Abstract
In early HIV-1 infection, Vδ1 T lymphocytes are increased in peripheral blood and this is related to chemokine receptor expression, chemokine response, and recirculation. Herein we show that, at variance with healthy donors, in HIV-1–infected patients ex vivo–isolated Vδ1 T cells display cytoplasmic interferon-γ (IFN-γ). Interestingly, these cells coexpress cytoplasmic interleukin-17 (IL-17), and bear the CD27 surface marker of the memory T-cell subset. Vδ1 T cells, isolated from either patients or healthy donors, can proliferate and produce IFN-γ and IL-17 in response to Candida albicans in vitro, whereas Vδ2 T cells respond with proliferation and IFN-γ/IL-17 production to mycobacterial or phosphate antigens. These IFN-γ/IL-17 double-producer γδ T cells express the Th17 RORC and the Th1 TXB21 transcription factors and bear the CCR7 homing receptor and the CD161 molecule that are involved in γδ T-cell transendothelial migration. Moreover, Vδ1 T cells responding to C albicans express the chemokine receptors CCR4 and CCR6. This specifically equipped circulating memory γδ T-cell population might play an important role in the control of HIV-1 spreading and in the defense against opportunistic infections, possibly contributing to compensate for the impairment of CD4+ T cells.
Introduction
T lymphocytes bearing the γδ T-cell receptor represent a relevant proportion of the mucosal-associated lymphoid tissue, known to play an important role in the first-line defense against viral, bacterial, and fungal pathogens.1-3 Two main subsets of γδ T cells are known, showing distinct functional behavior4-6 : Vδ2 T lymphocytes, circulating in the peripheral blood, are involved in the response to mycobacterial infections and certain viruses, including Coxsackie virus B3 and herpes simplex virus type 2.6-10 Vδ1 T cells are resident in the mucosal-associated lymphoid tissue and are reported to participate in the immunity against Listeria monocytogenes and cytomegalovirus (CMV).11,12 Vδ2 T lymphocytes recognize nonpeptidic phosphorylated metabolites of isoprenoid biosynthesis, such as (E)-4-hydroxy-3-methyl-but-2-enyl pyrophosphate (HMBPP), isopentenyl pyrophosphate (IPP), and its isomer dimethylallyl pyrophosphate (DMAPP), expressed by mycobacteria,6,13-15 whereas Vδ1 T cells interact mainly with MHC-related antigens (MIC-A, MIC-B) and with receptors, called UL-16 binding proteins (ULBPs), for the UL-16 protein produced by CMV-infected cells.16,17
In HIV-1–infected patients, Vδ1 T lymphocytes are increased in the peripheral blood, and this is related to mucosal depletion and recirculation,18,19 whereas circulating Vδ2 T cells may decrease possibly due to reduced response to chemotactic stimuli or impaired survival.19-22 The mechanisms underlying the expansion of Vδ1 T lymphocytes in these patients remain largely unknown, although HIV-1 infection appears to have an impact on both γδ T-cell subsets, and this could have implication for disease progression.
In exerting their effector function, γδ T lymphocytes exploit different mechanisms, including MHC-independent killing of infected cells or cytokine and chemokine production.3,6 Both Vδ1 and Vδ2 T cells can produce interferon-γ in response to damage signals.23 In particular, Vδ1 T-cell clones can release IFN-γ upon challenge with MIC-A+ cells, whereas IFN-γ is produced by the Vδ2 T-cell subset upon stimulation with nonpeptide antigens.23,24 Moreover, production of TNF-α by human Vγ9/Vδ2 T cells has been demonstrated in response to bacterial products and nonpeptidic molecules.24,25
Recently, it has been reported that resident γδ T lymphocytes can produce IL-17 during Escherichia coli or Mycobacterium tuberculosis infections in mice.26,27 This is of interest as IL-17 is emerging as a cytokine crucial in the control of intracellular pathogens and fungi.28,29
In this paper we show that (1) a population of circulating Vδ1 T lymphocytes producing IFN-γ and IL-17 is expanded in vivo in HIV-1–infected patients; (2) this population is capable of proliferating and enhancing cytokine production in response to Candida albicans, whereas Vδ2 T cells respond to mycobacterial antigens; (3) IFN-γ/IL-17 double producers express the RORC and the TXB21 transcription factors, and bear the CCR7 homing receptor, the CD161 molecule involved in transendothelial migration, and the CCR4 and CCR6 chemokine receptors.
Methods
Patients
Thirty untreated HIV-1–infected patients (Pts; 16 males, 14 females) were studied at the Department of Internal Medicine, University of Genoa (Table 1). Ten healthy subjects, matched for age, were also studied as controls (Hds; 5 males, 5 females). Informed consent, approved by the institutional ethic committee, was obtained from all participants in accordance with the Declaration of Helsinki. Patients were staged according to the Centers for Disease Control (CDC, Atlanta, GA) criteria (clinical features summarized in Table 1). Serum HIV-1 RNA was quantitated using the commercial branched DNA (bDNA ultrasensitive assay; Chiron, Amsterdam, The Netherlands) with a lower limit of detection of 50 RNA copies/mL. All studies were approved by the institutional review board of the University of Genoa.
Characteristics of HIV-1–infected patients analyzed in this study
| Patient . | Sex/age, y . | HIV-1+, y* . | HIV-RNA,† copies/mL . | Stage‡ . | No. CD4,§ cells/mL . | No. CD8,§ cells/mL . | CD4/CD8 ratio . |
|---|---|---|---|---|---|---|---|
| 1 | M/54 | 2004 | 16000 | A2 | 387 | 895 | 0.4 |
| 2 | F/48 | 2003 | 57000 | A2 | 226 | 800 | 0.3 |
| 3 | F/53 | 2003 | 4200 | A1 | 616 | 648 | 1.0 |
| 4 | F/42 | 2003 | 10000 | A2 | 381 | 820 | 0.6 |
| 5 | M/30 | 2003 | 6600 | A1 | 500 | 737 | 0.7 |
| 6 | M35 | 2004 | 900 | B1 | 539 | 1081 | 0.5 |
| 7 | F/49 | 2004 | 6700 | A2 | 247 | 804 | 0.3 |
| 8 | F/23 | 2004 | 1800 | A2 | 412 | 754 | 0.5 |
| 9 | F/28 | 2004 | 24000 | A2 | 338 | 708 | 0.5 |
| 10 | M/40 | 2003 | 27000 | B1 | 539 | 2815 | 0.2 |
| 11 | M/30 | 2003 | 6300 | A1 | 911 | 915 | 1.0 |
| 12 | F/26 | 2003 | 12000 | A1 | 583 | 470 | 1.2 |
| 13 | F/29 | 2004 | < 80 | A1 | 543 | 4069 | 0.1 |
| 14 | M/37 | 2004 | 18000 | A2 | 292 | 681 | 0.4 |
| 15 | M/32 | 2003 | 1500 | A2 | 251 | 756 | 0.3 |
| 16 | M/36 | 2003 | < 80 | A2 | 314 | 709 | 0.4 |
| 17 | F/31 | 2003 | 61000 | B2 | 455 | 919 | 0.5 |
| 18 | F/31 | 2004 | 11000 | A2 | 265 | 1267 | 0.2 |
| 19 | M/31 | 2003 | 3000 | A2 | 248 | 537 | 0.5 |
| 20 | M/41 | 2004 | 35000 | A2 | 314 | 480 | 0.6 |
| 21 | M/42 | 2003 | 21000 | A1 | 640 | 1340 | 0.4 |
| 22 | F/22 | 2004 | < 80 | A1 | 694 | 878 | 0.8 |
| 23 | F/28 | 2003 | 1980 | A1 | 688 | 517 | 1.3 |
| 24 | M/32 | 2003 | 17000 | A1 | 635 | 695 | 0.9 |
| 25 | F/43 | 2003 | < 80 | A2 | 287 | 351 | 0.8 |
| 26 | M/41 | 2004 | < 80 | A2 | 266 | 1271 | 0.2 |
| 27 | M/38 | 2003 | 16000 | A2 | 509 | 1040 | 0.5 |
| 28 | F/21 | 2003 | 1100 | A2 | 446 | 400 | 1.1 |
| 29 | M/37 | 2004 | 38000 | A2 | 220 | 1009 | 0.2 |
| 30 | M/39 | 2003 | 22500 | B2 | 365 | 925 | 0.4 |
| Patient . | Sex/age, y . | HIV-1+, y* . | HIV-RNA,† copies/mL . | Stage‡ . | No. CD4,§ cells/mL . | No. CD8,§ cells/mL . | CD4/CD8 ratio . |
|---|---|---|---|---|---|---|---|
| 1 | M/54 | 2004 | 16000 | A2 | 387 | 895 | 0.4 |
| 2 | F/48 | 2003 | 57000 | A2 | 226 | 800 | 0.3 |
| 3 | F/53 | 2003 | 4200 | A1 | 616 | 648 | 1.0 |
| 4 | F/42 | 2003 | 10000 | A2 | 381 | 820 | 0.6 |
| 5 | M/30 | 2003 | 6600 | A1 | 500 | 737 | 0.7 |
| 6 | M35 | 2004 | 900 | B1 | 539 | 1081 | 0.5 |
| 7 | F/49 | 2004 | 6700 | A2 | 247 | 804 | 0.3 |
| 8 | F/23 | 2004 | 1800 | A2 | 412 | 754 | 0.5 |
| 9 | F/28 | 2004 | 24000 | A2 | 338 | 708 | 0.5 |
| 10 | M/40 | 2003 | 27000 | B1 | 539 | 2815 | 0.2 |
| 11 | M/30 | 2003 | 6300 | A1 | 911 | 915 | 1.0 |
| 12 | F/26 | 2003 | 12000 | A1 | 583 | 470 | 1.2 |
| 13 | F/29 | 2004 | < 80 | A1 | 543 | 4069 | 0.1 |
| 14 | M/37 | 2004 | 18000 | A2 | 292 | 681 | 0.4 |
| 15 | M/32 | 2003 | 1500 | A2 | 251 | 756 | 0.3 |
| 16 | M/36 | 2003 | < 80 | A2 | 314 | 709 | 0.4 |
| 17 | F/31 | 2003 | 61000 | B2 | 455 | 919 | 0.5 |
| 18 | F/31 | 2004 | 11000 | A2 | 265 | 1267 | 0.2 |
| 19 | M/31 | 2003 | 3000 | A2 | 248 | 537 | 0.5 |
| 20 | M/41 | 2004 | 35000 | A2 | 314 | 480 | 0.6 |
| 21 | M/42 | 2003 | 21000 | A1 | 640 | 1340 | 0.4 |
| 22 | F/22 | 2004 | < 80 | A1 | 694 | 878 | 0.8 |
| 23 | F/28 | 2003 | 1980 | A1 | 688 | 517 | 1.3 |
| 24 | M/32 | 2003 | 17000 | A1 | 635 | 695 | 0.9 |
| 25 | F/43 | 2003 | < 80 | A2 | 287 | 351 | 0.8 |
| 26 | M/41 | 2004 | < 80 | A2 | 266 | 1271 | 0.2 |
| 27 | M/38 | 2003 | 16000 | A2 | 509 | 1040 | 0.5 |
| 28 | F/21 | 2003 | 1100 | A2 | 446 | 400 | 1.1 |
| 29 | M/37 | 2004 | 38000 | A2 | 220 | 1009 | 0.2 |
| 30 | M/39 | 2003 | 22500 | B2 | 365 | 925 | 0.4 |
Year of diagnosis.
HIV-1 RNA was quantitated using the commercial branched DNA (bDNA Ultrasensitive Assay; Chiron) with a lower limit of detection of 50 RNA copies/mL.
Stage was defined according to the CDC criteria. Patients 1, 2, 6, 9, and 30 have a clinical history of oral candidosis. Patients showed stable disease in 2008 and were free of therapy.
CD4+ or CD8+ cells were evaluated by immunofluorescence with the specific mAbs and FACS analysis; data are expressed as absolute number of positive cells per microliter.
mAbs and reagents
The fluorescein (FITC)–conjugated anti-CD8 monoclonal antibody (mAb), the phycoerythrin (PE)–conjugated anti-CD4, the allophycocyanin-conjugated (APC) or FITC–anti-CD3 mAb, the FITC–anti-CD161, the FITC- or PE- or PE-Cy7–anti-interferon-γ (IFN-γ), the PerCP–anti-CD27 or the PerCP–anti-CCR6, the Cy5-conjugated anti-CCR7, or Cy5–anti-CCR4 monoclonal antibodies (mAbs) were from BD Pharmingen Europe (Milan, Italy). The FITC– or APC–anti–interleukin-17 (IL-17) was from Società Italiana Chimici (Rome, Italy); the anti-Vδ1 mAb A13 and the anti-Vδ2 mAb BB3 (both IgG1) were prepared as described.21 Complete medium was composed of RPMI 1640 (Biochrom, Berlin, Germany) with 10% fetal calf serum (FCS; Biochrom) supplemented with penicillin, streptomycin, and l-glutamine (Biochrom). Phorbol myristate acetate (PMA), ionomycin, brefeldin-A, carboxy-fluorescein diacetate succinimidyl ester (CFSE), and IPP (used at 5 μg/mL) were from Sigma-Aldrich (St Louis, MO) and recombinant IL-2 (rIL-2) was from PeproTech EC (London, United Kingdom). Cytomegalovirus (CMV) extract (used at 5 μg/mL) was from Microbix Biosystem (Toronto, ON), and protein-purified derivative from M tuberculosis (PPD, used at 10 μg/mL) was obtained from Statens Serum Institute (Copenhagen, Denmark). Pneumocystis carinii (PC) was prepared from homogenized lungs of immunosuppressed rats by gradient fractionation.30,31 C albicans (Ca) was grown in RPMI 1640 medium for 2 days. Both pathogens were washed twice in PBS, autoclaved, and used at 106 bodies/mL final concentration in culture (body-cell ratio: 1/1). This concentration, in preliminary titrations experiments, was optimal for peripheral blood mononuclear cell (PBMC) stimulation.30,31
Immunofluorescence and cytofluorimetric analysis
Peripheral CD4+ and CD8+ T-lymphocyte counts were performed in HIV-1–infected patients at study entry by direct immunofluorescence performed on whole blood. Parallel samples were stained with FITC and PE isotypic controls. After fixation and red cell lysis by an automated cell preparator (Coulter Q-prep; Hialeah, FL), samples were run on a FACSCanto flow cytometer and analyzed by the CellQuest computer program (Becton Dickinson, Lincoln Park, NJ). The percentage of positive cells and the absolute number (cells/μL) of CD4+ T lymphocytes were evaluated.
Immunofluorescence on cells isolated from peripheral blood or on cultured cells was performed with A13 or BB3 mAbs labeled with the fluorochrome Alexa Fluor 488 (hereafter indicated as FITC) or PE, contained in the Zenon Tricolor Labeling Kit for mouse IgG1 (Molecular Probes Europe BV, Leiden, The Netherlands),21 followed by mAbs to the indicated markers labeled with the appropriate fluorochromes. Control aliquots were stained with Alexa Fluor–labeled isotype-matched irrelevant mAbs. Samples were run on a flow cytometer (FACSCanto; Becton Dickinson) equipped with a 488-nm argon ion laser exciting FITC, Alexa Fluor 488, PE, PerCP, and PE-Cy7 and with a 633-nm He/Ne red ion laser exciting APC and Cy5. The cytofluorimeter was also equipped with appropriate filters for analysis of emission light of each fluorochrome. Data were analyzed using the CellQuest computer program and are expressed as percentage of positive cells. Calibration was assessed with CALIBRITE particles (Becton Dickinson) using the AutoCOMP computer program (United Autocomp Computer, Newport Beach, CA).
Intracytoplasmic cytokine expression in γδ T lymphocytes
Peripheral blood mononuclear cells (PBMCs) were obtained by gradient centrifugation of venous blood. Intracytoplasmic IFN-γ and IL-17 expression was evaluated in Vδ1 or Vδ2 T cells (106/mL), in the presence of BFA (10 μg/mL) to avoid cytokine secretion, upon 7 days of culture with 20 μL of antigens (IPP, PPD, CMV, PC, or Ca) at the concentration indicated in “mAbs and reagents,” on day 4, rIL-2 (30 IU/mL) was added to the wells. Maximal cytokine production was also assessed in cells activated for 4 hours with PMA (25 ng/mL) and ionomycin (1 μg/mL). To identify Vδ1 or Vδ2 T cells, cells were stained with the A13 or BB3 mAb, followed by the different mAbs anti-CD3, anti-CD27, anti-CCR7, anti-CCR4, or anti-CCR6, all labeled with the appropriate fluorochromes as indicated in “Results.” After 30 minutes at 4°C, cells were washed with PBS, NaN3 0.1%, and FCS 0.5%, fixed, and permeabilized (Becton Dickinson). After washing, samples were stained with PE- or PE-Cy7-anti–IFN-γ and FITC- or APC-anti–IL-17 mAb and analyzed by FACSCanto flow cytometer. Results are expressed as log of mean fluorescence intensity or percentage of positive cells, as indicated in the figure legend.
ELISA for IL-17 measurement
In some experiments, γδ T cells were purified from PBMCs of HIV-1–infected patients or healthy donors by immunodepletion of CD4+ and CD8+ cells using immunomagnetic beads (EasySep cell enrichment kit; StemCell Technologies, Vancouver, BC) and were more than 98% pure as assessed by immunofluorescence staining with the specific anti-γδ T-cell mAbs (not shown). Monocytes were recovered from PBMCs after 1-hour plastic adherence and used as feeder cells. Purified γδ T lymphocytes were cultured with irradiated (30 Gy) autologous monocytes in the presence of 20 μL Ca at the concentration indicated in “mAbs and reagents” and SNs were recovered on days 1, 2, 3, and 5 to measure secreted IL-17 by a commercial enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems, Milan, Italy). Plates were read on a fluorimeter at the OD450 and results expressed as nanograms per milliliter referred to a standard curve. Ex vivo isolated or cultured (after 5 days), γδ T cells were then recovered and used for detection of IL-17 by quantitative real-time–polymerase chain reaction (Q-RT-PCR).
Proliferation assay
PBMCs were stained with CFSE and seeded at 200 μL (106/mL) per well in a flat-bottomed microtiter plate containing 20 μL antigens (IPP, PPD, CMV, PC, or Ca) at the concentration indicated in “mAbs and reagents” on day 4, rIL-2 (30 IU/mL final concentration) was added to the wells. At the indicated time points, cells were harvested, stained with the PE-A13 or PE-BB3 mAbs, and analyzed by flow cytometry as described.21 Proliferating T cells were identified with the specific mAb as red cells with decreased green fluorescence intensity. Data were analyzed using the ModFit LT version 3.0 computer program (Verity Software House, Topsham, ME) and results indicated both as percentage of proliferating cells and as precursor frequency.
Quantitative real-time PCR
γδ T cells were purified from HIV-1–infected patients or healthy donors, and used immediately (ex vivo) or after culture with Ca, RNA was extracted with TriPure (Roche Diagnostics, Milan, Italy) and reverse-transcribed with random primers. Primers and probes for RORC (identification assay number Hs01076112_m1), TBX21 (identification assay number Hs00203436_m1), and IL-17 (identification assay number Hs99999082_m1) were purchased from Applied Biosystems (Foster City, CA); according to Acosta-Rodriguez et al31 Q-RT-PCR was performed on the 7900HT Fast RT-PCR system (Applied Biosystems) with the fluorescent TaqMan method.32 RORC and TBX21 mRNAs were normalized to GAPDH as a control gene and were referred to a standard curve, that is, serial dilutions of plasmids containing cloned sequences of GAPDH or 18s (Ipsogen, Marseille, France). After subtracting the threshold cycle (CT) value for GAPDH or 18s from the CT values of the target genes, the ΔCT values were converted with the formula 2−ΔΔCT to show the fold relative increase in RORC and TBX21 mRNA expression compared with levels of resting PBMCs, which were given the arbitrary value of 1.33,34
Statistical analysis
Statistical analysis was performed by the analysis of the variance (ANOVA) for repeated measures. The cutoff value of significance was .01.
Results
Vδ1 T lymphocytes producing IFN-γ are expanded in vivo in HIV-1–infected patients
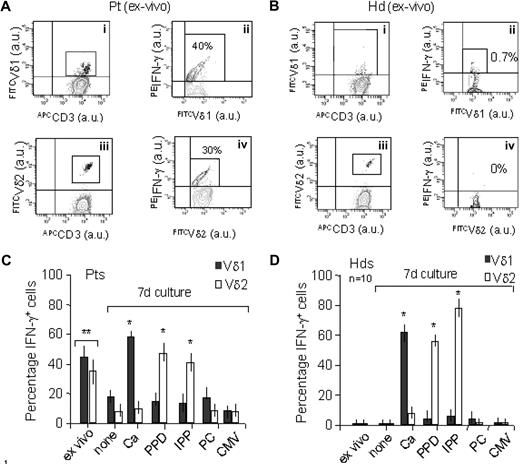
Thirty HIV-1–infected patients (Table 1), 26 at stage A and 4 at stage B of the disease, all nonprogressors, were studied. Among these patients, 5 had fewer than 80 HIV-1 RNA copies in the serum and the majority (25/30) showed a CD4/CD8 ratio lower than 1 (Table 1). In all patients, circulating Vδ1 T lymphocytes were significantly increased compared with healthy donors (9% ± 2% of T lymphocytes, 105 ± 3 cells/μL blood, in HIV-1 Pts vs 1% ± 0.5%, 13 ± 1 cells/μL blood, in Hds; one representative case in Figure 1Ai vs Bi) as we reported previously,21 whereas an increase in Vδ2 T cells was found in only 4 patients (7% ± 1% of T cells vs 4% ± 1% of Hds; one representative case in Figure 1Aiii vs Biii). Of note, in HIV-1–infected patients a fraction (ranging between 30% and 45%) of ex vivo–isolated Vδ1 (one representative case in Figure 1Aii; Figure 1C, 30 Pts) and 25% to 40% of Vδ2 T cells (one representative case in Figure 1Aiv; Figure 1C, 4 Pts) expressed cytoplasmic IFN-γ; on the other hand, no IFN-γ+ cells were found among Vδ1 or Vδ2 T cells in healthy donors (one representative case in Figure 1Bii or iv and Hds n = 10 in Figure 1D) or among ex vivo CD4+ T cells of the same patients (Figure S1, available on the Blood website; see the Supplemental Materials link at the top of the online article).
Ex vivo γδ T cells from HIV-1–infected patients express IFN-γ: response to microbial antigen stimulation. PBMCs from HIV-1–infected Pts (A: 1 representative Pt; n = 30 Vδ1 and n = 4 Vδ2 in C) or Hds (B: 1 representative Hd; n = 10 in D) were surface stained with the APC–anti-CD3 (Ai-Aiv, Bi-Biv) the FITC-conjugated A13 or BB3 mAbs to identify Vδ1 (Ai-ii, Bi-ii) or Vδ2 (Aiii-iv, Biii-iv) T cells and cytoplasmically stained with PE-anti–IFN-γ (performed immediately after isolation, Ai-Aiv and Bi-Biv, and ex vivo in C and D) or after 7 days of culture with IPP, PPD, CMV, PC, or Ca and rIL-2 was added on day 4 (C,D). (C,D) None indicates PBMCs cultured in the absence of antigens. Samples were analyzed by FACSCanto flow cytometer (Becton Dickinson). Results are expressed as mean far red (APC) fluorescence intensity (x-axis, arbitrary units, au) versus mean green (FITC) fluorescence intensity (y-axis, au; Ai, Aiii and Bi, Biii) or as mean green (FITC) fluorescence intensity (x-axis, au) versus mean red (PE) fluorescence intensity (y-axis, au; Aii, Aiv and Bii, Biv). In the top right quadrant of contour plots in Aii, Aiv, Bii, and Biv, the percentage of IFN-γ+ cells among Vδ1 or Vδ2 T cells, gated as shown in Ai, Bi or Aiii, Biii, respectively, is indicated. (C,D) Percentage of IFN-γ+ Vδ1 (■) or Vδ2 (□) on PBMC from Pts (C) or Hds (D) before and after culture with the indicated antigens; mean ± SD from 30 Pts (n = 30 Vδ1 and n = 4 Vδ2) and 10 Hds: *P < .01 versus ex vivo or versus none. (C) **P < .01 versus Hds.
Ex vivo γδ T cells from HIV-1–infected patients express IFN-γ: response to microbial antigen stimulation. PBMCs from HIV-1–infected Pts (A: 1 representative Pt; n = 30 Vδ1 and n = 4 Vδ2 in C) or Hds (B: 1 representative Hd; n = 10 in D) were surface stained with the APC–anti-CD3 (Ai-Aiv, Bi-Biv) the FITC-conjugated A13 or BB3 mAbs to identify Vδ1 (Ai-ii, Bi-ii) or Vδ2 (Aiii-iv, Biii-iv) T cells and cytoplasmically stained with PE-anti–IFN-γ (performed immediately after isolation, Ai-Aiv and Bi-Biv, and ex vivo in C and D) or after 7 days of culture with IPP, PPD, CMV, PC, or Ca and rIL-2 was added on day 4 (C,D). (C,D) None indicates PBMCs cultured in the absence of antigens. Samples were analyzed by FACSCanto flow cytometer (Becton Dickinson). Results are expressed as mean far red (APC) fluorescence intensity (x-axis, arbitrary units, au) versus mean green (FITC) fluorescence intensity (y-axis, au; Ai, Aiii and Bi, Biii) or as mean green (FITC) fluorescence intensity (x-axis, au) versus mean red (PE) fluorescence intensity (y-axis, au; Aii, Aiv and Bii, Biv). In the top right quadrant of contour plots in Aii, Aiv, Bii, and Biv, the percentage of IFN-γ+ cells among Vδ1 or Vδ2 T cells, gated as shown in Ai, Bi or Aiii, Biii, respectively, is indicated. (C,D) Percentage of IFN-γ+ Vδ1 (■) or Vδ2 (□) on PBMC from Pts (C) or Hds (D) before and after culture with the indicated antigens; mean ± SD from 30 Pts (n = 30 Vδ1 and n = 4 Vδ2) and 10 Hds: *P < .01 versus ex vivo or versus none. (C) **P < .01 versus Hds.
To address the question of whether an activating stimulus is operating in HIV-1–infected patients, we used a series of antigenic stimuli, known to activate γδ T cells or belonging to microbial agents responsible for coinfections in AIDS, to induce cytokine production by Vδ1 or Vδ2 T lymphocytes. To this aim, PBMCs from HIV-1–infected patients and Hds were challenged with IPP, PPD, CMV, PC, or Ca for 7 days, then harvested and stained for surface phenotype and cytoplasmic cytokine expression. Interestingly, in HIV-1–infected patients, where cytoplasmic IFN-γ was already detectable in ex vivo–isolated Vδ1 or Vδ2 T lymphocytes, a reduction of the percentage of producing cells was observed during culture in the absence of antigens (Figure 1C: none); both T-cell subsets reacquired the ability to produce the cytokine upon culture with Ca (60% of Vδ1-producing cells) or PPD/IPP (40% to 50% of Vδ2-producing cells; Figure 1C). In Hds most Vδ1 T lymphocytes (> 60%) produced IFN-γ in response to Ca, whereas the cytokine was found in the cytoplasm of approximately 50% of Vδ2 T cells after challenge with PPD or IPP (Figure 1D); no cytokine production was induced by PC or CMV in both cell subsets (Figure 1D). Thus, Vδ1 or Vδ2 T lymphocytes, which produce IFN-γ selectively in response to Ca or PPD/IPP, respectively, seem to be already activated in vivo in HIV-1–infected patients. No significant production of IL-4 was observed, either in Hds or in HIV-1 patients, also after challenge with antigenic stimuli (not shown).
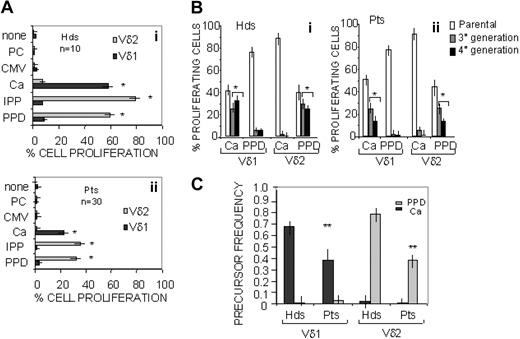
Proliferative response of Vδ1 T lymphocytes to C albicans
To define whether the IFN-γ–producing γδ T-cell population could be indeed the result of an antigen-driven expansion, a proliferation assay was performed. Thus, PBMCs obtained from either Hds or HIV-1–infected patients were stained with CFSE and cultured for 7 days in the presence of IPP, PPD, CMV, PC, or Ca, and rIL-2 starting from day 4. On day 7, cells were harvested, Vδ1 or Vδ2 T lymphocytes were identified with the specific mAbs, and the percentage of proliferating cells was evaluated as red cells with reduced green fluorescence intensity. As shown in Figure 2, a significant proliferation (> 60%) of Vδ1 T cells to Ca was found in both Hds (Figure 2Ai) and HIV-1–infected patients (Figure 2Aii), whereas Vδ2 T cells proliferated in response to PPD or IPP (Figure 2Ai for Hds and Aii for Pts). Data were confirmed by computerized analysis with the ModFit program, showing that most Vδ1 T lymphocytes (> 50%) were in third or fourth generation on day 7 when cultured in the presence of Ca, whereas the same fraction of Vδ2 T cells reached the third or fourth generation of proliferating cells when stimulated with PPD (Figure 2Bi for Hds, Bii for HIV-1 Pts). Precursor frequency calculated with ModFit computer program confirmed that Vδ1 and Vδ2 T lymphocytes proliferated selectively to Ca or PPD, respectively (Figure 2C). Taken together, these data suggest that in HIV-infected patients a Vδ1 T-cell population capable of producing IFN-γ and proliferating to Ca is expanded.
Proliferative response of Vδ1 and Vδ2 T lymphocytes to microbial antigens. PBMCs obtained from either Hds (n = 10) or HIV-1–infected patients (n = 30) were stained with CFSE and cultured for 7 days in the presence of IPP, PPD, CMV, PC, or Ca and rIL-2 was added on day 4. Vδ1 or Vδ2 T cells were identified by staining with the PE-conjugated A13 or BB3 mAbs, respectively. (A) Percentage of proliferating cells evaluated as red cells with reduced green fluorescence intensity on Vδ1 or Vδ2 gated T lymphocytes in Hds (Ai) or HIV-1–infected Pts (Aii). None indicates PBMCs cultured in the absence of antigens. Mean ± SD from 10 Hds (Ai) and 30 Pts (Aii); *P < .01 versus none. (B,C) Computerized analysis with the ModFit program, showing the percentage of Vδ1 or Vδ2 T lymphocytes in third or fourth generation (Bi: Hds; Bii: Pts) or the precursor frequency (C) on day 7 of culture with Ca or PPD. Mean ± SD from 10 Hds and 30 Pts. (B) *P < .01 versus parental population. (C) **P < .01 versus Hds.
Proliferative response of Vδ1 and Vδ2 T lymphocytes to microbial antigens. PBMCs obtained from either Hds (n = 10) or HIV-1–infected patients (n = 30) were stained with CFSE and cultured for 7 days in the presence of IPP, PPD, CMV, PC, or Ca and rIL-2 was added on day 4. Vδ1 or Vδ2 T cells were identified by staining with the PE-conjugated A13 or BB3 mAbs, respectively. (A) Percentage of proliferating cells evaluated as red cells with reduced green fluorescence intensity on Vδ1 or Vδ2 gated T lymphocytes in Hds (Ai) or HIV-1–infected Pts (Aii). None indicates PBMCs cultured in the absence of antigens. Mean ± SD from 10 Hds (Ai) and 30 Pts (Aii); *P < .01 versus none. (B,C) Computerized analysis with the ModFit program, showing the percentage of Vδ1 or Vδ2 T lymphocytes in third or fourth generation (Bi: Hds; Bii: Pts) or the precursor frequency (C) on day 7 of culture with Ca or PPD. Mean ± SD from 10 Hds and 30 Pts. (B) *P < .01 versus parental population. (C) **P < .01 versus Hds.
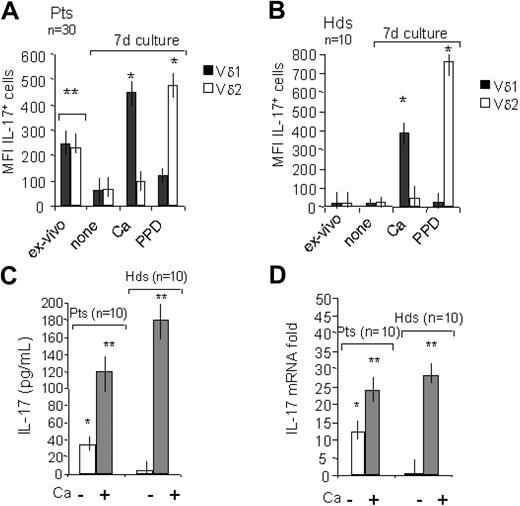
γδ T lymphocytes producing IFN-γ are also IL-17–producing cells
As IL-17 is emerging as a cytokine crucial in the control of intracellular pathogens and fungi,28,29 we analyzed the production of these cytokine in ex vivo γδ T cells in HIV-1–infected patients and in vitro in response to the different microbial antigens. Of note, more than one-third of Vδ1 and approximately half of Vδ2 T cells isolated ex vivo from HIV-1–infected patients were positive for cytoplasmic expression of IL-17, at variance with healthy donors (Figure 3A, Pts n = 30 and Figure 3B, Hds n = 10) and with ex vivo CD4+ T cells of the same patients (Figure S1). Production of IL-17 by γδ T cells from HIV-1–infected patients decreased when cultured in the absence of antigens (none in Figure 3A), but became able to produce the cytokine upon challenge with Ca for Vδ1 or PPD for Vδ2 T lymphocytes (Figure 3A). As shown in Figure 3B, Vδ1 T lymphocytes from Hds could produce IL-17 upon culture with Ca, whereas Vδ2 T cells became positive for the cytokine when stimulated with PPD. These data were supported by the finding that IL-17 was detectable in SNs from γδ T lymphocytes cultured in the presence of Ca; of note, γδ T cells from HIV-1 Pts could release IL-17 also before Ca stimulation (Figure 3C). Likewise, purified γδ T lymphocytes, obtained from either HIV-1 Pts or Hds and cultured with Ca, expressed IL-17 mRNA (Figure 3D); again, IL-17 transcript was already expressed in ex vivo γδ T cells from HIV-1 Pts (Figure 3D).
IL-17 expression in ex vivo γδ T cells from HIV-1–infected patients and response to microbial antigens. PBMCs from HIV-1–infected Pts (A: n = 30) or Hds (B: n = 10) were surface stained with the FITC–anti-CD3 and PE-conjugated A13 or BB3 mAbs to identify Vδ1 or Vδ2 T cells and cytoplasmically stained with APC-anti–IL-17 mAb, immediately ex vivo or after 7 days of culture with Ca or PPD, and rIL-2 was added on day 4. Samples were analyzed by flow cytometry and gated on Vδ1 or Vδ2 T cells, and results were expressed as mean far red (IL-17) fluorescence intensity (MFI; arbitrary units, au) of IL-17+ cells among Vδ1 (■) or Vδ2 (□) T cells (A: mean ± SD from 30 Pts; B: mean ± SD from 10 Hds). None indicates PBMCs cultured in the absence of antigens. *P < .01 versus ex vivo or versus none. (A) **P < .01 versus Hds in panel B. (C,D) γδ T cells purified from HIV-1–infected patients (n = 10) or healthy donors (n = 10) by immunodepletion of CD4+ and CD8+ cells were cultured with irradiated (30 Gy) autologous monocytes in the presence of Ca, and SNs were recovered on day 4 and secreted IL-17 was measured by ELISA (C). Plates were read on a fluorimeter at the OD450 and results expressed as picogram per milliliter referred to a standard curve. (−) indicates γδ T cells cultured in the absence of antigen. *P < .01 versus Hds. **P < .01 versus ex vivo or versus (−). (D) RNA from ex vivo–isolated or –cultured (d4) purified γδ T cells was reverse transcribed and amplified by Q-RT-PCR with specific primers for IL-17, compared with 18s. (−) indicates cells cultured in the absence of antigen. Results are expressed as fold increase of IL-17 mRNA versus 18s and are the mean ± SD from 10 Pts or 10 Hds. *P < .01 versus Hds. **P < .01 versus (−).
IL-17 expression in ex vivo γδ T cells from HIV-1–infected patients and response to microbial antigens. PBMCs from HIV-1–infected Pts (A: n = 30) or Hds (B: n = 10) were surface stained with the FITC–anti-CD3 and PE-conjugated A13 or BB3 mAbs to identify Vδ1 or Vδ2 T cells and cytoplasmically stained with APC-anti–IL-17 mAb, immediately ex vivo or after 7 days of culture with Ca or PPD, and rIL-2 was added on day 4. Samples were analyzed by flow cytometry and gated on Vδ1 or Vδ2 T cells, and results were expressed as mean far red (IL-17) fluorescence intensity (MFI; arbitrary units, au) of IL-17+ cells among Vδ1 (■) or Vδ2 (□) T cells (A: mean ± SD from 30 Pts; B: mean ± SD from 10 Hds). None indicates PBMCs cultured in the absence of antigens. *P < .01 versus ex vivo or versus none. (A) **P < .01 versus Hds in panel B. (C,D) γδ T cells purified from HIV-1–infected patients (n = 10) or healthy donors (n = 10) by immunodepletion of CD4+ and CD8+ cells were cultured with irradiated (30 Gy) autologous monocytes in the presence of Ca, and SNs were recovered on day 4 and secreted IL-17 was measured by ELISA (C). Plates were read on a fluorimeter at the OD450 and results expressed as picogram per milliliter referred to a standard curve. (−) indicates γδ T cells cultured in the absence of antigen. *P < .01 versus Hds. **P < .01 versus ex vivo or versus (−). (D) RNA from ex vivo–isolated or –cultured (d4) purified γδ T cells was reverse transcribed and amplified by Q-RT-PCR with specific primers for IL-17, compared with 18s. (−) indicates cells cultured in the absence of antigen. Results are expressed as fold increase of IL-17 mRNA versus 18s and are the mean ± SD from 10 Pts or 10 Hds. *P < .01 versus Hds. **P < .01 versus (−).
Interestingly, we found that ex vivo–isolated Vδ1 or Vδ2 T lymphocytes from HIV-1–infected patients coexpress cytoplasmic IFNγ and IL-17 (Figure 4Ai,C for Vδ1; Figure 4Bi,D for Vδ2). A similar population of γδ T cells coproducing the 2 cytokines was obtained from Hds upon culture with Ca for Vδ1 T lymphocytes or PPD for Vδ2 T lymphocytes (Figure 4C,D, respectively); in HIV-1–infected patients, the in vitro culture with these antigens led to the expansion of the IL-17/IFN-γ–producing Vδ1 or Vδ2 T cells (Figure 4Aii,Bii and 4C,D). Figure S2 shows that ex vivo–isolated Vδ1 and Vδ2 T cells from Hds, in the absence of antigens, need PMA plus ionomycin stimulation to produce IFN-γ (Figure S2A), stimuli that are not sufficient for IL-17 production (Figure S2B); on the other hand, in HIV-1–infected patients ex vivo–isolated Vδ1 and Vδ2 T cells constitutively express both IFN-γ (Figure S2A) and IL-17 (Figure S2B). These results would confirm that among γδ T cells the Vδ1 subset preferentially respond to Ca producing both IL-17 and IFN-γ and support that this population is expanded in vivo in HIV-1–infected patients.
γδ T lymphocytes producing IFN-γ are also IL-17–producing cells. PBMCs from HIV-1–infected Pts (A,B: 1 representative Pt; C: n = 20 for Pts with increased Vδ1 T cells; D: n = 4 for Pts with increased Vδ2 T cells) or Hds (n = 10, C,D) were surface stained with the FITC–anti-CD3 and PE-conjugated A13 (A) or BB3 (B) mAbs (to identify Vδ1 or Vδ2 T cells, respectively) and cytoplasmically stained with APC-anti–IL-17 and PE-Cy7-anti–IFN-γ (performed immediately after isolation [Ai,Bi] and ex vivo [C,D]) or after 7 days of culture with Ca or PPD, and rIL-2 was added on day 4 (Aii,Bii,C,D). Samples were analyzed by FACSCanto flow cytometer (Becton Dickinson) gating on CD3/Vδ1 (Ai-Aii, C) or CD3/Vδ2 (Bi-ii, D) T cells. Results are expressed as mean far red (APC) fluorescence intensity (x-axis, au) versus mean very far red (PE-Cy7) fluorescence intensity (y-axis, au; Ai-ii, Bi-ii). The percentages depicted in the top right quadrants of contour plots in panels A and B indicate IFN-γ+IL-17+ cells among Vδ1 T cells ex vivo (Ai) or after culture with C albicans (Ca; Aii) or among Vδ2 T cells ex vivo (Bi) or after culture with PPD (Bii). (C-D) IFN-γ+IL-17+ cells gated on CD3/Vδ1 (C) or CD3/Vδ2 (D) T cells, before and after culture with Ca or PPD (mean ± SD from 10 Hds and mean ± SD from 20 in C or 4 Pts in D). *P < .01 versus Hds. **P < .01 versus ex vivo.
γδ T lymphocytes producing IFN-γ are also IL-17–producing cells. PBMCs from HIV-1–infected Pts (A,B: 1 representative Pt; C: n = 20 for Pts with increased Vδ1 T cells; D: n = 4 for Pts with increased Vδ2 T cells) or Hds (n = 10, C,D) were surface stained with the FITC–anti-CD3 and PE-conjugated A13 (A) or BB3 (B) mAbs (to identify Vδ1 or Vδ2 T cells, respectively) and cytoplasmically stained with APC-anti–IL-17 and PE-Cy7-anti–IFN-γ (performed immediately after isolation [Ai,Bi] and ex vivo [C,D]) or after 7 days of culture with Ca or PPD, and rIL-2 was added on day 4 (Aii,Bii,C,D). Samples were analyzed by FACSCanto flow cytometer (Becton Dickinson) gating on CD3/Vδ1 (Ai-Aii, C) or CD3/Vδ2 (Bi-ii, D) T cells. Results are expressed as mean far red (APC) fluorescence intensity (x-axis, au) versus mean very far red (PE-Cy7) fluorescence intensity (y-axis, au; Ai-ii, Bi-ii). The percentages depicted in the top right quadrants of contour plots in panels A and B indicate IFN-γ+IL-17+ cells among Vδ1 T cells ex vivo (Ai) or after culture with C albicans (Ca; Aii) or among Vδ2 T cells ex vivo (Bi) or after culture with PPD (Bii). (C-D) IFN-γ+IL-17+ cells gated on CD3/Vδ1 (C) or CD3/Vδ2 (D) T cells, before and after culture with Ca or PPD (mean ± SD from 10 Hds and mean ± SD from 20 in C or 4 Pts in D). *P < .01 versus Hds. **P < .01 versus ex vivo.
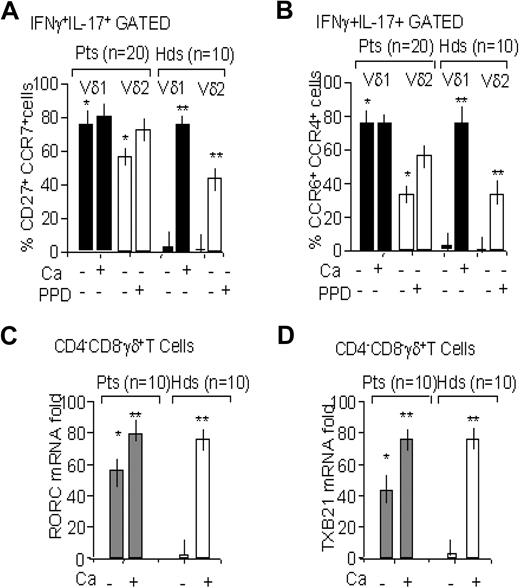
γδ T lymphocytes producing IFN-γ and IL-17 have a memory phenotype and are CD161+
It has been reported that IL-17–producing T helper (Th) cells, besides expressing CD27 as a marker of memory T cells, also bear CCR4 and CCR6, which identify memory CD4+ T cells specific for C albicans.32,35 Thus, we analyzed the expression of these markers on IL-17/IFN-γ–producing γδ T lymphocytes from HIV-1 patients before and after stimulation with the various microbial antigens, compared with healthy donors. Of note, fluorescence-activated cell sorting (FACS) analysis performed gating on γδ T lymphocytes coproducing the 2 cytokines showed that this cell population coexpresses CD27 and CCR7 (Figure 5A), thus belonging to the so-called central memory T-cell subset.32,35 More importantly, γδ T lymphocytes producing IL-17/IFN-γ in response to fungal or mycobacterial antigens coexpressed the chemokine receptors CCR6 and CCR4 (Figure 5B). The double-producer γδ T lymphocytes, obtained from either HIV-1 Pts or Hds upon culture with Ca, expressed RORC (variant 2; Figure 5C), the human ortholog of the mouse RORγt transcription factor that is required for IL-17 production,32 and the Th1 transcription factor TXB2132 (Figure 5D). Interestingly both transcripts were already expressed in ex vivo γδ T cells from HIV-1 Pts (Figure 5C,D).
γδ T lymphocytes producing IFN-γ and IL-17 have a memory phenotype. PBMCs from HIV-1–infected Pts (n = 20) or Hds (n = 10) were stained with PE-conjugated A13 or BB3 mAbs to identify Vδ1 (■) or Vδ2 (□) T cells, respectively, PerCP-conjugated anti-CD27 and Cy5-conjugated anti-CCR7 (A), or PerCP-conjugated anti-CCR6 and Cy5-conjugated anti-CCR4 (B). Then cells were fixed and permeabilized, and cytoplasmically stained with FITC-anti–IL-17 and PE-Cy7-anti–IFN-γ mAbs was performed on cells before or after 7 days of culture with Ca or PPD and rIL-2 was added on day 4. Samples were analyzed by FACSCanto flow cytometer (Becton Dickinson) gated on IFN-γ+IL-17+ Vδ1 or Vδ2 T cells. Results are expressed as percentage of double-positive cells; mean ± SD from 20 Pts or 10 Hds. *P < .01 versus Hds. **P < .01 versus cells cultured in the absence of antigens (−). (C-D) Total RNA from purified γδ T cells, HIV-1–infected Pts (n = 10), or Hds (n = 10) before and after 7 days of culture in the presence of Ca, as indicated, was reverse transcribed and amplified by Q-RT-PCR with specific primers for RORC (C) or TBX21 (D), compared with GAPDH. Results are expressed as fold increase of RORC or TBX21 mRNA versus GAPDH and are the mean ± SD from 10 Pts or 10 Hds. *P < .001 versus Hds. **P < .001 versus (−).
γδ T lymphocytes producing IFN-γ and IL-17 have a memory phenotype. PBMCs from HIV-1–infected Pts (n = 20) or Hds (n = 10) were stained with PE-conjugated A13 or BB3 mAbs to identify Vδ1 (■) or Vδ2 (□) T cells, respectively, PerCP-conjugated anti-CD27 and Cy5-conjugated anti-CCR7 (A), or PerCP-conjugated anti-CCR6 and Cy5-conjugated anti-CCR4 (B). Then cells were fixed and permeabilized, and cytoplasmically stained with FITC-anti–IL-17 and PE-Cy7-anti–IFN-γ mAbs was performed on cells before or after 7 days of culture with Ca or PPD and rIL-2 was added on day 4. Samples were analyzed by FACSCanto flow cytometer (Becton Dickinson) gated on IFN-γ+IL-17+ Vδ1 or Vδ2 T cells. Results are expressed as percentage of double-positive cells; mean ± SD from 20 Pts or 10 Hds. *P < .01 versus Hds. **P < .01 versus cells cultured in the absence of antigens (−). (C-D) Total RNA from purified γδ T cells, HIV-1–infected Pts (n = 10), or Hds (n = 10) before and after 7 days of culture in the presence of Ca, as indicated, was reverse transcribed and amplified by Q-RT-PCR with specific primers for RORC (C) or TBX21 (D), compared with GAPDH. Results are expressed as fold increase of RORC or TBX21 mRNA versus GAPDH and are the mean ± SD from 10 Pts or 10 Hds. *P < .001 versus Hds. **P < .001 versus (−).
Finally, we analyzed whether this cell population did express the CD161 molecule, also known as NKRP1A, previously reported to define a subset of CD4+ cells able to recirculate36 and recently shown to identify IL-17–producing cells.37-39 We found that in HIV-1 patients, approximately half of the Vδ1 T-cell population coexpresses the CD161 molecule (Figure 6A,Bi), at variance with Hds where Vδ1 T cells are mostly CD161− (Figure 6A); Vδ2 T cells are CD161+ in both HIV-1 patients and Hds (Figure 6A). We have reported that Vδ2 T lymphocytes use NKRP1A/CD161 to transmigrate across endothelial cells.40,41 Among the Vδ1 T-cell population, IL-17/IFN-γ–producing cells were confined in the CD161+ subset (Figure 6Bi,ii vs Bi,iii and 6C); of note, in Hds, this population was evident only upon culture with Ca (Figure 6D). In most HIV-1 Pts, the Vδ1 CD161+ cell population was expanded after culture with Ca (Figure 6C). Among Vδ2 T cells this analysis was not possible as they all express CD161.
γδ T lymphocytes producing IFN-γ and IL-17 express CD161. PBMCs from HIV-1–infected Pts (n = 20) or Hds (n = 10) were stained with the PE-conjugated A13 or BB3 mAbs to identify Vδ1 or Vδ2 T cells, respectively, PerCP-conjugated anti-CD3, and FITC-conjugated anti-CD161 (A-D). Then cells were fixed and permeabilized and cytoplasmically stained with APC-anti–IL-17 and PE-Cy7-anti–IFN-γ was performed on cells before or after 7 days of culture with Ca or PPD and rIL-2 was added on day 4 (B,C: Pts; D: Hds). Samples were analyzed by FACSCanto flow cytometer (Becton Dickinson) gated on CD3/Vδ1 or CD3/Vδ2 cells (A) and on CD161+ or CD161− Vδ1 T cells (C,D). (A) Percentage of CD161+ cells on CD3/Vδ1 or CD3/Vδ2 gated cells as indicated. (B) One representative case of 10 analyzed: PE-Cy7–IFN-γ/APC–IL-17 staining of CD161+ (Bii) or CD161− (Biii) gated cells among Vδ1 T cells (Bi, indicated by []). Results are expressed as log red fluorescence intensity (x-axis, au) versus log green fluorescence intensity (y-axis, au; Bi) or as log far red fluorescence intensity (x-axis, au) versus log very far red fluorescence intensity (y-axis, au; Bii,iii). In panels C-D, results are expressed as percentage of IFN-γ+IL-17+ cells among CD161+Vδ1 or CD161−Vδ1 T cells and are the mean ± SD from 20 Pts (C) or 10 Hds (D). *P < .01 versus cells cultured in the absence of antigens (−). **P < .01 versus Hds.
γδ T lymphocytes producing IFN-γ and IL-17 express CD161. PBMCs from HIV-1–infected Pts (n = 20) or Hds (n = 10) were stained with the PE-conjugated A13 or BB3 mAbs to identify Vδ1 or Vδ2 T cells, respectively, PerCP-conjugated anti-CD3, and FITC-conjugated anti-CD161 (A-D). Then cells were fixed and permeabilized and cytoplasmically stained with APC-anti–IL-17 and PE-Cy7-anti–IFN-γ was performed on cells before or after 7 days of culture with Ca or PPD and rIL-2 was added on day 4 (B,C: Pts; D: Hds). Samples were analyzed by FACSCanto flow cytometer (Becton Dickinson) gated on CD3/Vδ1 or CD3/Vδ2 cells (A) and on CD161+ or CD161− Vδ1 T cells (C,D). (A) Percentage of CD161+ cells on CD3/Vδ1 or CD3/Vδ2 gated cells as indicated. (B) One representative case of 10 analyzed: PE-Cy7–IFN-γ/APC–IL-17 staining of CD161+ (Bii) or CD161− (Biii) gated cells among Vδ1 T cells (Bi, indicated by []). Results are expressed as log red fluorescence intensity (x-axis, au) versus log green fluorescence intensity (y-axis, au; Bi) or as log far red fluorescence intensity (x-axis, au) versus log very far red fluorescence intensity (y-axis, au; Bii,iii). In panels C-D, results are expressed as percentage of IFN-γ+IL-17+ cells among CD161+Vδ1 or CD161−Vδ1 T cells and are the mean ± SD from 20 Pts (C) or 10 Hds (D). *P < .01 versus cells cultured in the absence of antigens (−). **P < .01 versus Hds.
Discussion
Expansion of circulating Vδ1 T lymphocytes has been reported both in early and in nonprogressor HIV-1–infected patients.21,22 In this paper, we show that (1) in HIV-1–infected patients circulating Vδ1 T lymphocytes not only are increased but are already activated in vivo, as they express cytoplasmic IFN-γ and IL-17; (2) the Vδ1 T-cell subset is able to selectively proliferate and produce IFN-γ and IL-17 in response to C albicans in vitro; and (3) IFN-γ/IL-17–producing cells display a memory phenotype, express the Th17 RORC and the Th1 TXB21 transcription factors, bear the CCR4 and CCR6 chemokine receptors, and are CD161+.
Antimicrobial immune response is based on antigen-induced triggering and expansion of naive CD4+ T lymphocytes that differentiate into memory T cells of the Th1 or Th2 type, producing IFN-γ or IL-4, respectively.42 In particular, activation of the Th1 subset is crucial in the defense against viruses and intracellular pathogens.43 This process depends on the availability of an intact CD4 T-helper subset, which in turn is highly impaired in HIV-1 patients, thus leading not only to a defective control of viral infection but also to an increased susceptibility to fungi and intracellular pathogen invasion. From this viewpoint, it is of interest that in HIV-1–infected patients with stable disease (all the patients analyzed in this study) we found several circulating Vδ1 T lymphocytes significantly increased, compared with healthy donors, and already activated in vivo as they contain in the cytoplasm IFN-γ and IL-17. Notably, IL-17 has an important role in the control of fungal infections, by recruiting neutrophils and macrophages to infected tissues.44 Interestingly, we observed that Vδ1 T lymphocytes from both HIV-1–infected patients and healthy donors are able to proliferate and produce IFN-γ and IL-17 upon stimulation in vitro with C albicans, thus supporting the hypothesis that this γδ T-cell subset may participate in antifungal immune response in vivo. Along this line, 5 patients had a clinical history of C albicans mucosal infections, which recovered without therapy (Table 1). On the other hand, in 4 patients we also detected an increase of peripheral Vδ2 T lymphocytes expressing IFN-γ and IL-17: this T-cell population, isolated from either patients or healthy donors, selectively responded to mycobacterial antigens in vitro, proliferating and producing the 2 cytokines.
Among CD4+ T cells, IL-17–producing cells have been proposed to represent a third lineage of Th cells, called Th17, distinct from Th1 or Th2 cell subsets.32,45 This population displays a memory phenotype, being CD27+, and coexpresses CCR4 and CCR6.32,35 Human memory Th17 cells were found to react against C albicans, whereas memory T cells specific for M tuberculosis displayed a Th1 cell phenotype.32 However, an intermediate population of double-producer CD4+ T cells, with a memory phenotype and expressing CCR6 and CXCR3, has been described.42,46 The double-producer Vδ1 or Vδ2 T cells that we describe here display a central memory phenotype, as they bear not only CD27 at their surface but also CCR7, which is usually lost in effector memory T cells.44 Nevertheless, differentiation of human memory CD4+ T cells has been described as a stepwise process, where a subset of double-positive CD27+CCR7+ T cells can be found.33 Interestingly, this subset can both secrete cytokines and recirculate through lymph nodes, due to the expression of the CCR7 homing receptor.46 Notably, the Vδ1 (and in 4 cases also Vδ2) memory T-cell subset that we found in HIV-1–infected patients also bears the CCR4 and CCR6 chemokine receptors, and, although not shown, they coexpress CXCR3, in keeping with our previous observations.21 Finally, this double-producer cell population expresses the RORC Th17 and the TXB21 Th1 transcription factors and is confined to the CD161+ subset, in agreement to what has been reported for CD4+ T lymphocytes.37-39 It is of note that CD161, also known as NKRP1A, is an adhesion receptor used by Vδ2 T cells for transendothelial migration.40,41
The finding that this specifically equipped circulating memory γδ T-cell population, which has been recently described in mice with Listeria infection,47 is expanded in nonprogressor HIV-1–infected patients might suggest that it plays an important role in the control of HIV-1 spreading and in the defense against opportunistic infections, possibly contributing to compensate for the impairment of CD4+ T cells. Indeed, this T-cell subset not only produces Th1/Th17 cytokines, but expresses several homing and chemokine receptors, thus being equipped for recirculation through lymph nodes and peripheral tissues.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was partially supported by the Italian Ministero della Salute (Coordinated Grant Special Project) and by the Italian Istituto Superiore di Sanità (VI National Project on AIDS Research; A.P. and M.R.Z.).
Authorship
Contribution: D.F., A.F., S.C., and F.B. performed the research; A.P. designed the research, analyzed data, and revised the paper; M.S. and G.M. provided human blood samples from healthy donors and HIV-1–infected patients; and M.R.Z. designed and performed the research, analyzed data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Alessandro Poggi, Laboratory of Immunology, National Institute for Cancer Research, Largo R Benzi 10, I-16132 Genoa, Italy; e-mail: alessandro.poggi@istge.it or Maria Raffaella Zocchi, Division of Immunology, Transplants, and Infectious Diseases, San Raffaele Scientific Institute, Milan, Italy; e-mail: zocchi.maria@hsr.it.

![Figure 4. γδ T lymphocytes producing IFN-γ are also IL-17–producing cells. PBMCs from HIV-1–infected Pts (A,B: 1 representative Pt; C: n = 20 for Pts with increased Vδ1 T cells; D: n = 4 for Pts with increased Vδ2 T cells) or Hds (n = 10, C,D) were surface stained with the FITC–anti-CD3 and PE-conjugated A13 (A) or BB3 (B) mAbs (to identify Vδ1 or Vδ2 T cells, respectively) and cytoplasmically stained with APC-anti–IL-17 and PE-Cy7-anti–IFN-γ (performed immediately after isolation [Ai,Bi] and ex vivo [C,D]) or after 7 days of culture with Ca or PPD, and rIL-2 was added on day 4 (Aii,Bii,C,D). Samples were analyzed by FACSCanto flow cytometer (Becton Dickinson) gating on CD3/Vδ1 (Ai-Aii, C) or CD3/Vδ2 (Bi-ii, D) T cells. Results are expressed as mean far red (APC) fluorescence intensity (x-axis, au) versus mean very far red (PE-Cy7) fluorescence intensity (y-axis, au; Ai-ii, Bi-ii). The percentages depicted in the top right quadrants of contour plots in panels A and B indicate IFN-γ+IL-17+ cells among Vδ1 T cells ex vivo (Ai) or after culture with C albicans (Ca; Aii) or among Vδ2 T cells ex vivo (Bi) or after culture with PPD (Bii). (C-D) IFN-γ+IL-17+ cells gated on CD3/Vδ1 (C) or CD3/Vδ2 (D) T cells, before and after culture with Ca or PPD (mean ± SD from 10 Hds and mean ± SD from 20 in C or 4 Pts in D). *P < .01 versus Hds. **P < .01 versus ex vivo.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/113/26/10.1182_blood-2009-01-198028/4/m_zh89990937940004.jpeg?Expires=1769931453&Signature=n-z7gXj-v77rGiZghHczxhJnKaooNf6w3ml51FYJOm8HQ6e9senzMrgsZ6BOHfK-gpZ8zBx7QsYvAfoEN631FT-NR2xniYZkEjxqT2AK46pH~EJB8qiV~QVkHLqH5NROD3-R4TgnrBz-N8fWexU1HtsORBqLy7e4BuDQpn1pfLqZmbWyCWMNr40JYr0ceeKCsVkGbmBnyNzsD3lPpw8Hnvn9bOhFRzLprdLshx6JWHl5VhZ7LGhPQUyfCFe6JT5UWpqmSd8CEOUU5xOGWYeB0LgjeEVyYfFAMACY~LYrVWKeMGIDYQZ7pdiarIedoFlLHqpMcdJi6WEsPs0I6PF2Bg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 6. γδ T lymphocytes producing IFN-γ and IL-17 express CD161. PBMCs from HIV-1–infected Pts (n = 20) or Hds (n = 10) were stained with the PE-conjugated A13 or BB3 mAbs to identify Vδ1 or Vδ2 T cells, respectively, PerCP-conjugated anti-CD3, and FITC-conjugated anti-CD161 (A-D). Then cells were fixed and permeabilized and cytoplasmically stained with APC-anti–IL-17 and PE-Cy7-anti–IFN-γ was performed on cells before or after 7 days of culture with Ca or PPD and rIL-2 was added on day 4 (B,C: Pts; D: Hds). Samples were analyzed by FACSCanto flow cytometer (Becton Dickinson) gated on CD3/Vδ1 or CD3/Vδ2 cells (A) and on CD161+ or CD161− Vδ1 T cells (C,D). (A) Percentage of CD161+ cells on CD3/Vδ1 or CD3/Vδ2 gated cells as indicated. (B) One representative case of 10 analyzed: PE-Cy7–IFN-γ/APC–IL-17 staining of CD161+ (Bii) or CD161− (Biii) gated cells among Vδ1 T cells (Bi, indicated by []). Results are expressed as log red fluorescence intensity (x-axis, au) versus log green fluorescence intensity (y-axis, au; Bi) or as log far red fluorescence intensity (x-axis, au) versus log very far red fluorescence intensity (y-axis, au; Bii,iii). In panels C-D, results are expressed as percentage of IFN-γ+IL-17+ cells among CD161+Vδ1 or CD161−Vδ1 T cells and are the mean ± SD from 20 Pts (C) or 10 Hds (D). *P < .01 versus cells cultured in the absence of antigens (−). **P < .01 versus Hds.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/113/26/10.1182_blood-2009-01-198028/4/m_zh89990937940006.jpeg?Expires=1769931453&Signature=boV7d3dqWWglEbwUWMTwkzOLWJsoSNpAZxAkHGgeR9GzfGT7-WDAYXJPUzM6poUrYus2jKqZMUiRvwlbrjG7dYwo9ZYhNq3wwHJfGAV8mFMOoDBds6dakEF06e4~5Vy66Mx8Fl0XkPy5PhMSZN4WUdo4zfFfYJPpzACEJo6ydYHgRTVhkMwr5kRcf5dGADqOz1imBAaKiadOiY5YNjlhHG-sBH1caG3F28JX5b4bPvLNNVG8kChkgvp04hlBiUA0ztpNoujRoInGNQqEJ801Xv5h2Ui3Vbw3gS~HDXY4ZtqQFsRZj6QlMjVmrZPOjwX0YX7xv0-rDIAfIpIDMEDBhg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)