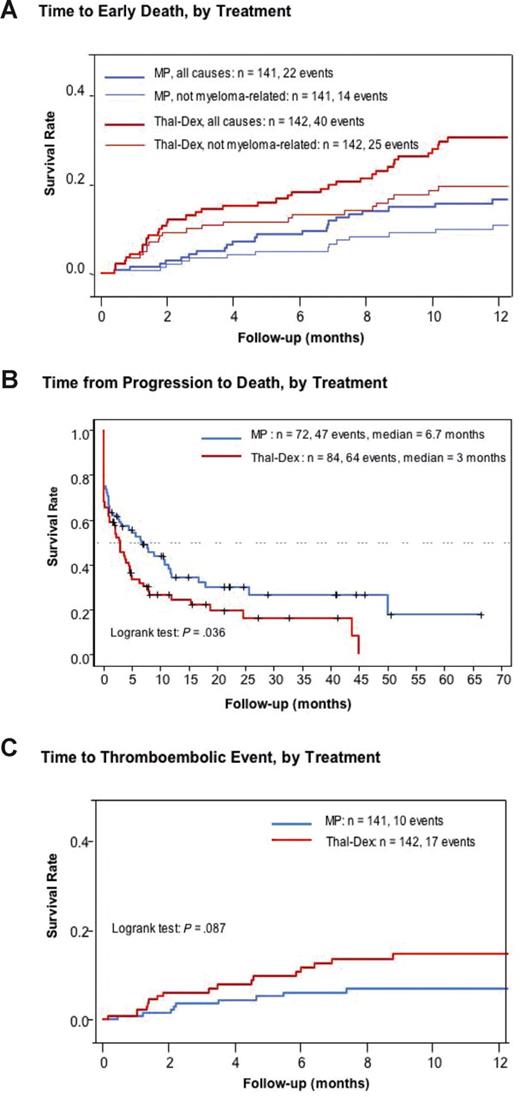
At time of analysis 111 patients had died. The number of deaths was slightly higher (64 [45%] vs 47 [33%]; P = .051) and that of early deaths within the first year was significantly higher in patients treated with TD (40 [28%] vs 22 [16%]; P = .014). Twenty-four of the early deaths observed in the TD group and 12 documented in the MP group occurred within the first 6 months (P = .048).
Twenty-five of the 40 patients in the TD arm who died within the first year died as a result of non–myeloma-related causes (infection 12, cardiovascular 9, unknown 2, second cancer 1, ileus 1). In the MP group, 14 of the 22 patients died as a result of non–myeloma-related causes infection 6, cardiovascular 4, second cancer 1, ileus 1, renal failure 1, bleeding 1). Myeloma-related mortality within the first 12 months was slightly higher but not significantly higher in patients on TD (Figure 4A). There were 75 (35%) of 214 deaths in patients younger than 75 years and 36 (52%) of 69 deaths in patients older than 75 years. Causes of death were myeloma, infection, cardiovascular, and other or unknown in 42 (19.6%), 17 (7.9%), 10 (4.8%), and 6 (2.8%) in the younger group and 21 (30.4%), 6 (8.7%), 6 (8.7%), and 3 (4.3%), respectively, in the older group. After the first 12 months of therapy mortality did not differ between patients initially randomly assigned to TD (24 [16.9%]) or to MP (25 [17.7%]; P = .876). Likewise, there was no difference in the number of deaths between patients on higher (≥ 300 mg/day) or lower doses of thalidomide within the first 2 cycles (15 [11%] vs 21 [15%]; P = .372) and during the entire duration of thalidomide induction therapy (36 [25%] vs 28 [20%]; P = .320). After progression, median time to death was significantly shorter in patients pretreated with TD compared with the MP group (median, 3 vs 6.7 months; log-rank test, P = .036; Figure 4B).
Time to early death, time from progression to death, and time to thromboembolic event. (A) Time to early death (within 12 months after entry into the trial) due to all causes or due to non–myeloma-related causes by treatment. (B) Time from progression to death by treatment. (C) Time to thromboembolic event b treatment.
Time to early death, time from progression to death, and time to thromboembolic event. (A) Time to early death (within 12 months after entry into the trial) due to all causes or due to non–myeloma-related causes by treatment. (B) Time from progression to death by treatment. (C) Time to thromboembolic event b treatment.
Predictors of early non–myeloma-related mortality in patients treated with TD and in the entire patient cohort
Univariate analysis showed low serum albumin (< 3.5 mg/dL) and poor ECOG performance status2,3 as being significantly associated with non–myeloma-related early mortality in patients treated with TD (P = .017 and P = .001, respectively). The multivariate analysis, including variables associated with a P value of at least 0.5 (age, stage, creatinine level, performance status, hemoglobin level, albumin, and center) confirmed poor performance status (odds ratio, 7.6; CI: 2.35-24.5) followed by low albumin level (odds ratio, 5.9; CI, 1.75-20.0) as independent significant predictors for early non–myeloma-related mortality. Multivariate analysis in the entire cohort of 283 patients with the use of age, performance status, and treatment arm confirmed TD as an independent predictor for shortened first-year survival (odds ratio, 1.95; CI, 1.06-3.60; P = .032). Age (odds ratio, 2.59; CI, 1.41-4.75; P = .002) and poor performance status (odds ratio, 3.02; CI, 1.65-5.56) retained their negative prognostic effect.
Number of cycles and dose of thalidomide
At time of data closure, two-thirds of the patients (TD, 65%; MP, 68%) had already received the planned 9 cycles of either therapy. Investigators were asked to start treatment with 200 mg thalidomide daily and to increase the dose if possible to 400 mg. Information was available in 136 (94%) of the 145 patients randomly assigned to TD. At cycle 2, 35% of the patients received 400 mg. The proportion of patients on this dose gradually declined to 28% at cycle 9. The mean percentage of patients with daily doses of 300, 200, 100, and 50 mg was rather constant throughout cycles 2 to 9 and amounted to 16%, 36%, 17%, and 4%, respectively. The median cumulative dose of thalidomide was 42 g (range, 1.4-162.4 g), yielding a median daily dose of 200 mg (range, 50-400 mg). Patients were on average 200 days on TD therapy. Comparison of a higher dose of thalidomide (≥ 300 mg) with a lower dose (≤ 200 mg) did not show a significant difference in response rates (P = .39), progression-free survival (P = .58), survival (P = .70), and early non–myeloma-related mortality (P = .65).
Maintenance treatment
Of the 111 patients enrolled into the maintenance phase, 54 were randomly assigned to receive thalidomide-interferon α-2b and 57 to receive interferon α-2b maintenance therapy. Median duration of maintenance therapy was 9.9 months, and median follow-up of these patients was 17.2 months. Median survival from start of maintenance treatment was 53.1 months in patients randomly assigned to receive thalidomide–interferon α-2b maintenance therapy, whereas the median has not been reached as yet in patients on interferon α-2b maintenance only (log-rank test, P = .49). When survival after start of maintenance was analyzed in relation to the induction treatment, no difference was observed (TD: median, 41.1 months; MP: median, 53.1 months; P = .41).
Toxicity
Grade 3 to 4 leukopenia and thrombopenia were more frequently reported in patients in the MP group (15% vs 3%; P < .001, and 12% vs 1%; P < .001, respectively), whereas for neuropathy, constipation, and psychological disturbances, a significant trend for greater toxicity during TD therapy was observed (P < .001, P < .001, and P < .001, respectively; Table 2).
Adverse events graded according to National Cancer Institute toxicity criteria
| Toxicity . | Patients, n (%) . | P . | |
|---|---|---|---|
| TD (n = 134) . | MP (n = 134) . | ||
| Hematologic | |||
| Anemia | 6 (4) | 15 (11) | .067 |
| Leukopenia | 4 (3) | 20 (15) | < .001 |
| Thrombopenia | 2 (1) | 16 (12) | < .001 |
| Infection | 18 (13) | 11 (8) | .237 |
| Thromboembolic | |||
| DVT | 13 (10) | 5 (4) | .085 |
| Pulmonary embolism | 4 (3) | 4 (3) | 1.0 |
| Fatigue | 15 (11) | 8 (6) | .190 |
| Neuropathy | 10 (7) | 2 (1) | < .001* |
| Neuropathy G1+2) | 87 (65) | 43 (32) | |
| Constipation | 10 (7) | 4 (3) | < .001* |
| Constipation G1+2) | 35 (26) | 13 (10) | |
| Nausea or vomiting | 8 (6) | 4 (3) | .377 |
| Renal creatinine increase) | 6 (4) | 1 (1) | .120 |
| Pulmonary | |||
| Dyspnea | 4 (3) | 2 (1) | .684 |
| Pulmonary edema | 4 (3) | 0 (0) | .122 |
| Cardiac | |||
| Cardiotoxicity | 4 (3) | 4 (3) | 1.0 |
| Hypertension | 1 (1) | 1 (1) | 1.0 |
| Edema | 1 (1) | 0 (0) | .999 |
| Skin | |||
| Exanthema or rash | 2 (1) | 2 (1) | 1.0 |
| Alopecia | 2 (1) | 0 (0) | .498 |
| Glaucoma | 2 (1) | 0 (0) | .498 |
| Psychological disturbance | 2 (1) | 1 (1) | < .001* |
| Psychological disturbance (G1+2) | 48 (36) | 24 (18) | |
| Bleeding | 1 (1) | 1 (1) | 1.0 |
| Diarrhea | 1 (1) | 1 (1) | 1.0 |
| Hyperglycemia | 1 (1) | 1 (1) | 1.0 |
| Reported grade 3 to 4 events ≥1) | 121 | 104 | |
| Toxicity . | Patients, n (%) . | P . | |
|---|---|---|---|
| TD (n = 134) . | MP (n = 134) . | ||
| Hematologic | |||
| Anemia | 6 (4) | 15 (11) | .067 |
| Leukopenia | 4 (3) | 20 (15) | < .001 |
| Thrombopenia | 2 (1) | 16 (12) | < .001 |
| Infection | 18 (13) | 11 (8) | .237 |
| Thromboembolic | |||
| DVT | 13 (10) | 5 (4) | .085 |
| Pulmonary embolism | 4 (3) | 4 (3) | 1.0 |
| Fatigue | 15 (11) | 8 (6) | .190 |
| Neuropathy | 10 (7) | 2 (1) | < .001* |
| Neuropathy G1+2) | 87 (65) | 43 (32) | |
| Constipation | 10 (7) | 4 (3) | < .001* |
| Constipation G1+2) | 35 (26) | 13 (10) | |
| Nausea or vomiting | 8 (6) | 4 (3) | .377 |
| Renal creatinine increase) | 6 (4) | 1 (1) | .120 |
| Pulmonary | |||
| Dyspnea | 4 (3) | 2 (1) | .684 |
| Pulmonary edema | 4 (3) | 0 (0) | .122 |
| Cardiac | |||
| Cardiotoxicity | 4 (3) | 4 (3) | 1.0 |
| Hypertension | 1 (1) | 1 (1) | 1.0 |
| Edema | 1 (1) | 0 (0) | .999 |
| Skin | |||
| Exanthema or rash | 2 (1) | 2 (1) | 1.0 |
| Alopecia | 2 (1) | 0 (0) | .498 |
| Glaucoma | 2 (1) | 0 (0) | .498 |
| Psychological disturbance | 2 (1) | 1 (1) | < .001* |
| Psychological disturbance (G1+2) | 48 (36) | 24 (18) | |
| Bleeding | 1 (1) | 1 (1) | 1.0 |
| Diarrhea | 1 (1) | 1 (1) | 1.0 |
| Hyperglycemia | 1 (1) | 1 (1) | 1.0 |
| Reported grade 3 to 4 events ≥1) | 121 | 104 | |
Grade 3 to 4 (unless otherwise specified) adverse events during induction therapy are assumed.
DVT indicates deep vein thrombosis.
Cochrane-Armitage trend test.
Thromboembolic events were documented in 17 patients in the TD arm and 9 cases in the MP arm (P = .15), within the first year. Thirteen patients presented with deep vein thrombosis (DVT) in the former, and in 5 patients in the latter treatment group; pulmonary embolism was seen in 4 patients of each treatment arm. Within the first 2 months after start of therapy, thromboembolic complications occurred in 8 patients of the TD group and in 3 patients of the MP group (Figure 4C). The cumulative incidence rate was 15% in the TD group and 8% in the MP group. After enrollment of 48 patients to the TD group, prophylaxis for thromboembolic complications with LMWH was recommended for the first 6 months of TD treatment in February 2004. This resulted in a 35% relative risk reduction of thromboembolic complications within the first 6 months of TD therapy from actually 12.4% to 9%.
Osteonecrosis of the jaw occurred in 2 patients (14 months and 34 months after enrollment). Both patients were on maintenance therapy with thalidomide–interferon α-2b after MP induction therapy.
Discussion
This is the first trial to compare TD with MP in elderly patients. Results in the TD group showed a significantly higher rate of very good responses (CR and VGPR) and significantly shorter time to response with no difference in time to progression (Figure 2A) and in progression-free survival (Figure 2B). Surprisingly, overall survival, however, was found to be significantly shorter with TD therapy (Figure 2C). Response rates obtained with TD in this trial were similar to response rates reported with this regimen by other groups.9,10,20,21 In those studies younger patients were enrolled, and survival data were either not reported or influenced by subsequent autologous stem cell transplantation, leaving our trial as the only one reporting survival as the main consequence of conventional therapy. The data also indicate that significant tumor reduction does not always translate into better outcome, a phenomenon observed in some other studies as well.22 This seems to be more common with the high-dose dexamethasone–containing regimen and may partly be due to a “cosmetic effect” with greater reduction in M-component concentration than in myeloma cells, as well as because of greater toxicity and significant immunosuppression by cortisone-induced apoptosis of immune cells. In accordance with these considerations, high-dose continuous corticosteroid therapy was also shown to have a detrimental effect on survival in certain nonhematologic malignancies.23
The progression-free and overall survivals observed in this study are in the range of results obtained in recent trials that compared melphalan-prednisone-thalidomide (MPT) with MP.12,13,24-26 On the basis of the poorer survival with TD particularly in the elderly patients, one may argue that thalidomide in combination with MP offers a valuable alternative to TD because it exploits the advantage of the traditional MP regimen that showed remarkable activity also in the present study. MPT avoids the significant toxicity of high-dose dexamethasone, although it may also induce considerable toxicity, particularly in patients older than 75 years,25,26 but it renders high response rates and long progression-free survival. Overall survival with MPT, however, was found to be superior to MP in only 213,24 of the 5 randomized trials presented so far.
Expectedly, in the entire cohort, overall survival was significantly shorter in patients older than 75 years (Figure 3A). TD resulted in a trend for lower survival rates compared with MP in patients 75 years or younger (Figure 3B), but it showed a marked, although not significant, tendency for shorter survival in patients older than this age, partly because of increased toxicity (Figure 3C). During the first 12 months of therapy, almost double as many patients died as a result of non–myeloma-related causes in the TD group compared with the MP arm. Multivariate analysis showed poor ECOG performance status,2,3 followed by low serum albumin level as the most important predictors of early non–myeloma-related mortality. Frequent causes of early non–myeloma-related mortality were infections in 12 and cardiovascular toxicity in 9 of the 25 patients dying as a result of other causes than myeloma during the first year. The independent prognostic effect of TD therapy for shortened survival within the first 12 months of treatment was also confirmed by multivariate analysis, including all 283 patients.
The median dose of thalidomide was 200 mg/day in individual patients with dose adaptations ranging from 50 to 400 mg/day, resulting in approximately 20% of patients receiving 100 mg or less, 36% receiving 200 mg, and the other patients being treated with 300 to 400 mg. The design of the trial that stems from 2001 required investigators to aim for a thalidomide dose of 400 mg/day, a policy that later was abandoned in clinical practice, because subsequent studies found lower doses similarly effective but better tolerated.7
Maintenance therapy with thalidomide–interferon α-2b yielded similar survival data than did treatment with interferon α-2b only. Because we used sequential randomization, half of the patients enrolled into the maintenance phase had already been pretreated with TD, which might explain the similar outcome in survival in both maintenance groups. Presently, comparisons of this part of the study are hampered by the low number of events; therefore, we plan to report on this phase of the trial after longer follow-up. Use of interferon may partly account for the rather long overall survival observed in both groups, given the high age of the patients. Previously, 2 meta-analyses have shown a survival gain of half a year with interferon maintenance therapy.27,28 Time from progression to death was relatively short with 6.7 months in patients induced with MP and only 3 months in patients initially started with TD (Figure 4B). Although we are not able to provide the exact number of patients who have received bortezomib or lenalidomide for second- or later-line therapy, only approximately 10% had access to the proteasome inhibitor and less than 5% to the newer immunomodulatory derivative of thalidomide (IMiD). Maintenance treatment with interferon was previously associated with short survival after progression,29 a phenomenon that may also have contributed to the unfavorable outcome after relapse. The significantly shorter survival after progression of disease in patients pretreated with TD (Figure 4B) is of particular interest. Analogous findings were already previously reported by Barlogie et al30 in patients who received thalidomide during up-front and the maintenance phase in conjunction with autologous transplantation. Those researchers noticed a greater than 50% reduction in postrelapse survival and a higher proportion of drug-resistant patients after thalidomide treatment. Palumbo et al31 reported similar findings in patients treated with MPT in comparison to MP. In that study, survival from relapse was less than half in the group with prior thalidomide therapy, indicating again that prolonged exposure to thalidomide may either induce a more malignant myeloma phenotype or alter the bone marrow stroma or the immune system or both in a direction favoring proliferation of myeloma cells.
The toxicities previously associated with thalidomide-based combinations7 were also observed in this trial. Neuropathy, constipation, and psychological disturbances were significantly more frequent as well as thromboembolic complications. The latter occurred primarily during the first months after the start of therapy and were only partly reduced after the introduction of prophylaxis with LMWH (Figure 4C). Severe complications resulting in non–myeloma-related mortality were probably primarily due to high-dose dexamethasone and most likely not a consequence of the high starting dose of thalidomide, because mortality did not differ between patients on higher (≥ 300 mg) and lower (≤ 200 mg) doses of thalidomide. Mortality was significantly associated with poor performance status and predominantly seen in patients older than 75 years. Our observation has significant implications for clinical practice: elderly patients with poor performance status should not be started on high-dose dexamethasone in combination with thalidomide. In those patients a less-aggressive approach with lower doses of dexamethasone and thalidomide or thalidomide in combination with melphalan-prednisone seems to be a more appropriate treatment strategy.
In conclusion, TD resulted in higher remission rates and in shorter time to response than did MP but led to higher 1-year mortality and significantly shorter overall survival.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Silvia Bakos for assistance in data collection and manuscript preparation.
This work was supported by the Austrian Forum against Cancer, by the Austrian Health authorities, the Association of Austrian Social Insurance Carriers, and partly by an investigational grant from Schering-Plough. Sample collections in the Czech Republic were supported by MSM0021622434 and LC06027.
Authorship
Contributions: H.L. designed the study, served as principal investigator, organized study group meetings, and wrote the manuscript; R.H., E.T., J.D., Z.A., B.L., M.E., I.S., H.G., R.G., and N.Z. served as investigators and contributed patient data, participated in study group meetings, and commented on the final analysis and the manuscript; I.K. provided organizational support, participated in study group meetings, and commented on the final analysis and the manuscript; and A.H. conducted the statistical analysis, participated in study group meetings, and commented on the final analysis and the manuscript. All authors had access to primary clinical trial data.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
A list of the members of the Central European Myeloma Study Group (CEMSG) who contributed by treating patients within the study and providing data appears in the Appendix (available on the Blood website; see the Supplemental Materials link at the top of the online article).
Correspondence: Heinz Ludwig, Department of Medicine I, Center of Oncology and Hematology, Wilhelminenspital, Montleartstrasse 37, A-1171, Vienna, Austria; e-mail: heinz.ludwig@wienkav.at.