To the editor:
Immune thrombocytopenic purpura (ITP) is an uncommon disorder, with an annual incidence of 2.7 adults/105 per year.1 To estimate the prevalence of ITP with a focus on patients who may require treatment, we planned to survey all hematologists in the state of Oklahoma. To determine the validity of contacting only hematologists, we assessed primary care clinicians' self-reported practices regarding referral of patients with isolated thrombocytopenia to a hematologist. Approval was obtained from the University of Oklahoma Health Sciences Center Institutional Review Board for these studies. Informed consent was obtained in accordance with the Declaration of Helsinki.
Surveys were sent to 127 primary care clinicians who participate actively in the Oklahoma Practice-Based Research Network (OKPRN), representing approximately 4% of the total primary care clinicians in Oklahoma. The survey presented 5 case vignettes, each describing a healthy 35-year-old woman who had taken no medications, had no symptoms other than the described bleeding, and who had normal blood counts except for thrombocytopenia, criteria suggesting the diagnosis of ITP.2 The scenarios ranged from mild, asymptomatic thrombocytopenia to severe thrombocytopenia with significant bleeding symptoms. Eighty-four (66%) practitioners completed the survey. Of these, 67 (80%) were MDs, 8 (9%) were DOs, 5 (6%) were nurse practitioners, and 4 (5%) were physician's assistants. Among the respondents, 43 (51%) had been in practice for 6 to 20 years, 10 (12%) for less than 6 years, and 31 (37%) for more than 20 years.
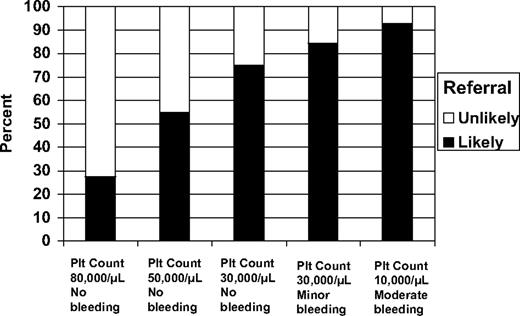
The referral pattern demonstrated by this survey (Figure 1) is similar to recommendations of the ASH ITP Practice Guideline, which recommends that patients presenting with platelet counts greater than 30 000/μL may not require treatment.2 Potential barriers to referrals were revealed. Sixteen (19%) stated that there was a not a hematologist within 50 miles of their practice, and 33 (39%) stated that there was not a hematologist they routinely called for advice and to whom they referred patients. One clinician added a comment that illustrated an additional potential barrier: “I have had difficulty identifying a ‘hematologist.’ Most ‘heme/onc’ specialists view themselves solely as ‘oncologists’ and are unhelpful for anything short of ‘cancer.’” This potential barrier to referral of patients with benign hematologic disorders deserves further study.
Clinicians' self-reported likelihood of referral to a hematologist of patients presenting with various severities of thrombocytopenia and bleeding symptoms. The bars represent responses of 84 primary care clinicians who responded to questions describing a 35-year-old woman with thrombocytopenia and either no bleeding or bruising symptoms, mild bleeding symptoms (minor bruising and prolonged menstrual periods; mild petechiae on her ankles and legs), or moderate bleeding (blood blisters in her mouth and gum bleeding). For each patient scenario, the clinicians were asked, “How likely are you to send her to a hematologist?” and given 4 possible answers from which to choose: very likely, likely, unlikely, and very unlikely. For this figure, very likely and likely were combined; unlikely and very unlikely were also combined.
Clinicians' self-reported likelihood of referral to a hematologist of patients presenting with various severities of thrombocytopenia and bleeding symptoms. The bars represent responses of 84 primary care clinicians who responded to questions describing a 35-year-old woman with thrombocytopenia and either no bleeding or bruising symptoms, mild bleeding symptoms (minor bruising and prolonged menstrual periods; mild petechiae on her ankles and legs), or moderate bleeding (blood blisters in her mouth and gum bleeding). For each patient scenario, the clinicians were asked, “How likely are you to send her to a hematologist?” and given 4 possible answers from which to choose: very likely, likely, unlikely, and very unlikely. For this figure, very likely and likely were combined; unlikely and very unlikely were also combined.
Referral patterns among physicians have been extensively studied because they affect both the quality and cost of health care.3 However, there are no previous data on referral of patients with isolated thrombocytopenia from primary care clinicians to hematologists, perhaps reflecting the low incidence of ITP.1 A 17-month study of the referral decisions of 141 family physicians documented no patients with isolated thrombocytopenia among 184 conditions seen during 34 519 office visits.4
Previous studies have validated the use of patient vignettes to measure the quality of clinical practice.5 Although some aspects of the practice of the clinicians who participated in the OKPRN survey may not be representative of all US primary care clinicians, the overall referral practices of family physicians in practice-based research networks are similar to a national sample of primary care physicians.4
This survey documents that patients who present to primary care clinicians with a new occurrence of moderate to severe thrombocytopenia are appropriately referred to a hematologist, but it also identified potential barriers to the referral of patients with benign disorders to a hematologist.
Authorship
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Deirdra R. Terrell, PhD, The University of Oklahoma Health Sciences Center, Room CHB 358, 801 NE 13th St, Oklahoma City, OK 73104; e-mail: deirdra-terrell@ouhsc.edu.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal