Abstract
Inhibitory-cell killer immunoglobulin-like receptors (KIR) negatively regulate natural killer (NK) cell–mediated killing of HLA class I–expressing tumors. Lack of KIR-HLA class I interactions has been associated with potent NK-mediated antitumor efficacy and increased survival in acute myeloid leukemia (AML) patients upon haploidentical stem cell transplantation from KIR-mismatched donors. To exploit this pathway pharmacologically, we generated a fully human monoclonal antibody, 1-7F9, which cross-reacts with KIR2DL1, -2, and -3 receptors, and prevents their inhibitory signaling. The 1-7F9 monoclonal antibody augmented NK cell–mediated lysis of HLA-C–expressing tumor cells, including autologous AML blasts, but did not induce killing of normal peripheral blood mononuclear cells, suggesting a therapeutic window for preferential enhancement of NK-cell cytotoxicity against malignant target cells. Administration of 1-7F9 to KIR2DL3-transgenic mice resulted in dose-dependent rejection of HLA-Cw3–positive target cells. In an immunodeficient mouse model in which inoculation of human NK cells alone was unable to protect against lethal, autologous AML, preadministration of 1-7F9 resulted in long-term survival. These data show that 1-7F9 confers specific, stable blockade of KIR, boosting NK-mediated killing of HLA-matched AML blasts in vitro and in vivo, providing a preclinical basis for initiating phase 1 clinical trials with this candidate therapeutic antibody.
Introduction
Natural killer (NK) cells play critical roles in host defense against infections and tumors, by secreting immunoregulatory cytokines and by killing infected or transformed cells. The activation of NK-cell effector functions is regulated by multiple types of activating and inhibitory receptors that recognize ligands expressed on potential target cells.1 The balance between positive and negative signals transmitted via these NK receptors determines whether or not a target cell is killed by an NK cell.2 Activating receptors include NKp30, NKp44, NKp46, NKG2D, and DNAM-1, among others.3 Their ligands appear preferentially on stressed, transformed, or infected cells, but not on normal, healthy cells.2,4,5 Therefore, transformed or infected cells may provide activation signals and become sensitive to killing by NK cells, whereas healthy cells generally do not.2 NK-cell expression of CD16, the low-affinity Fc receptor, provides an additional mechanism by which NK cells may mediate antitumor effects via antibody-dependent cellular cytotoxicity (ADCC) toward antibody-coated target cells. Signaling through activating NK receptors is negatively regulated via inhibitory receptors, such as killer immunoglobulin (Ig)–like receptors (KIR), CD94/NKG2A, and leukocyte Ig-like receptor-1, which recognize major histocompatibility complex (MHC)–class I molecules. Efficient NK cell–mediated killing occurs when target cells abundantly express stress- or transformation-induced ligands for activating NK receptors, and few or no MHC class I ligands for inhibitory receptors. Cancer cells that retain expression of class I molecules may evade NK-mediated immunosurveillance.6 Conversely, loss of MHC class I expression renders tumor cells more sensitive to killing by NK cells, which may be associated with improved prognosis in some types of cancer.7-9
The human KIR family comprises polymorphic Ig-like molecules expressed on NK cells, and small subsets of CD8+ and γδ+ T cells. Individual KIR bind distinct subgroups of HLA class I allotypes, and are clonally expressed in NK cells, creating a repertoire of NK cells with specificities for different HLA class I molecules. KIR2DL and KIR3DL have long cytoplasmic tails containing inhibitory signaling motifs, and 2 or 3 extracellular Ig domains conferring specificity for HLA-C or HLA-A/B allotypes, respectively. KIR2DL1 and KIR2DL2/3 recognize distinct HLA-C allotypes, based on polymorphisms at positions 77 and 80 in the α1 domain of the HLA heavy chain.10 For example, KIR2DL1 binds HLA-Cw2, -4, -5, and -6, whereas KIR2DL2 and -3 bind to HLA-Cw1, -3, -7, and -8. Collectively, the inhibitory KIR2DL1, -2, and -3 receptors recognize essentially all HLA-C allotypes. In contrast to KIR2DL receptors, KIR2DS and KIR3DS have short cytoplasmic tails with activating potential.11
NK cells may coexpress multiple inhibitory KIRs, and/or other MHC class I–specific inhibitory receptors with different MHC class I specificities. Nevertheless, all people appear to also harbor some NK cells that are inhibited by only one MHC class I allotype.12,13 Thus, the NK population as a whole may detect loss of even a single HLA class I allotype, allowing killing of target cells deficient in only one or a few class I allotypes.7 The clinical relevance of such missing-self recognition has been demonstrated in patients with acute myeloid leukemia (AML), in which haploidentical stem cell transplantation (SCT) led to expansion and activation of donor-derived, KIR-HLA class I–mismatched NK cells, resulting in NK cell–mediated antileukemia responses associated with reduced risk of relapse and increased survival rates, with no risk of graft-versus-host disease.13-17 However, few patients with AML are candidates for transplant-based therapy, and thus, novel treatment options are urgently needed. To explore the feasibility of achieving similar NK-mediated antileukemia activity by a pharmacologic approach that would circumvent the need for SCT, we generated fully human anti-KIR monoclonal antibodies (mAbs) that block the interactions of the 3 main inhibitory KIR2DL with their HLA-C ligands, thereby enhancing NK activity. In this study, we present the in vitro and in vivo characterization of 1-7F9, which formed the basis for selection of this mAb as candidate for clinical development.
Methods
Cell isolation
All patient samples were collected and stored under institutional review board–approved protocols. Patients provided prior written informed consent in accordance with the Declaration of Helsinki, approved by the Ohio State University Comprehensive Cancer Center Institutional Review Board for use of samples. AML blasts were isolated from bone marrow aspirate at diagnosis and cryopreserved. Sample viability was more than 90%. Patients received induction and consolidation chemotherapy, and upon complete remission, peripheral blood mononuclear cells (PBMC) were obtained by Ficoll-Hypaque density gradient centrifugation, which were the source of autologous NK cells for functional assays with patient-derived target cells. For some experiments, NK cells from these patient samples, or from healthy donors (HLA class I high resolution typed), were depleted of T cells by negative CD3 immunomagnetic selection (Miltenyi Biotec), stimulated with irradiated PBMC feeder cells, phytohemagglutinin (Biochrom), and 500 U/mL interleukin (IL)–2 (Chiron), and expanded for up to 2 months.18 Purity of NK cells was confirmed by flow cytometry, and was at least 85% CD56+CD3− lymphocytes in all experiments. NK-cell clones were generated from PBMC of healthy donors.19
Cell lines
KIR2D-transfected BWZ cell lines,20 YTS cells transfected with KIR2DL121 (YTS-2DL1), and 721.221 B-EBV cells transfected with HLA-Cw3 and -4 have been described.22 The 721.221 cells expressing both HLA-Cw3 and HLA-Cw4 molecules were generated by sequential transfection of pCDNA.3-Cw3 and pRSV.5-Cw4, and sorting for high-level HLA-Cw3 and -Cw4 expression by flow cytometry of cells stained with soluble KIR2DL1 and -3.
Antibodies
Fully human anti-KIR mAbs were generated by immunization of KM mice (Medarex) bearing human genomic IgG loci, with BW5417 cells stably transfected with KIR2DL1, followed by 3 booster immunizations with the soluble, extracellular part of KIR2DL3 produced in Escherichia coli. Antibodies were screened for binding to recombinant, soluble KIRs by enzyme-linked immunosorbent assay, and positive clones were tested for binding to YTS-KIR2DL1 cells by flow cytometry. Selected hybridomas were subcloned until stable lines were obtained.
Murine mAbs specific for KIR2DL1/S1 (clones EB6, IgG1, and XA141, IgM), KIR2DL2, -3/S2 (clones GL183, IgG1, and Y249, IgM), KIR2DL1, -2, -3/S1, -S2, -S5 (clone DF200, IgG1), KIR2DS4 (clone FES172, IgG2a), HLA class I (clone A6-136, IgM), and NKG2A (clone Z199, IgG2b) have been described.23-25 Phycoerythrin (PE)–conjugated anti-KIR antibodies were from Beckman Coulter. Human IgG4 (I7385; Sigma-Aldrich) was used as control for 1-7F9.
Flow cytometry
Cell lines.
A total of 105 cells was incubated at 4°C with 1 μg/mL purified human (1-7F9) or murine (EB6, GL183, and/or FES172) anti-KIR mAbs, followed by PE-conjugated mouse anti–human IgG4 (HP6025; Southern Biotechnology Associates) or PE-conjugated goat anti–mouse IgG (Beckman Coulter). Percentages of anti-KIR2D binding were calculated using the following formula: percentage of binding = MFI (mean fluorescence intensity) Cx/MFI C1 × 100, where Cx is the anti-KIR2D concentration in micrograms per milliliter (1 μg/mL represents 100%).
NK populations.
Three-color immunofluorescence was used to analyze expression of KIR and NKG2A on CD56+ NK cells. NK cells were incubated with allophycocyanin-conjugated anti-CD56 (IgG1) plus unconjugated anti-NKG2A (IgG2b), followed by fluorescein isothiocyanate–conjugated goat anti–mouse IgG2b antibodies (Southern Biotechnology Associates), in combination with PE-conjugated anti-KIR2DL2/3/S2 (clone GL183, IgG1), anti-KIR2DL1/S1 (clone EB6B, IgG1), or anti-KIR3DL1/S1 (clone Z27, IgG1).
Whole blood staining.
Blood samples were incubated at room temperature with PE-conjugated 1-7F9 and combinations of cell type–specific mAbs, as indicated.
Binding assays.
Fusion proteins consisting of the extracellular part of KIR2DL1 attached to Fc part of murine or human IgG1 (designated KIR2DL1-mFc and -hFc, respectively) were incubated with human (1-7F9) or mouse (DF200 or GL183) anti-KIR mAbs for 30 minutes on ice. LCL721.221-Cw4 cells were added and incubated for 1 hour on ice, washed, and incubated with allophycocyanin-conjugated F(ab′)2 goat anti–human IgG or anti–mouse IgG, and analyzed by flow cytometry.
CD107/IFN–γ assay.
Cells were processed, as described.26 Briefly, NK cells or PBMC were incubated for 4 hours at 37°C in the presence of 5 μM monensin (Sigma-Aldrich) and fluorescein isothiocyanate–conjugated anti-CD107a and -b mAbs, with or without anti-KIR mAbs, and with or without target cells. After incubation, cells were washed in phosphate-buffered saline and 2 mM EDTA (ethylenediaminetetraacetic acid) and stained for extracellular markers, fixed, permeabilized with IntraPrep reagent (Beckman Coulter), labeled with anti–IFN-γ, and analyzed by flow cytometry.
Cytotoxicity assays
Lysis of 721.221-Cw3 and -4 target cells by NK-cell lines or clones was evaluated in 4-hour 51Cr release assays, as described.23 Lysis of AML blasts by autologous, IL-2–activated NK cells isolated from the same patient in remission was evaluated by standard 51Cr release assay, or by the Topro-3 iodide/PKH-26 flow cytometry–based assay.27 In the latter, target cells labeled with the membrane dye, PKH-26 (Sigma-Aldrich), were coincubated with NK cells at 37°C for 4 hours, and then placed on ice. At the beginning of incubation, 1-7F9, control human IgG4 (hIgG4), or a mixture of mouse anti-KIR F(ab′)2 fragments was added, each at 30 μg/mL final concentration. A total of 10 μL of the viability dye To-Pro3 iodide (1/10000 dilution; Molecular Probes) was added to each well immediately before flow cytometric analysis. Percent specific lysis was determined, as described.27 Cytotoxicity by fresh, patient-derived NK cells toward autologous AML blasts was measured as granzyme B release, using enzyme-linked immunospot (ELISPOT) technique, as described.28 Cytotoxicity results using this methodology correlate closely with results of chromium release and flow cytometric–based methods with the advantage of requiring many fewer cells. Briefly, effector NK cells were incubated for 4 hours with 1-7F9 or hIgG4 isotype control. A total of 5 × 104 target cells/well was aliquoted in triplicate on a polyvinylidene difluoride plate (Millipore) that had been coated overnight with anti–human granzyme B capture antibody (7.5 ug/mL, 3485-3; Mabtech). Effector cells were added, and 12 hours later, plates were washed and anti–human granzyme B detecting antibody (.25 ug/mL, 3485-6; Mabtech) was added to each well. Plates were incubated for 2 to 4 hours with streptavidin alkaline phosphatase (1:1500; Gibco BL Life Technologies), and spots were visualized with 5-bromo-4-chloro-3-indolyl phosphate-nitroblue tetrazolium phosphatase substrate (Kirkegaard & Perry Laboratories). Automated plate evaluation was conducted using the ImmunoSpot Imaging Analyzer System (Cellular Technology).
Mouse models
We crossed Rag−/− and KIR2DL3 transgenic (tg) mice29 to obtain KIR2DL3tg, Rag−/− mice. Cw3tg30 were crossed with KbDb−/− mice,31 resulting in Cw3tg, KbDb−/− mice. Wild-type C57BL/6 mice were purchased from Janvier, and nonobese diabetic–severe combined immunodeficiency (NOD-SCID) mice from Charles River Laboratories. All experiments were performed according to European directive for animal experimentation.
To assess in vivo rejection, splenocytes from donor strains were prepared by lysing red cells with NH4Cl, and incubating leukocytes for 8 minutes at 37°C degrees with .5 or 3 μM carboxy fluorescein succinimidyl ester (CFSE; Invitrogen). Twenty million cells were injected intravenously into groups of 3 recipient mice, which were killed 20 hours later, and the frequency of CFSE-labeled cells in peripheral blood was assessed by flow cytometry. The 1-7F9 antibody was dosed intravenously, and 4 hours later, mice were injected intravenously with 20 million of a 1:1 mixture of tg donor cells labeled with 3 μM CFSE and wild-type C57BL/6-derived cells labeled with .5 μM of CFSE. Twenty hours after cell injection, mice were killed and peripheral blood cells and spleen cells were isolated and analyzed by flow cytometry. In vivo KIR occupancy by 1-7F9 was evaluated by staining cells ex vivo with PE-labeled 1-7F9. Percentage of free receptors was quantified by the ratio of the MFI of 1-7F9–treated animals (mean MFI of 3 treated mice) and the MFI of untreated animals (mean MFI of 3 mice).
NOD-SCID mice were administered 250 μg of 1-7F9 mAb 1 day after 3.5 Gy irradiation. Three hours later, mice were given coinfusion (intravenously) of AML cells (5 × 106) and nonalloreactive, IL-2–activated NK cells (obtained from a healthy donor with same HLA class I allotype groups as the AML cells) at different effector to target (E:T) ratio (1:3, 1:12, 1:18). Mice that succumbed to leukemia were assessed for AML organ infiltration by flow cytometric analysis with anti–human CD45 mAb.
Statistical analysis
Differences between groups were analyzed by Student t test (2 groups) or analysis of variance (ANOVA), followed by Bonferroni posttest (more than 2 groups). Dose responses were fitted with a 1-site saturation-binding equation, and 50% effective concentration (EC50) and confidence intervals (CIs) are reported. Survival analysis was performed using Kaplan Meier log rank test. Significant results (*P < .05, **P < .01, ***P < .005) are reported.
Results
1-7F9 mAb recognizes inhibitory KIR2DL-1, -2, and -3
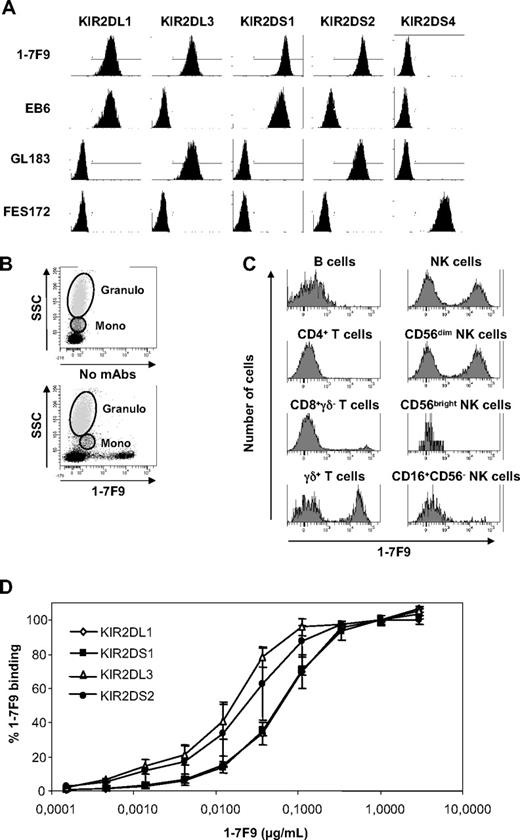
As distinct HLA-C allotypes are recognized by KIR2DL1, -2, and -3, and KIR genes segregate independently of HLA class I, only mAbs that cross-react with these 3 KIRs were expected to be active in the entire population. Hence, we immunized tg mice bearing human Ig loci with different combinations of KIR2DLs. The 1-7F9 mAb was selected based on binding to soluble, recombinant KIR2DL1, -2, and -3 by enzyme-linked immunosorbent assay (data not shown). Recognition of native KIR was confirmed by binding to KIR2DL1, -2, and -3 at the surface of transfected BWZ cells and NK-cell clones (Figure 1A, and data not shown). The 1-7F9 also bound to KIR2DS1 and -2, but not to cells transfected with KIR2DS3, -S4, or -S5 (Figure 1A; supplemental Figure 1, available on the Blood website; see the Supplemental Materials link at the top of the online article); however, we could not confirm surface expression of 2DS3 due to lack of positive control antibodies recognizing 2DS3.
Specificity of 1-7F9 antibody. (A) Characterization of 1-7F9 specificity for KIR2D subtypes. Transduced BWZ cells expressing individual KIR2DL or KIR2DS receptors were incubated for 30 minutes with anti-KIR antibodies (1 μg/mL), as indicated. The 1-7F9 was detected with PE anti–human IgG4, and EB6, GL183, and FES172 were revealed with PE goat anti–mouse IgG. Results shown are representative of 4 separate experiments. (B) Human whole blood from a healthy volunteer was stained with PE-conjugated 1-7F9; dot plots represent 1-7F9 binding to the indicated leukocyte subsets based on forward/side light scatter. (C) Human whole blood from a healthy volunteer was stained with PE-conjugated 1-7F9 and a combination of mAbs defining various leukocyte subsets, and analyzed by flow cytometry. Experiments in panels B and C have been performed on 11 healthy donors. Mean percentage and SD of 1-7F9–positive cells among the NK- and T-cell populations were 48.1% ± 14.9 and 2.4% ± 2.1, respectively. (D) Titration of 1-7F9 mAb on KIR2D-transduced BWZ cell lines. Cells were incubated for 30 minutes with 1/3 serial dilutions of 1-7F9, which were then revealed with PE anti–human IgG4 and analyzed by flow cytometry. Each dilution point was performed in duplicate.  , ■, ▲, and ● represent cell lines expressing KIR2DL1, KIR2DS1, KIR2DL3, and KIR2DS2, respectively. Mean and SD of data collected in 2 independent experiments are shown.
, ■, ▲, and ● represent cell lines expressing KIR2DL1, KIR2DS1, KIR2DL3, and KIR2DS2, respectively. Mean and SD of data collected in 2 independent experiments are shown.
Specificity of 1-7F9 antibody. (A) Characterization of 1-7F9 specificity for KIR2D subtypes. Transduced BWZ cells expressing individual KIR2DL or KIR2DS receptors were incubated for 30 minutes with anti-KIR antibodies (1 μg/mL), as indicated. The 1-7F9 was detected with PE anti–human IgG4, and EB6, GL183, and FES172 were revealed with PE goat anti–mouse IgG. Results shown are representative of 4 separate experiments. (B) Human whole blood from a healthy volunteer was stained with PE-conjugated 1-7F9; dot plots represent 1-7F9 binding to the indicated leukocyte subsets based on forward/side light scatter. (C) Human whole blood from a healthy volunteer was stained with PE-conjugated 1-7F9 and a combination of mAbs defining various leukocyte subsets, and analyzed by flow cytometry. Experiments in panels B and C have been performed on 11 healthy donors. Mean percentage and SD of 1-7F9–positive cells among the NK- and T-cell populations were 48.1% ± 14.9 and 2.4% ± 2.1, respectively. (D) Titration of 1-7F9 mAb on KIR2D-transduced BWZ cell lines. Cells were incubated for 30 minutes with 1/3 serial dilutions of 1-7F9, which were then revealed with PE anti–human IgG4 and analyzed by flow cytometry. Each dilution point was performed in duplicate.  , ■, ▲, and ● represent cell lines expressing KIR2DL1, KIR2DS1, KIR2DL3, and KIR2DS2, respectively. Mean and SD of data collected in 2 independent experiments are shown.
, ■, ▲, and ● represent cell lines expressing KIR2DL1, KIR2DS1, KIR2DL3, and KIR2DS2, respectively. Mean and SD of data collected in 2 independent experiments are shown.
Specificity was further evaluated by analyzing binding of PE-conjugated 1-7F9 in whole human blood. Subsets of NK cells and γδ T cells, and few CD8+ T cells, were stained by 1-7F9 (Figure 1B-C), consistent with the known expression pattern of KIRs.32-35 Weak binding to monocytes was observed in some experiments (Figure 1B bottom dot plot), which could be prevented by inclusion of 10% to 20% human serum, or by mAbs to CD64, the high affinity Fc receptor (data not shown). The isotype of 1-7F9 was determined to be IgG4, which is known to bind CD64 with lower affinity than other IgG isotypes, and therefore is considered appropriate for a blocking, nondepleting therapeutic mAb.
Titration analysis indicated that 1-7F9 binds to cell surface KIR2DL1/S1 and KIR2DL3/S2 with EC50 at approximately 0.04 and 0.01 μg/mL, corresponding to 0.3 and 0.08 nM, respectively (Figure 1D). Consistently, Biacore analysis indicated bivalent avidities of 1-7F9 for KIR2DL1 and 2DL3 to be 0.43 and 0.025 nM.
1-7F9 antagonizes inhibitory KIR signaling
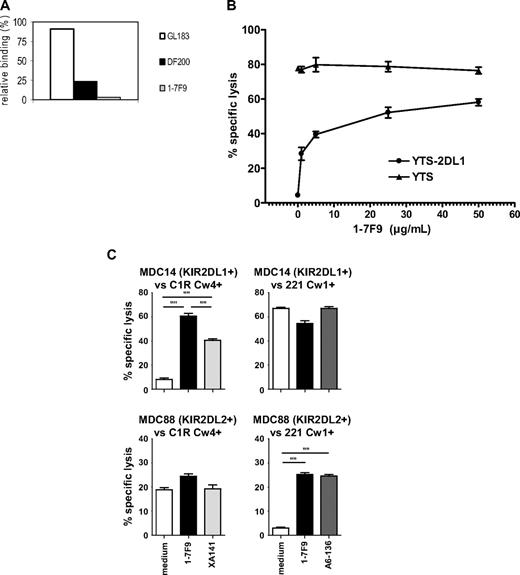
To characterize the biologic effects of 1-7F9 binding to KIR, we first tested the capacity of 1-7F9 mAb to prevent interactions of KIR2DL1 with HLA-Cw4. Binding of soluble, recombinant KIR2DL1-Fc to 721.221-Cw4 transfectants was effectively competed by 1-7F9 (Figure 2A). The functional effect of binding 1-7F9 to KIR was evaluated in cytotoxicity assays. In a dose-dependent manner, 1-7F9 augmented the lysis of .221-Cw4 target cells by an NK-cell line transfected with KIR2DL1 (YTS-2DL1 cells), but did not affect lysis by KIR-negative YTS cells (Figure 2B). The 1-7F9 mAb also increased cytotoxicity mediated by human NK-cell clones expressing KIR2DL1, -2, or -3 toward targets cells expressing HLA-Cw4 or -Cw3, respectively (Figure 2C; supplemental Figure 2). Taken together, these results indicated that 1-7F9 effectively blocks binding of HLA class I to inhibitory KIR2DLs, resulting in increased NK cell–mediated killing of target cells expressing HLA-C.
1-7F9 blocks interactions of inhibitory KIR2DL with HLA class I on B-EBV cells. (A) Binding of soluble KIR2DL1-hFc was blocked by anti-KIR mAbs GL183 or DF200 and binding of KIR2DL1-mFc blocked by 1-7F9, as measured by flow cytometry. Relative binding of KIR-Fc proteins to .221-Cw4 cells is shown as percentage of binding by KIR-Fc in the absence of mAbs. Similar data were obtained in a repeat experiment. (B) In a 51Cr release cytotoxicity assay, YTS cells efficiently killed LCL721.221-Cw4 cells (▲), whereas YTS-2DL1 cells did not (●; E:T ratio 12:1). Preincubation (30 minutes at 37°C) of the NK cells with increasing doses of 1-7F9 augmented the killing of LCL721.221-Cw4 targets by YTS-2DL1 cells, in a dose-dependent manner. Curve fitting using one-site receptor saturation equation gives an EC50 of 0.71 μg/mL (95% CI, 0.2-1.2 μg/mL). Experiment shown is representative of multiple experiments giving equivalent results. (C) NK-cell clones were tested for cytolytic activity against B-EBV cell lines transfected with indicated HLA class I allotypes at 10:1 E:T ratio, with or without mAb at 10 μg/mL. NK clone MDC14 (top panels) is KIR2DL1+, KIR2DL2/3−, NKG2A−. NK clone MDC88 (bottom panels) is KIR2L1−, KIR2DL2+, KIR2DL3−, NKG2A−. Killing by these NK cells was tested against B-EBV cell lines transfected with HLA-Cw4 (left panels) and HAL-Cw1 (right panels). Results were analyzed by ANOVA, followed by Bonferroni posttest; only P < .001 are reported.
1-7F9 blocks interactions of inhibitory KIR2DL with HLA class I on B-EBV cells. (A) Binding of soluble KIR2DL1-hFc was blocked by anti-KIR mAbs GL183 or DF200 and binding of KIR2DL1-mFc blocked by 1-7F9, as measured by flow cytometry. Relative binding of KIR-Fc proteins to .221-Cw4 cells is shown as percentage of binding by KIR-Fc in the absence of mAbs. Similar data were obtained in a repeat experiment. (B) In a 51Cr release cytotoxicity assay, YTS cells efficiently killed LCL721.221-Cw4 cells (▲), whereas YTS-2DL1 cells did not (●; E:T ratio 12:1). Preincubation (30 minutes at 37°C) of the NK cells with increasing doses of 1-7F9 augmented the killing of LCL721.221-Cw4 targets by YTS-2DL1 cells, in a dose-dependent manner. Curve fitting using one-site receptor saturation equation gives an EC50 of 0.71 μg/mL (95% CI, 0.2-1.2 μg/mL). Experiment shown is representative of multiple experiments giving equivalent results. (C) NK-cell clones were tested for cytolytic activity against B-EBV cell lines transfected with indicated HLA class I allotypes at 10:1 E:T ratio, with or without mAb at 10 μg/mL. NK clone MDC14 (top panels) is KIR2DL1+, KIR2DL2/3−, NKG2A−. NK clone MDC88 (bottom panels) is KIR2L1−, KIR2DL2+, KIR2DL3−, NKG2A−. Killing by these NK cells was tested against B-EBV cell lines transfected with HLA-Cw4 (left panels) and HAL-Cw1 (right panels). Results were analyzed by ANOVA, followed by Bonferroni posttest; only P < .001 are reported.
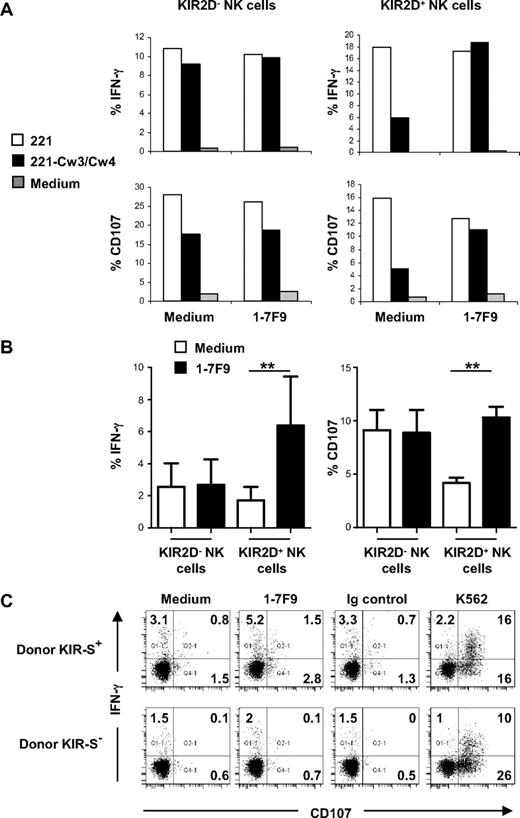
IL-2–activated NK cells, as used in the above experiments, are more sensitive to activation signals than resting NK cells.36 To test whether 1-7F9 may affect activation of resting NK cells, we incubated freshly isolated human NK cells with .221 cells transfected with both HLA-Cw3 and -Cw4, and used flow cytometry to quantitate levels of intracellular IFN-γ and cell surface CD107, as measures of NK-cell activation. By costaining for cell surface KIR, this assay allowed to distinguish activation of KIR-positive versus KIR-negative NK cells. In the absence of .221 target cells, 1-7F9 alone did not induce activation of resting NK cells (Figure 3A; supplemental Figure 3). Addition of HLA class I–negative .221 cells resulted in very low levels of activation of KIR-negative or KIR-positive resting NK cells (data not shown). This result is in line with a previous report that indicated that resting NK cells were unable to lyse insect cells, unless the latter were coated with antibodies cross-linking CD16 on NK cells.36 To induce detectable activation of the resting NK cells, we preincubated .221 target cells with rituximab, to cross-link CD20 on the B cells with CD16 Fc receptors on NK cells. This led to up-regulation of IFN-γ and CD107, on both KIR-positive and KIR-negative NK cells (Figure 3A). The .221-Cw3/Cw4 transfectants, coated with rituximab, induced significantly less activation of KIR-positive than KIR-negative NK cells, reflecting inhibition via HLA-C. Addition of 1-7F9 restored activation of KIR-positive NK cells to levels observed with KIR-negative NK cells, indicating that 1-7F9 effectively blocks inhibitory KIR function in resting NK cells activated via ADCC (Figure 3A).
1-7F9 interferes with HLA class I-induced inhibitory signaling in KIR2DL-positive resting NK cells. (A) Freshly purified human NK cells were incubated overnight in medium. Then NK cells were incubated for 4 hours at 37°C alone (medium; ▩), with rituximab-coated 221 cells (E:T ratio = 1; □), or rituximab-coated 221-Cw3/Cw4 (E:T ratio = 1; ■) in the presence or not of 1-7F9 (10 μg/mL) and with anti-CD107 and monensin. Cells were then stained with anti-CD3, anti-CD56, and purified 1-7F9 revealed by anti–human IgG4 (HP6025); fixed; permeabilized; and finally stained with anti–IFN-γ. Percentage of IFN-γ positive (top panels) and CD107 positive (bottom panels) was then assessed on KIR2D-negative NK cells (left panels) and KIR2D-positive NK cells (right panels). Results from 1 representative donor are shown. (B) Data represent means ± SD of the percentages of IFN-γ–positive NK cells (left panel) and of CD107-positive NK cells (right panel) collected using method described in panel A, from 6 people. Results in the presence of 221-Cw3/Cw4 are shown. Statistical analysis was performed using first a one-way repeated measures ANOVA test, followed by a Bonferroni test to compare pairs of values (ie, KIR2D− medium with KIR2D− 1-7F9 and KIR2D+ medium with KIR2D+ 1-7F9). **P < .01. Multiple experiments have also been performed with 221 transfected with single HLA-C and provided similar results. (C) Thawed human PBMC from KIR-S–positive (1 and 2) or KIR-S–negative (3 and 4) donors were incubated for 4 hours at 37°C, alone or in the presence of 1-7F9 (10 μg/mL), cognate isotypic control (IgG4, 10 μg/mL), or K562 (E:T ratio = 10) in the presence of anti-CD107 and monensin. After incubation, cells were stained with anti-CD3 and anti-CD56, and then fixed, permeabilized, and stained with anti–IFN-γ. CD107 mobilization and IFN-γ production are then assessed on NK cells (CD3−CD56+ lymphocytes). Results are representative of 1 experiment of 2 done with a KIR-S–positive and a KIR-S–negative donor. Percentage of cells in each quadrant is shown.
1-7F9 interferes with HLA class I-induced inhibitory signaling in KIR2DL-positive resting NK cells. (A) Freshly purified human NK cells were incubated overnight in medium. Then NK cells were incubated for 4 hours at 37°C alone (medium; ▩), with rituximab-coated 221 cells (E:T ratio = 1; □), or rituximab-coated 221-Cw3/Cw4 (E:T ratio = 1; ■) in the presence or not of 1-7F9 (10 μg/mL) and with anti-CD107 and monensin. Cells were then stained with anti-CD3, anti-CD56, and purified 1-7F9 revealed by anti–human IgG4 (HP6025); fixed; permeabilized; and finally stained with anti–IFN-γ. Percentage of IFN-γ positive (top panels) and CD107 positive (bottom panels) was then assessed on KIR2D-negative NK cells (left panels) and KIR2D-positive NK cells (right panels). Results from 1 representative donor are shown. (B) Data represent means ± SD of the percentages of IFN-γ–positive NK cells (left panel) and of CD107-positive NK cells (right panel) collected using method described in panel A, from 6 people. Results in the presence of 221-Cw3/Cw4 are shown. Statistical analysis was performed using first a one-way repeated measures ANOVA test, followed by a Bonferroni test to compare pairs of values (ie, KIR2D− medium with KIR2D− 1-7F9 and KIR2D+ medium with KIR2D+ 1-7F9). **P < .01. Multiple experiments have also been performed with 221 transfected with single HLA-C and provided similar results. (C) Thawed human PBMC from KIR-S–positive (1 and 2) or KIR-S–negative (3 and 4) donors were incubated for 4 hours at 37°C, alone or in the presence of 1-7F9 (10 μg/mL), cognate isotypic control (IgG4, 10 μg/mL), or K562 (E:T ratio = 10) in the presence of anti-CD107 and monensin. After incubation, cells were stained with anti-CD3 and anti-CD56, and then fixed, permeabilized, and stained with anti–IFN-γ. CD107 mobilization and IFN-γ production are then assessed on NK cells (CD3−CD56+ lymphocytes). Results are representative of 1 experiment of 2 done with a KIR-S–positive and a KIR-S–negative donor. Percentage of cells in each quadrant is shown.
To test whether 1-7F9 may break NK-cell tolerance to normal self, levels of IFN-γ and CD107 were measured in fresh, resting NK cells among human PBMC incubated with or without the mAb. As 1-7F9 cross-reacts with the short-tailed KIR2DS1 and -2, which potentially may activate NK cells upon cross-linking,19,24 PBMC from KIR2DS-positive and KIR2DS-negative donors were compared. However, when used to stimulate PBMC from KIR2DS-positive donors, 1-7F9 resulted only in low increments in the absolute number of NK cells expressing IFN-γ and/or CD107 (Figure 3C), suggesting that 1-7F9 does not induce efficient cross-linking of KIR2DS.
The 1-7F9 antibody did not significantly affect activation of resting NK cells in PBMC from KIR2DS-negative donors, suggesting that blockade of inhibitory KIR by 1-7F9 does not break NK-cell tolerance to normal self. Furthermore, 1-7F9 also did not induce activation of NK cells in fresh whole human blood from KIR2DS-positive or KIR2DS-negative donors (data not shown), and did not lead to killing of PBMC (supplemental Figure 4).
These results suggested that 1-7F9 effectively blocks inhibitory signaling via KIR2DLs, lowering the threshold for triggering NK-cell effector functions in the presence of transformed target cells that provide sufficient levels of activation signals, but not in the presence of normal, healthy cells.
1-7F9 enhances in vitro NK-cell cytotoxicity against AML tumor cells
To further evaluate effects of 1-7F9 on NK activation in models of greater clinical relevance, we first measured the lysis of patient-derived AML blasts by IL-2–activated NK cells from a HLA-C–matched donor. Only low levels of lysis were observed in the absence of antibody. Inclusion of 1-7F9 led to significant cytotoxicity of the AML blasts (Figure 4A), demonstrating that the mAb can interfere with the protection conferred by expression of HLA-C on primary tumor cells. Next, we tested whether 1-7F9 could enhance killing of primary AML blasts isolated from patients at diagnosis by autologous NK cells collected from the same patient when in remission, and expanded in IL-2 in vitro. NK cells pretreated with 1-7F9 showed a 2- to 3-fold increase in cytotoxicity against the autologous AML blasts, as measured by a flow cytometry–based assay, compared with NK cells pretreated with isotype control antibody (Figure 4B). Comparable levels of cytotoxicity were observed when preincubating NK cells with a mixture of F(ab′)2 fragments of mouse anti-KIR2DL1 and -2DL2/3 mAbs, suggesting that 1-7F9 effectively blocked inhibitory signaling via the major HLA-C–specific KIR.
1-7F9 increases NK cell–mediated lysis of primary AML blasts. (A) Lysis of primary AML cells by IL-2–activated NK cells of a healthy, KIR ligand-matched donor, in the presence of 1-7F9 at 10 μg/mL (▨) or without antibody (□), measured in standard 51Cr assay at the indicated E:T ratios. Differences were analyzed by Student t test (***P < .005). Experiment shown is representative of different experiments using different effector and target blast cells. (B) Patient NK cells expanded in IL-2 were mixed with freshly thawed, autologous AML blasts obtained at diagnosis. The 1-7F9, control hIgG4, or a mixture of mouse anti-KIR2DL1 and -2/3 F(ab′)2 fragments was added to each well (each at 30 μg/mL final concentration), and after 4 hours, percent specific lysis was measured by a flow cytometry–based assay. Results shown are representative of 4 independent experiments. (C) Patient NK cells (n = 4 for the E:T 30:1 level, plus n = 5 at E:T 15:1) were incubated with 1-7F9 or hIgG4 isotype control mAb and cocultured in the presence of autologous AML blasts. Cytotoxicity, measured as granzyme B release, is shown. Statistically significant differences in cytotoxicity (*P = .01; **P < .03), as a function of granzyme B release were observed at multiple E:T ratios as shown (■ = 1-7F9; ▩ = IgG4 isotype control). No appreciable granzyme B release was found in effectors and targets cultured alone (negative controls for the assay). As a positive control for the ELISPOT granzyme B assay readout, an equivalent number of NK cells from a healthy donor was cultured in 30:1 ratio against the NK cell–sensitive K562 cell line (■). Results are representative of 2 independent experiments in 2 patients.
1-7F9 increases NK cell–mediated lysis of primary AML blasts. (A) Lysis of primary AML cells by IL-2–activated NK cells of a healthy, KIR ligand-matched donor, in the presence of 1-7F9 at 10 μg/mL (▨) or without antibody (□), measured in standard 51Cr assay at the indicated E:T ratios. Differences were analyzed by Student t test (***P < .005). Experiment shown is representative of different experiments using different effector and target blast cells. (B) Patient NK cells expanded in IL-2 were mixed with freshly thawed, autologous AML blasts obtained at diagnosis. The 1-7F9, control hIgG4, or a mixture of mouse anti-KIR2DL1 and -2/3 F(ab′)2 fragments was added to each well (each at 30 μg/mL final concentration), and after 4 hours, percent specific lysis was measured by a flow cytometry–based assay. Results shown are representative of 4 independent experiments. (C) Patient NK cells (n = 4 for the E:T 30:1 level, plus n = 5 at E:T 15:1) were incubated with 1-7F9 or hIgG4 isotype control mAb and cocultured in the presence of autologous AML blasts. Cytotoxicity, measured as granzyme B release, is shown. Statistically significant differences in cytotoxicity (*P = .01; **P < .03), as a function of granzyme B release were observed at multiple E:T ratios as shown (■ = 1-7F9; ▩ = IgG4 isotype control). No appreciable granzyme B release was found in effectors and targets cultured alone (negative controls for the assay). As a positive control for the ELISPOT granzyme B assay readout, an equivalent number of NK cells from a healthy donor was cultured in 30:1 ratio against the NK cell–sensitive K562 cell line (■). Results are representative of 2 independent experiments in 2 patients.
As we had observed only marginal activation of resting NK cells challenged with B-EBV target cells, despite robust killing of the same targets by IL-2–activated NK cells, we tested whether AML blasts may express sufficient levels of activating ligands to allow induction of NK-mediated killing by resting NK cells, when KIR is blocked by 1-7F9. In a sensitive granzyme ELIPOT assay, fresh autologous NK cells pretreated with 1-7F9 were shown to exert a 2- to 3-fold increase in cytotoxicity against autologous AML blasts compared with primary autologous NK cells pretreated with isotype control antibody and AML blasts (Figure 4C).
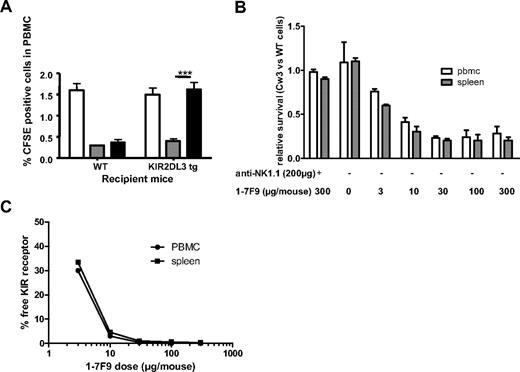
1-7F9 enhances in vivo NK-cell cytotoxicity
The above experiments demonstrate that inhibitory KIR blockade by 1-7F9 augments human NK-cell effector responses against primary, autologous AML blasts. However, it remained to be tested whether 1-7F9 could mediate activation of peripheral or tissue NK cells in vivo. Because mice lack KIR genes, a tg system was developed to test in vivo effects of 1-7F9, based on mice expressing a human KIR2DL3 transgene.29 To confirm that the KIR2DL3 receptor is functional in these mice, we first compared rejection of splenocytes isolated from MHC class I–negative KbDb knockout (KO) mice or from Cw3tg, KbDbKO tg mice, which express the HLA-Cw3 ligand of KIR2DL3, but no murine MHC class I that would engage endogenous inhibitory Ly49 receptors on mouse NK cells. HLA class I–negative cells were efficiently rejected in KIR2DL3tg mice, comparable with the level of rejection obtained in wild-type B6 mice (Figure 5A). In contrast, Cw3tg, KbDbKO cells were protected from NK-mediated lysis, demonstrating that the KIR transgene confers inhibitory signals, preventing killing of Cw3-expressing cells.
Receptor occupancy and functional activity of 1-7F9 in KIR2DL3tg mice. (A) KIR2DL3 is functional in tg mice. Splenocytes from wild-type (□) and from genetically modified mice (▩, KbDbKO cells; ■, KbDbKO Cw3tg cells), labeled with 0.5 and 3 μM CFSE, respectively, were mixed 1:1 (10 million each) and injected (i.v.) into wild-type or KIR2DL3tg mice. Twenty hours later, the mean percentage ± SD (3 to 6 mice per group) of cells with each level of CFSE was determined by flow cytometry. Results were analyzed by ANOVA, followed by Bonferroni posttest (***P < .005). (B) Single injection of 1-7F9 induces rejection of HLA-Cw3–positive splenocytes in a NK-dependent manner. Spleen cells from wild-type and KbDbKO, Cw3tg mice were labeled differentially with CFSE, as in panel A, and were injected into Rag KO, KIR2DL3tg mice. Four hours before the cells, 1-7F9 and NK1.1 mAbs were injected intravenously at the indicated doses. Twenty hours after injection of cells, percentage of cells with each level of CFSE was determined in blood (□) and spleen (▩) by flow cytometry, and the ratio of tg to wild-type donor cells is reported. In some animals, NK cells were depleted by administration of NK1.1 mAb (200 μg per mouse, intravenously). Curve fitting using receptor saturation equation gives an EC50 of 4.6 μg per mouse (95% CI, 1.5-7.7). Experiment shown is representative of 2 different experiments. (C) Maximum effect of 1-7F9 is achieved when KIR2DL3 receptor is saturated. The level of KIR2DL3 receptor occupancy after injection of 1-7F9 was estimated by flow cytometry. Cells from blood and spleen of mice were stained ex vivo with PE-conjugated 1-7F9, and the total MFI of the NK population (a measure of the free receptors) is determined. The level of receptor saturation at a given dose is calculated as the ratio of MFI obtained in mice injected with 1-7F9 relative to MFI obtained in untreated mice (3 mice per group). Receptor occupancy was measured in parallel with the determination of ratio of CFSE-labeled cells in B (24 hours after injection of 1-F9).
Receptor occupancy and functional activity of 1-7F9 in KIR2DL3tg mice. (A) KIR2DL3 is functional in tg mice. Splenocytes from wild-type (□) and from genetically modified mice (▩, KbDbKO cells; ■, KbDbKO Cw3tg cells), labeled with 0.5 and 3 μM CFSE, respectively, were mixed 1:1 (10 million each) and injected (i.v.) into wild-type or KIR2DL3tg mice. Twenty hours later, the mean percentage ± SD (3 to 6 mice per group) of cells with each level of CFSE was determined by flow cytometry. Results were analyzed by ANOVA, followed by Bonferroni posttest (***P < .005). (B) Single injection of 1-7F9 induces rejection of HLA-Cw3–positive splenocytes in a NK-dependent manner. Spleen cells from wild-type and KbDbKO, Cw3tg mice were labeled differentially with CFSE, as in panel A, and were injected into Rag KO, KIR2DL3tg mice. Four hours before the cells, 1-7F9 and NK1.1 mAbs were injected intravenously at the indicated doses. Twenty hours after injection of cells, percentage of cells with each level of CFSE was determined in blood (□) and spleen (▩) by flow cytometry, and the ratio of tg to wild-type donor cells is reported. In some animals, NK cells were depleted by administration of NK1.1 mAb (200 μg per mouse, intravenously). Curve fitting using receptor saturation equation gives an EC50 of 4.6 μg per mouse (95% CI, 1.5-7.7). Experiment shown is representative of 2 different experiments. (C) Maximum effect of 1-7F9 is achieved when KIR2DL3 receptor is saturated. The level of KIR2DL3 receptor occupancy after injection of 1-7F9 was estimated by flow cytometry. Cells from blood and spleen of mice were stained ex vivo with PE-conjugated 1-7F9, and the total MFI of the NK population (a measure of the free receptors) is determined. The level of receptor saturation at a given dose is calculated as the ratio of MFI obtained in mice injected with 1-7F9 relative to MFI obtained in untreated mice (3 mice per group). Receptor occupancy was measured in parallel with the determination of ratio of CFSE-labeled cells in B (24 hours after injection of 1-F9).
In KIR2DL3tg mice, the transgene is controlled by a H-2Kb promoter and IgH enhancer, resulting in KIR expression on approximately 85% of circulating peripheral blood lymphocytes, including T cells and NK cells.29 To analyze the effect of blocking KIR on NK cells specifically, we generated KIR2DL3tg, Rag−/− mice, which expressed KIR2DL3 on virtually all NK cells (supplemental Figure 5); absolute NK-cell numbers remain comparable with wild-type B6 mice. In KIR2DL3tg, Rag−/− mice, the 1-7F9 mAb increased rejection of CFSE-labeled PBMC or splenocytes from Cw3tg, KbDbKO mice in a dose-dependent fashion (Figure 5B). This rejection was NK cell–dependent, as prior depletion of NK cells by NK1.1 antibody completely abrogated the effect (Figure 5B). Maximum rejection at 20 hours was obtained at 30 μg of 1-7F9, which was the lowest dose that resulted in full KIR occupancy in these in vivo experiments (Figure 5C), indicating a good correspondence between KIR binding by the 1-7F9 mAb and its in vivo functional efficacy. Thus, injection of 1-7F9 antibody alone is capable of inducing NK cell–mediated rejection of exogenous Cw3-positive cells in KIR2DL3tg, Rag−/− mice.
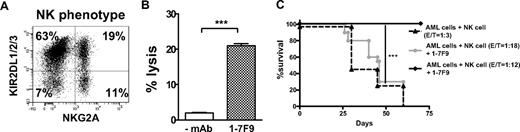
In vivo antitumor cell efficacy of 1-7F9 was further evaluated in a NOD-SCID mouse model of NK-mediated tumor rejection. NOD-SCID mice are immunologically tolerant to cells from other species, and do not reject human NK cells or tumor cells. The 1-7F9 promoted rejection of transformed B-cell lines by NK cells in NOD-SCID mice (supplemental Figure 6). Primary AML blasts were inoculated together with HLA-C–matched NK cells, a majority of which expressed KIR2DLs (Figure 6A). These NK cells did not significantly lyse the AML blasts in vitro, whereas addition of 1-7F9 resulted in robust NK-mediated killing (Figure 6B). Infusion of NK cells and AML blasts alone resulted in a high rate of mortality. A single injection of 1-7F9 was sufficient to rescue the mice, resulting in long-term survival (Figure 6C). At 3 months, mice were killed and did not display leukemic infiltration of spleen and bone marrow. Thus, 1-7F9 significantly augmented NK-mediated elimination of primary AML blasts in vivo.
1-7F9–induced clearance of AML cells by human NK cells in NOD-SCID mice. (A) Flow cytometric analysis of KIR and NKG2A expression by the polyclonal IL-2–activated NK-cell population that was used as effector cells in the in vitro cytotoxicity and the in vivo tumor rejection experiments shown in panels B and C, respectively. (B) □, Lysis of primary human AML cells by KIR ligand-matched NK cells, without (□) or with 1-7F9 antibody ( ). (The NK cells were isolated from a healthy donor having the same HLA class I allotype groups as the AML target cells.) E:T ratio was 15:1. Results were analyzed by Student t test (***P < .005). (C) NOD-SCID mice infused with autologous NK cells and AML target cells at 1:3 E:T ratio died of leukemia within 65 days. Treatment with 1-7F9 (250 μg/mouse) rescued mice challenged with NK and AML cells at an E:T ratio of 1:12, but not at an E:T of 1:18. N = 5 mice per group. Results have been analyzed by Kaplan Meier log rank test (***P < .005). Similar results were obtained in a repeat experiment.
). (The NK cells were isolated from a healthy donor having the same HLA class I allotype groups as the AML target cells.) E:T ratio was 15:1. Results were analyzed by Student t test (***P < .005). (C) NOD-SCID mice infused with autologous NK cells and AML target cells at 1:3 E:T ratio died of leukemia within 65 days. Treatment with 1-7F9 (250 μg/mouse) rescued mice challenged with NK and AML cells at an E:T ratio of 1:12, but not at an E:T of 1:18. N = 5 mice per group. Results have been analyzed by Kaplan Meier log rank test (***P < .005). Similar results were obtained in a repeat experiment.
1-7F9–induced clearance of AML cells by human NK cells in NOD-SCID mice. (A) Flow cytometric analysis of KIR and NKG2A expression by the polyclonal IL-2–activated NK-cell population that was used as effector cells in the in vitro cytotoxicity and the in vivo tumor rejection experiments shown in panels B and C, respectively. (B) □, Lysis of primary human AML cells by KIR ligand-matched NK cells, without (□) or with 1-7F9 antibody ( ). (The NK cells were isolated from a healthy donor having the same HLA class I allotype groups as the AML target cells.) E:T ratio was 15:1. Results were analyzed by Student t test (***P < .005). (C) NOD-SCID mice infused with autologous NK cells and AML target cells at 1:3 E:T ratio died of leukemia within 65 days. Treatment with 1-7F9 (250 μg/mouse) rescued mice challenged with NK and AML cells at an E:T ratio of 1:12, but not at an E:T of 1:18. N = 5 mice per group. Results have been analyzed by Kaplan Meier log rank test (***P < .005). Similar results were obtained in a repeat experiment.
). (The NK cells were isolated from a healthy donor having the same HLA class I allotype groups as the AML target cells.) E:T ratio was 15:1. Results were analyzed by Student t test (***P < .005). (C) NOD-SCID mice infused with autologous NK cells and AML target cells at 1:3 E:T ratio died of leukemia within 65 days. Treatment with 1-7F9 (250 μg/mouse) rescued mice challenged with NK and AML cells at an E:T ratio of 1:12, but not at an E:T of 1:18. N = 5 mice per group. Results have been analyzed by Kaplan Meier log rank test (***P < .005). Similar results were obtained in a repeat experiment.
Discussion
There is still a significant need for novel therapies for AML patients who cannot be cured by chemotherapy or SCT. Specific transplantation protocols, initially involving haploidentical donors14 and subsequently expanded to HLA-matched settings, revealed potent antileukemia efficacy of donor-derived NK cells expressing KIRs that failed to bind a ligand in recipients.37 Clinical efficacy correlated with presence of donor-derived alloreactive NK cells that could lyse patient target cells due to lack of engagement of inhibitory KIR. Extrapolating on this principle, we generated and characterized in this study a fully human anti-KIR therapeutic candidate mAb, 1-7F9, which is now in clinical development with the overall aim of boosting antitumor responses of endogenous NK cells in patients with hematologic malignancies, without transplantation.
The 1-7F9 mAb was selected as lead candidate for clinical development first on the basis of its binding to KIR2DL1, -2, and -3 at the surface of NK cells. A second important criterion was the ability of 1-7F9 to block binding of these KIR to their HLA-C ligands. In functional experiments with NK clones and polyclonal NK-cell populations, 1-7F9 blocked inhibitory KIR signaling mediated by both HLA-C group 1 and group 2 allotypes. An antibody with this binding profile should reduce inhibitory signaling in a subset of NK cells in all people. Nevertheless, at least some NK cells may still receive inhibitory signals via other KIRs, specific for HLA-A or -B allotypes, and via CD94/NKG2A, which recognizes HLA-E, or other inhibitory receptors that recognize non-MHC ligands.38 Results of haploidentical allotransplantations in patients with AML indicate that NK allorecognition due to absence of inhibition via KIR2DL receptors is sufficient to allow clinically meaningful antitumor efficacy by NK cells. As CD94/NKG2A recognize nonpolymorphic HLA-E, and leukocyte Ig-like receptor-1 binds a broad range of HLA-A, -B, and -C allotypes, these receptors are expected to still engage their ligands in recipients of haploidentical SCT.
As the therapeutic mechanism of action relies on augmenting NK-cell activity, it was important that the lead candidate antibody does not cause depletion of NK cells by complement- or antibody-dependent cytotoxicity. The 1-7F9 antibody is an IgG4, an isotype that has been used for other therapeutic antibodies and is known to not activate complement, is not bound by CD16, and exhibiting only residual binding to CD64 on monocytes, which can be competed by human IgG1. Accordingly, 1-7F9 did not induce depletion of KIR-positive cells in whole blood, or in PBMC in the presence of human serum, although weak binding to monocytes was detected in the absence of serum or purified human IgG.
The 1-7F9 mAb also binds to the short-tailed KIR2DS1 and -2 molecules. Such cross-reactivity is not surprising because the extracellular portions of KIR2DS1 and KIR2DS2 differ from those of KIR2DL1 and KIR2DL2/3 by only 7 and 3/4 amino acids, respectively.11,39 However, possibly because of its IgG4 isotype, this antibody did not induce efficient cross-linking of KIR2DS, as demonstrated by the very low increments in the number of IFN-γ+/CD107+ NK cells when KIR2DS+ donors were stimulated with 1-7F9 antibody. Moreover, the ability to bind KIR2DS does not appear to impact the capacity of 1-7F9 to bind or block inhibitory KIR2DL receptors, or to augment activation of KIR2DL-positive NK cells, because we consistently observed increased NK-mediated killing of HLA-C–positive target cells in the presence of 1-7F9, regardless of KIR2DS expression. A proportion of healthy people lack the genes encoding KIR2DS1 and -2,40 yet have NK cells that appear functionally normal. In addition, all people harbor subsets of NK cells that express inhibitory KIR2DL receptors without coexpressing the activating KIR2DS1 and -2 molecules,12 suggesting that expression of KIR2DS1 and -2 is not required for activation of NK-cell cytotoxicity, nor for the function of KIR2DLs.
It is well established that anti-KIR antibodies may augment killing of tumor cells by IL-2–activated NK cells.23 However, certain types of target cells appeared unable to induce killing by resting NK cells, despite robust killing by cytokine-stimulated NK cells.36 Furthermore, it has been suggested that NK cells derived from AML patients are functionally impaired,41 perhaps due to tumor- and/or chemotherapy-mediated suppression.42 Therefore, it was important to test whether patient-derived, resting NK cells may kill autologous AML blasts. Hence, we collected tumor cells at diagnosis, and tested their capacity to activate NK cells isolated from the same patient at least 6 weeks after the last chemotherapy, to allow time for reconstitution of the NK compartment. Under these conditions, 1-7F9 mAb augmented AML blast-induced activation of NK cells, as detected by a flow cytometric cytotoxicity assay, and by granzyme B release measured by an ELISPOT assay. The 1-7F9 mAb did not induce NK activation in the absence of AML target cells, suggesting that NK cells do not rely on recognition of HLA-C for tolerance to each other. Furthermore, addition of 1-7F9 to PBMC or to whole blood of normal donors also did not result in detectable NK-cell activation, measured by expression of CD107 or IFN-γ. These results are consistent with the possibility that normal, healthy cells may express insufficient levels of activating ligands to allow for NK activation, even when KIR is blocked.43 In contrast, addition of HLA class I–negative K562 target cells resulted in significant NK-cell activation, as did primary AML blasts in the presence of 1-7F9 mAb–mediating KIR blockade. Transformed cells, therefore, appear to deliver activation signals to NK cells that may not be provided by normal PBMC. Taken together, our results indicate that blocking of KIR by 1-7F9 antibody may augment tumor-mediated triggering of resting NK cells, without breaking tolerance to normal, healthy hematopoietic cells. Consistent with these findings, alloreactive, KIR ligand-mismatched NK cell–mediated antileukemia responses were not associated with graft-versus-host disease or other signs of NK-cell aggression toward healthy tissues in AML patients receiving SCT or infusion of NK cells.14,44,45
KIRs are not conserved in mice, which instead use a family of inhibitory Ly49 receptors for recognition of MHC class I allotypes on target cells. Therefore, the capacity of 1-7F9 mAb to augment NK-cell activation in vivo was tested by 2 approaches involving humanized mice. First, we developed mouse strain mice expressing a KIR2DL3 transgene on a Rag−/− background, which lack B and T cells. In these mice, 1-7F9 dose dependently induced rejection of HLA-Cw3+/+, KbDb−/− splenocytes. The degree of rejection correlated well with KIR occupancy by the antibody. It should be noted that in this model, clinical grade antibody alone, carefully checked for absence of endotoxin, is sufficient to induce rejection of HLA-Cw3–positive cells without the addition of exogenous cytokine. Remarkably, no depletion of NK cells was detected in these experiments, even after long exposure to 1-7F9, consistent with the in vitro data.
The in vivo efficacy of 1-7F9 was further evaluated in a NOD-SCID mouse model of NK-mediated rejection of transformed B cells. Inoculation of transformed human B cells together with autologous NK cells resulted in a high rate of mortality. A single injection of 1-7F9 was sufficient to rescue the mice, resulting in long-term survival. Similarly, preincubation ex vivo of the NK cells with 1-7F9 before inoculation was sufficient to induce elimination of the autologous tumor cells in vivo. These results indicate that 1-7F9 significantly augmented tumor killing in vivo. In these experiments, however, the NK cells were grown in vitro in IL-2 before inoculation into the mice. Evidence that antibody-mediated masking of inhibitory receptors alone may be sufficient to induce activation of resting NK cells came from the in vitro assays with human NK cells and autologous AML blasts, and from our KIR2DL3tg model described above. Furthermore, in wild-type mice, injection of an anti-Ly49 antibody conferred resistance to a lethal dose of syngeneic lymphoma cells.46
The results described in this study indicate that 1-7F9 is capable of increasing natural cytotoxicity, as well as rituximab-induced ADCC, toward AML blasts or transformed B cells, respectively, and that it does not induce activation of NK cells in the presence of normal cells alone. Thus, our results suggest promise for the use of 1-7F9 antibody to block inhibitory KIR2DLs therapeutically. Based on these data, phase 1 trials are now under way with 1-7F9 in patients with AML and multiple myeloma.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank David Baltimore (California Institute of Technology, Pasadena, CA) and Peter Parham (Stanford University, Stanford, CA) for the gifts of YTS-2DL1 and .221 transfectants, respectively. We acknowledge the technical assistance of staff at Innate-Pharma and Novo Nordisk.
This work was supported by National Cancer Institute (NCI)/National Institutes of Health (NIH; Bethesda, MD) PO1 CA95426-01 and NCI/NIH R01 CA68458-08 to M.A.C. L.R. and A.V. are supported by a Translational Research Grant and Special Fellowship in Clinical Research from the Leukemia & Lymphoma Society (White Plains, NY), and by grants from Italian Association for Cancer Research, Italian Ministry of Further Education, Italian Ministry of Health, European Community (Contract LSHB-CT-2004-503319), and NIH (Project 1 PO1 CA100265). A.M. is supported by grants awarded by Associazione Italiana per la Ricerca sul Cancro, Istituto Superiore di Sanità, Ministero della Sanità, Ministero dell'Istruzione, dell'Università e della Ricerca Scientifica e Tecnologica; E.V. is supported by European Union FP6, LSHB-CT-2004-503319-Allostem, Ligue Nationale contre le Cancer ('Equipe labellisée La Ligue'), Agence Nationale de la Recherche, Institut National du Cancer, Inserm, CNRS, and Ministère de l'Enseignement Supérieur et de la Recherche. E.V. is a scholar of the Institut Universitaire de France.
National Institutes of Health
Authorship
Contribution: F.R. and N.W. designed research, interpreted data, and wrote the paper; P.A., P.S., N.A., L.R., and D.M.B. designed and performed research, interpreted data, and revised the manuscript; S.Z., L.G., and B.W.B. designed and performed research and interpreted data; M.C. and M.D.C. performed research and interpreted data; and A.M., E.V., M.A.C., and A.V. designed and supervised research, interpreted data, and revised the manuscript.
Conflict-of-interest disclosure: A.M. and E.V. are founders and shareholders of and F.R., P.A., N.A., and L.G. are employees of Innate-Pharma. P.S., S.Z., and N.W. are employees and shareholders of Novo Nordisk. The remaining authors declare no competing financial interests.
Correspondence: Nicolai Wagtmann, Biopharmaceuticals Research Unit, Novo Nordisk R&D, Novo Nordisk Park, G8.1.21, DK-2760 Maaloev, Denmark; e-mail: wagt@novonordisk.com.
Requests for reagents: Francois Romagné, Innate-Pharma SA, 117 Avenue Leon Lachamps, 13009 Marseille, France; e-mail: Francois.romagne@innate-pharma.fr.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal