Heparan sulfate binds to and regulates many inflammatory mediators in vitro, suggesting that it serves an important role in directing the progression and outcome of inflammatory responses in vivo. Here, we evaluated the role of syndecan-1, a major heparan sulfate proteoglycan, in modulating multiorgan host injury responses in murine endotoxemia. The extent of systemic inflammation was similar between endotoxemic syndecan-1–null and wild-type mice. However, high levels of CXC chemokines (KC and MIP-2), particularly at later times after LPS, were specifically sustained in multiple organs in syndecan-1–null mice and associated with exaggerated neutrophilic inflammation, organ damage, and lethality. Syndecan-1 shedding was activated in several organs of endotoxemic wild-type mice, and this associated closely with the removal of tissue-bound CXC chemokines and resolution of accumulated neutrophils. Moreover, administration of a shedding inhibitor exacerbated disease by impeding the removal of CXC chemokines and neutrophils, whereas administration of heparan sulfate inhibited the accumulation of CXC chemokines and neutrophils in tissues and attenuated multiorgan injury and lethality. These data show that syndecan-1 shedding is a critical endogenous mechanism that facilitates the resolution of neutrophilic inflammation by aiding the clearance of proinflammatory chemokines in a heparan sulfate–dependent manner.
Introduction
A properly regulated inflammatory response protects the host from infection and aids in restoring the structure and function of damaged tissues after injury. However, severe or persistent inflammation can lead to many serious acute and chronic diseases, such as systemic inflammatory response syndrome, acute lung injury, inflammatory bowel disease, atherosclerosis, and many more. Irrespective of the affected organ, dysregulated inflammation can lead to organ damage, dysfunction, and failure. In a typical controlled inflammatory response, an inductive phase is followed by a sustained response, which declines and ends when the processes triggered by the initial responses are halted. Thus, correct coordination and timely resolution of the inflammatory response are critical in maintaining the balance between health and disease. However, although mechanisms instigating and perpetuating inflammatory responses have been studied extensively, less is known about the mechanisms governing the resolution of inflammation.
Heparan sulfate (HS) and its pharmaceutical functional analog, heparin, bind to and regulate many inflammatory factors in vitro.1,2 HS and heparin are linear polysaccharides composed of repeating disaccharide units of hexuronic acid, either glucuronic or iduronic acid, alternating with unsubstituted or N-substituted glucosamine on which the substituents are either acetate or sulfate.1,2 Heparin possesses anti-inflammatory activities in several human inflammatory diseases, such as asthma3 and inflammatory bowel disease.4 Clinical studies also show that low-dose heparin increases the odds of survival in patients with sepsis,5 suggesting that heparin inhibits the deleterious consequences of dysregulated inflammation. However, heparin apparently does not attenuate inflammation through its anticoagulant activities.3,6 Native heparin is found in intracellular vesicles of mast cells, whereas HS is ubiquitously expressed on the surface of cells and in the extracellular matrix. Because HS contains all of the structural motifs present in heparin and all HS in vivo are found covalently conjugated to specific core proteins as HS proteoglycans (HSPGs), the physiologic counterpart of pharmaceutical heparin is probably HS.
The syndecan family of type I transmembrane HSPGs, comprising 4 members in mammals (syndecan-1 through -4), is the major source of cell surface HS.1,7 Although all syndecans contain the ligand-binding HS chains, they are expressed on different cell types and different locations and, hence, perform specific functions in vivo.1,8 For example, syndecan-1 is predominantly expressed by epithelial cells, although it is also expressed by other cell types to a lesser degree (eg, endothelial cells). Syndecans function as coreceptors by capturing HS-binding ligands and increasing ligand concentration in the pericellular vicinity of their respective signaling receptors.1,7
In response to injury or infection, the ectodomain of syndecan-1 is proteolytically shed from the cell surface by metalloproteinases, enabling syndecan-1 to also function as soluble HSPGs.1,7 Several inflammatory mediators enhance syndecan-1 shedding in vitro,9,,,–13 and certain pathologic conditions induce shedding in vivo.14,,,,,–20 In humans, syndecan-1 ectodomains are detected in skin wound fluids, tracheal aspirates of intubated preterm infants, and blood of patients with acute graft-versus-host disease or myeloma.13,15,19,21 In mice, elevated levels of syndecan-1 ectodomains are found in lungs of mice challenged with Pseudomonas aeruginosa,17 Staphylococcus aureus β-toxin,22 bleomycin16 or allergens,18 and in blood of mice challenged with Gram-positive superantigens.20 Results from these studies suggest that syndecan-1 shedding protects the host from dysregulated inflammation. For example, in the mouse model of allergic lung inflammation, intranasal inoculation of allergens stimulates airway syndecan-1 shedding, and syndecan-1 ectodomain attenuates lung inflammation by inhibiting T helper type 2 cell homing to the lung.18 Consistent with this mechanism, allergen-instilled syndecan-1–null (Sdc1−/−) mice show exaggerated lung inflammation relative to wild-type (WT) mice. These observations suggest that syndecan-1 shedding is an important host response that assures the adequate and correct functioning of inflammatory processes, but the underlying mechanisms have remained elusive.
In the present study, we show that syndecan-1 facilitates the resolution of neutrophilic inflammation in a mouse model of endotoxemia. Syndecan-1 does not affect the systemic or local expression of inflammatory factors, but it specifically facilitates the removal of the CXC chemokines, KC (CXCL1, an IL-8 ortholog) and MIP-2 (CXCL2), in multiple organs. Further, we show that syndecan-1 shedding is induced at later times after LPS infusion, and inhibition of shedding interferes with the removal of KC and MIP-2 and resolution of neutrophilic inflammation in various organs. In contrast, HS infusion improves survival by inhibiting the sequestration of KC and MIP-2, tissue neutrophilia, and multiorgan injury. These data uncover a previously unknown mechanism that facilitates the resolution of neutrophilic inflammation.
Methods
Reagents
Escherichia coli O111:B4 LPS was purchased from Calbiochem. Rat anti–mouse GR-1 (clone RBC6-8C5) and rat anti–mouse CD14 (159010) monoclonal antibodies were from R&D Systems, rat anti–mouse syndecan-1 (281-2) monoclonal antibodies were from BD Pharmingen, rat anti–mouse syndecan-4 (Ky8.2) monoclonal antibodies were from Dr Paul Kincade (Oklahoma Medical Research Foundation), rabbit anti–cleaved caspase 3 monoclonal antibodies were from Cell Signaling, and Alexa 594 donkey anti–rat and Alexa 488 goat anti–rabbit antibodies were from Invitrogen. Bovine kidney HS was from MP Biomedicals, red blood cell lysis buffer was from Sigma-Aldrich, and GM6001 was from Millipore.
Mouse model of endotoxemia
Unchallenged Sdc1−/− mice are healthy with normal growth, reproduction, tissue morphology, complete blood cell (CBC) counts, and serum chemistry parameters.17,23 Sdc1−/− mice on the C57BL/6J background and littermate WT mice were used at an age of 6 to 9 weeks. Mice were injected intraperitoneally with LPS, GM6001, or HS in 100 μL sterile saline at the indicated doses. All animal experiments were approved by the Institutional Animal Care and Use Committee of Children's Hospital, Harvard Medical School, and complied with federal guidelines for research with experimental animals.
Protein assays
Serum was prepared from blood collected by cardiac puncture. Tissues were weighed and homogenized. Cytokines and chemokines in serum and tissue homogenates were measured by enzyme-linked immunoabsorbent assay (ELISA; R&D Systems). Plasma, prepared from citrate-anticoagulated blood, was used to measure circulating levels of the thrombin-antithrombin III (TAT) complex by ELISA (Dade Behring Inc) and activated partial thromboplastin time with the use of a kit from Trinity Biotech. Organ injury and dysfunction markers were measured with the use of an automated Cobas Integra 400 Plus serum chemistry analyzer. CBC analysis was performed with the use of the Bayer Advia 120 hematology analyzer.
Reverse transcription polymerase chain reaction
Total RNA (200 ng) was reverse-transcribed and amplified with the use of the Superscript One-Step reverse transcription polymerase chain reaction kit (Invitrogen). The primers used were 5′-TTC TCT GTG CAG CGC TGC TG-3′ (sense) and 5′-GGA GCT TCA GGG TCA GGC AA-3′ (antisense) for KC, 5′-TGC CGG CTC CTC AGT GC-3′ (sense) and 5′-TTA GCC TTG CCT TTG TTC AGT ATC-3′ (antisense) for MIP-2, and 5′-GTG GGC CGC CCT AGG CAC CAA-3′ (sense) and 5′-CTC TTT GAT GTC ACG CAC GAT TTC-3′ (antisense) for β-actin.
Splenocytes
Splenocytes were prepared by straining isolated spleens through 70-μm screens (Falcon) and lysing erythrocytes in red blood cell lysis buffer. Splenocytes were suspended in RPMI with 10% FCS, and 2 × 107 cells were cultured for 2 hours in 24-well plates. Nonadherent cells were washed away, and adherent splenocytes (∼ 106 cells/well) were incubated with 100 ng/mL LPS for 24 hours at 37°C.
Histology
WT and Sdc1−/− tissues were isolated at various times after LPS, fixed in 4% paraformaldehyde/PBS for 2 days at 4°C, embedded in paraffin, and sectioned. Tissue sections (5 μm) were stained with hematoxylin-eosin or immunostained with anti–mouse GR1, 281-2 anti–mouse syndecan-1 ectodomain, anti–mouse CD14, or anticleaved caspase-3 antibodies and Alexa 594 anti–rat or Alexa 488 anti–rabbit antibodies. Stained tissues were visualized with the Nikon Eclipse 80i microscope (20×/0.75 NA) and pictures were taken with the Nikon DS-2MBWc camera using Prolong gold anti-fade reagent (Invitrogen) and Nikon NIS-elements image-acquistion software (Version 2.30). Photoshop CS2 (Adobe Systems) was used to process the acquired images.
Syndecan shedding assay
Serum levels of syndecan-1 and -4 ectodomains were assessed by a dot immunoblot assay as described previously.11,12 Briefly, 10 to 50 μL of serum collected at various times after LPS was diluted in TBS and dot blotted onto a cationic nylon membrane (Immobilon Ny+; Millipore), and the concentration of shed ectodomains was quantified with 281-2 anti–syndecan-1 or Ky8.2 anti–syndecan-4 ectodomain antibodies.
Statistical analyses
All data are expressed as mean plus or minus SE. Differences between experimental groups and respective controls were examined by Student t test, and differences in survival values were compared by Fisher exact test. P values of less than .05 were considered statistically significant.
Results
Sdc1−/− mice are susceptible to LPS-induced multiorgan injury and lethal endotoxemia
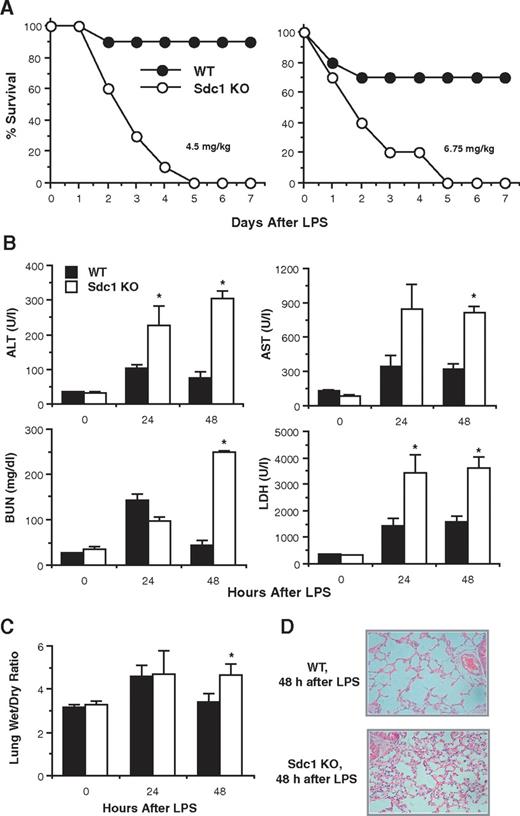
We first tracked the survival of WT and Sdc1−/− mice injected intraperitoneally with various doses of LPS. Only 10% or 30% of WT mice died, and only within the first 2 days, during the course of a 7-day experiment in response to 4.5 or 6.75 mg LPS/kg, respectively (Figure 1A). However, all Sdc1−/− mice died by 5 days after LPS at both doses (Figure 1A). Both WT and Sdc1−/− mice showed similar signs of distress (eg, decreased mobility, shivering, hunched stature) starting at approximately 15 to 20 hours after LPS. WT mice that survived started to show external signs of recovery at approximately 40 to 48 hours after LPS, but Sdc1−/− mice remained distressed and morbid. These observations indicate that the potentially lethal responses to LPS are exacerbated in the absence of syndecan-1 and suggest that syndecan-1 attenuates the dysregulated inflammatory response to LPS.
Sdc1−/− mice are susceptible to LPS-induced multiorgan injury and dysfunction and lethal endotoxemia. (A) WT and Sdc1−/− mice were injected intraperitoneally with 4.5 or 6.75 mg LPS/kg, and their survival was tracked for 7 days (n = 10 in each group; P < .05 at ≥ 3 days after LPS at both LPS doses). At a higher dose of LPS (15 mg/kg), all WT and Sdc1−/− mice died by 3 days after LPS, whereas at a lower dose (2.25 mg/kg), all WT and Sdc1−/− mice survived (not shown). (B) WT and Sdc1−/− mice were injected with LPS (4.5 mg/kg) and serum levels of ALT, AST, BUN, and LDH were measured at 0, 24, and 48 hours after LPS by a serum chemistry analyzer (Cobas Integra 400 Plus serum chemistry analyzer). Results shown are mean ± SE (n = 5; *P < .05 relative to WT mice). (C) WT and Sdc1−/− mice were injected with LPS, and the lung wet/dry ratio was determined at the indicated times by weighing lungs before and after incubation at 90°C for 3 days (n = 5). (D) Paraffin-embedded tissues sections (5 μm) of WT and Sdc1−/− lungs harvested at 48 hours after LPS were stained with hematoxylin-eosin (original magnification, ×200). Error bars indicate SE.
Sdc1−/− mice are susceptible to LPS-induced multiorgan injury and dysfunction and lethal endotoxemia. (A) WT and Sdc1−/− mice were injected intraperitoneally with 4.5 or 6.75 mg LPS/kg, and their survival was tracked for 7 days (n = 10 in each group; P < .05 at ≥ 3 days after LPS at both LPS doses). At a higher dose of LPS (15 mg/kg), all WT and Sdc1−/− mice died by 3 days after LPS, whereas at a lower dose (2.25 mg/kg), all WT and Sdc1−/− mice survived (not shown). (B) WT and Sdc1−/− mice were injected with LPS (4.5 mg/kg) and serum levels of ALT, AST, BUN, and LDH were measured at 0, 24, and 48 hours after LPS by a serum chemistry analyzer (Cobas Integra 400 Plus serum chemistry analyzer). Results shown are mean ± SE (n = 5; *P < .05 relative to WT mice). (C) WT and Sdc1−/− mice were injected with LPS, and the lung wet/dry ratio was determined at the indicated times by weighing lungs before and after incubation at 90°C for 3 days (n = 5). (D) Paraffin-embedded tissues sections (5 μm) of WT and Sdc1−/− lungs harvested at 48 hours after LPS were stained with hematoxylin-eosin (original magnification, ×200). Error bars indicate SE.
Next, we assessed the extent of multiorgan injury and dysfunction by measuring serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), blood urea nitrogen (BUN), and lactic dehydrogenase (LDH). We also measured the lung wet/dry ratio as an indicator of pulmonary edema and assessed lung injury by histology. We used 4.5 mg LPS/kg in this and subsequent experiments, a lethal dose for Sdc1−/− mice but a sublethal dose for WT mice. Starting at 24 hours after LPS, Sdc1−/− mice exhibited elevated levels of organ dysfunction markers compared with WT mice, and, by 48 hours after LPS, serum levels of ALT (4-fold), AST (3-fold), BUN (6-fold), and LDH (2-fold) were significantly increased in Sdc1−/− mice relative to WT mice (Figure 1B). Further, at 48 hours after LPS, Sdc1−/− mice showed significantly increased lung wet/dry ratio and histologic evidence of lung injury with increased infiltration of leukocytes relative to WT mice (Figure 1C-D). These data indicate that LPS-induced multiorgan injury and dysfunction are exacerbated in the absence of syndecan-1 and suggest that multiorgan failure is the cause of increased mortality in endotoxemic Sdc1−/− mice.
Removal of tissue-associated KC and MIP-2 is inhibited in endotoxemic Sdc1−/− mice
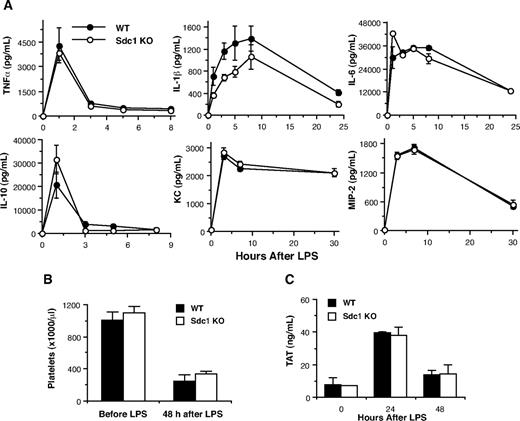
To determine the underlying cause of the exaggerated host response to LPS in Sdc1−/− mice, we tested if syndecan-1 binds to and neutralizes LPS. Radiolabeled syndecan-1 did not bind to LPS by ligand blotting, and LPS did not bind to heparin by affinity chromatography (not shown). We next examined the systemic inflammatory response in endotoxemic Sdc1−/− mice. Increased and decreased systemic levels of proinflammatory and anti-inflammatory factors, respectively, are thought to lead to the development of multiorgan dysfunction and failure in systemic inflammatory response syndrome.24 However, no significant differences in serum levels of the proinflammatory factors, TNFα, IL-1β, IL-6, KC, or MIP-2, or the anti-inflammatory cytokine IL-10 were found between genotypes (Figure 2A). Similarly, serum levels of IFN-γ, FasL, TGFβ1, G-CSF, and IL-1RA increased at different times after LPS administration but did not differ between genotypes (not shown). These data indicate that syndecan-1 deficiency does not affect the systemic inflammatory response to LPS challenge.
Endotoxemic WT and Sdc1−/− mice show similar systemic inflammatory and hemostatic responses. Mice were injected with LPS, and (A) serum levels of TNFα, IL-1β, IL-6, IL-10, KC, and MIP-2 were determined by ELISA at the indicated times after LPS (n = 5), (B) circulating platelets were measured by CBC analysis before and 48 hours after LPS (n = 3; Bayer Advia 120 hematology analyzer), and (C) plasma TAT levels were determined by ELISA at the indicated times after LPS (n = 4). Error bars indicate SE.
Endotoxemic WT and Sdc1−/− mice show similar systemic inflammatory and hemostatic responses. Mice were injected with LPS, and (A) serum levels of TNFα, IL-1β, IL-6, IL-10, KC, and MIP-2 were determined by ELISA at the indicated times after LPS (n = 5), (B) circulating platelets were measured by CBC analysis before and 48 hours after LPS (n = 3; Bayer Advia 120 hematology analyzer), and (C) plasma TAT levels were determined by ELISA at the indicated times after LPS (n = 4). Error bars indicate SE.
We also examined if aberrant hemostatic responses were associated with the enhanced host responses in endotoxemic Sdc1−/− mice. LPS activates systemic coagulation and disseminated intravascular coagulation,25 and some consider cell surface HSPGs as endogenous heparin-like molecules that maintain an anticoagulant state in the vasculature.26,27 Both WT and Sdc1−/− mice showed similar extent of thrombocytopenia at 48 hours after LPS (Figure 2B). Further, plasma levels of the TAT complex (Figure 2C) and the activated partial thromboplastin time (not shown) were similar between endotoxemic WT and Sdc1−/− mice. These data suggest that syndecan-1 does not affect the hemostatic responses in murine endotoxemia.
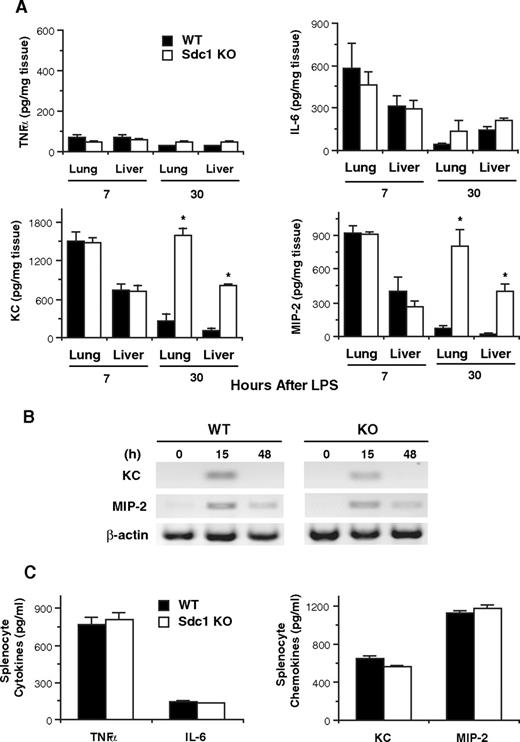
We next examined if the local inflammatory response to LPS is dysregulated in Sdc1−/− mice. Lungs and livers from WT and Sdc1−/− mice were harvested at 7 and 30 hours after LPS, and TNFα, IL-6, KC, and MIP-2 levels in tissue homogenates were measured by ELISA (Figure 3A). Tissue levels of TNFα and IL-6 were similar between endotoxemic WT and Sdc1−/− mice. Similarly, tissue levels of KC and MIP-2 were markedly elevated at 7 hours after LPS in both genotypes. However, although both KC and MIP-2 returned to baseline by 30 hours after LPS in WT mice, they remained significantly elevated in endotoxemic Sdc1−/− mice. At 30 hours after LPS, lung and liver levels of KC were 6- and 8-fold higher, and those of MIP-2 were 11- and 19-fold higher in Sdc1−/− mice than those in WT mice (Figure 3A).
Removal of tissue-associated KC and MIP-2 is impeded in endotoxemic Sdc1−/− mice. (A) WT and Sdc1−/− mice were injected with LPS, and their lungs and livers were harvested at 7 or 30 hours after LPS. Tissues were weighed and homogenized, and tissue levels of TNFα, IL-6, KC, and MIP-2 were determined by ELISA (n = 5; *P < .05 relative to WT mice at the indicated time). (B) Total RNA was isolated from WT and Sdc1−/− lungs at 0, 15, and 48 hours after LPS infusion, and KC, MIP-2, and β-actin mRNA was assessed by reverse transcription polymerase chain reaction. (C) WT or Sdc1−/− splenocytes were stimulated with 100 ng LPS/mL for 24 hours at 37°C, and the concentration of TNFα, IL-6, KC, and MIP-2 in the conditioned medium was determined by ELISA (n = 4). Error bars indicate SE.
Removal of tissue-associated KC and MIP-2 is impeded in endotoxemic Sdc1−/− mice. (A) WT and Sdc1−/− mice were injected with LPS, and their lungs and livers were harvested at 7 or 30 hours after LPS. Tissues were weighed and homogenized, and tissue levels of TNFα, IL-6, KC, and MIP-2 were determined by ELISA (n = 5; *P < .05 relative to WT mice at the indicated time). (B) Total RNA was isolated from WT and Sdc1−/− lungs at 0, 15, and 48 hours after LPS infusion, and KC, MIP-2, and β-actin mRNA was assessed by reverse transcription polymerase chain reaction. (C) WT or Sdc1−/− splenocytes were stimulated with 100 ng LPS/mL for 24 hours at 37°C, and the concentration of TNFα, IL-6, KC, and MIP-2 in the conditioned medium was determined by ELISA (n = 4). Error bars indicate SE.
To assess if sustained high levels of tissue KC and MIP-2 were due to continued production, we measured mRNA levels of these chemokines in LPS-injected WT and Sdc1−/− tissues. Lung KC and MIP-2 mRNA were similarly increased at 15 hours after LPS and dropped to near basal levels by 48 hours after LPS in both genotypes (Figure 3B). Similar results were obtained with WT and Sdc1−/− liver (not shown). We examined if Sdc1−/− cells produce higher amounts of KC and MIP-2 in response to LPS. WT and Sdc1−/− splenocytes were stimulated with LPS, and TNFα, IL-6, KC, and MIP-2 in the conditioned medium were measured. Both WT and Sdc1−/− splenocytes produced similar levels of cytokines and chemokines in response to LPS (Figure 3C). Together, these data indicate that the sustained high levels of KC and MIP-2 in Sdc1−/− tissues are not due to increased production. Instead, these results indicate that syndecan-1 facilitates the clearance of KC and MIP-2 in tissues during the resolution of inflammation, and the absence of syndecan-1 impedes this process in endotoxemic Sdc1−/− mice.
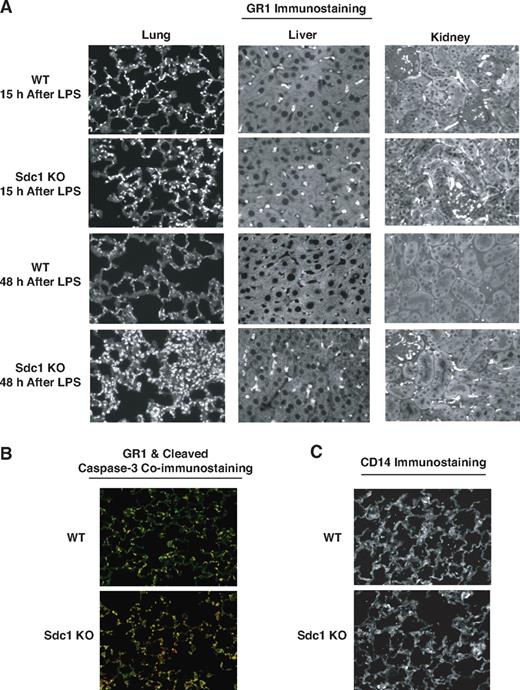
Resolution of neutrophilic inflammation is impeded in endotoxemic Sdc1−/− mice
A key event during an inflammatory response is the recruitment of leukocytes to the site of injury, immune response, or infection. KC and MIP-2 are the major CXC chemokines that provide chemotactic signals for neutrophil infiltration.28,29 Neutrophils are typically the first type of leukocytes recruited to sites of infection and injury. Although an essential arm of innate immunity, several studies have implicated neutrophils in contributing greatly to tissue damage associated with dysregulated inflammation.30,31 Thus, we assessed if increased tissue levels of KC and MIP-2 led to exaggerated neutrophil accumulation in endotoxemic Sdc1−/− mice. Lung, liver, and kidney harvested from WT and Sdc1−/− mice at 15 and 48 hours after LPS were immunostained for GR1, a mouse neutrophil-specific antigen. At 15 hours after LPS, abundant GR1-positive neutrophils were seen within the lung alveolar walls, in the liver interstitium and microcapillaries, and in the kidney interstitium and glomeruli in both WT and Sdc1−/− mice (Figure 4A). These findings indicate that syndecan-1 deficiency does not affect the initial accumulation of neutrophils and are consistent with similar tissue levels of KC and MIP-2 at earlier times after LPS in WT and Sdc1−/− mice (Figure 3A). At 48 hours after LPS, sparse anti-GR1 staining was seen in WT organs, indicating that the signals for neutrophil influx have been removed, neutrophil infiltration has been halted, and infiltrated neutrophils have been cleared (Figure 4A). However, a large number of neutrophils remained in Sdc1−/− organs at 48 hours after LPS (Figure 4A). In fact, neutrophils increased in Sdc1−/− lungs at 48 hours after LPS relative to 15 hours after LPS. Similar results were obtained when the extent of neutrophil accumulation was assessed by fluorescence-activated cell sorting (FACS) analysis of lung and liver cells (not shown). Coimmunostaining with anti-GR1 and anti–cleaved caspase-3 showed that the extent of neutrophil apoptosis was similar in WT and Sdc1−/− lungs at 24 after LPS (Figure 4B). FACS analysis of lung cells with anti-Ly6G and anti–cleaved caspase-3 also showed that a similar proportion of apoptotic neutrophils were present in WT and Sdc1−/− lungs at 15 and 48 hours after LPS (not shown). Further, immunostaining with anti-CD14 (Figure 4C) or anti-F4/80 and FACS analysis with anti-CD14 showed that monocyte/macrophage infiltration was also similar between the 2 genotypes (not shown), suggesting that apoptosis of infiltrated neutrophils and their removal by macrophages are normal in endotoxemic Sdc1−/− mice. Together, these results suggest that, whereas neutrophilic inflammation was resolved in WT mice by 48 hours after LPS, an exuberant inflammatory response was sustained in Sdc1−/− mice, most likely because of a deficiency in the removal of KC and MIP-2 in tissues at later times after LPS.
Resolution of neutrophilic inflammation is inhibited in endotoxemic Sdc1−/− mice. (A) WT and Sdc1−/− mice were injected with LPS, and their lungs, livers, and kidneys were isolated at 15 or 48 hours after LPS. Tissue sections were immunostained with the rat anti–mouse GR-1 (Ly6G/C, clone RBC6-8C5) antibody and Alexa 594 donkey anti–rat IgG antibody (original magnification, ×200). Similar results were obtained with the rat anti–mouse Ly6G (1A8) monoclonal antibody (not shown). (B) WT and Sdc1−/− lung sections (24 hours after LPS) were coimmunostained with rabbit anti–cleaved caspase-3 and anti-GR1 antibodies and with Alexa 594 anti–rat and Alexa 488 goat anti–rabbit antibodies (original magnification, ×200). (C) WT and Sdc1−/− lung sections (24 hours after LPS) were immunostained with rat anti-CD14 and Alexa 594 anti–rat antibodies (original magnification, ×200).
Resolution of neutrophilic inflammation is inhibited in endotoxemic Sdc1−/− mice. (A) WT and Sdc1−/− mice were injected with LPS, and their lungs, livers, and kidneys were isolated at 15 or 48 hours after LPS. Tissue sections were immunostained with the rat anti–mouse GR-1 (Ly6G/C, clone RBC6-8C5) antibody and Alexa 594 donkey anti–rat IgG antibody (original magnification, ×200). Similar results were obtained with the rat anti–mouse Ly6G (1A8) monoclonal antibody (not shown). (B) WT and Sdc1−/− lung sections (24 hours after LPS) were coimmunostained with rabbit anti–cleaved caspase-3 and anti-GR1 antibodies and with Alexa 594 anti–rat and Alexa 488 goat anti–rabbit antibodies (original magnification, ×200). (C) WT and Sdc1−/− lung sections (24 hours after LPS) were immunostained with rat anti-CD14 and Alexa 594 anti–rat antibodies (original magnification, ×200).
Syndecan-1 ectodomain shedding is induced in endotoxemic WT mice
On the basis of these data, we propose that syndecan-1 moderates neutrophilic inflammation by facilitating the removal of tissue-associated KC and MIP-2. To begin defining how syndecan-1 functions, we examined the expression of syndecan-1 in endotoxemic WT mice. Tissue sections of WT lung and liver harvested before and after LPS infusion were immunostained with the 281-2 anti–syndecan-1 ectodomain antibody (Figure 5A). Untreated lungs showed strong cell surface syndecan-1 expression in mostly cuboidal type II epithelial cells of alveoli. Untreated livers showed intense 281-2 immunoreactivity on the sinusoidal side of hepatocytes, indicating that syndecan-1 is abundantly expressed on the cell surface of hepatocytes and/or endothelial cells. In contrast, the signal for cell surface syndecan-1 in the lung and liver was significantly reduced at 24 hours after LPS (Figure 5A). Because steady-state syndecan-1 mRNA levels were similar in the lung and liver at 0, 6, and 24 hours after LPS (not shown), the reduced cell surface expression suggested that syndecan-1 ectodomains were shed from various organs in endotoxemic WT mice. Indeed, whereas serum levels of syndecan-1 ectodomains were low in unchallenged WT mice, they increased progressively up to 24 hours after LPS, and high levels were sustained at 48 hours after LPS (Figure 5B). Levels of syndecan-4 ectodomains in serum were also increased at 8 hours after LPS, but, unlike syndecan-1, syndecan-4 quickly dropped to basal levels (Figure 5B). Further, serum syndecan-1 ectodomains were not detected when probed with antibodies directed against the syndecan-1 cytoplasmic domain,11 verifying that syndecan-1 ectodomains were shed and not released from damaged cells (not shown). Interestingly, we found that levels of syndecan-4 ectodomains are increased in LPS-infused Sdc1−/− mice compared with LPS-infused WT mice (Figure 5B). These data indicate that, although syndecan-4 shedding is increased in Sdc1−/− mice, it does not functionally compensate for the loss of syndecan-1 in endotoxemic Sdc1−/− mice, suggesting that syndecan-1 functions specifically in the resolution of neutrophilic inflammation.
Syndecan-1 ectodomains are shed from the cell surface in various organs and released into the circulation in endotoxemic WT mice. (A) WT mice were injected with or without LPS, and their lungs and livers were isolated at 24 hours after LPS. Tissue sections were immunostained with 281-2 rat anti–mouse syndecan-1 ectodomain and Alexa 594 donkey anti–rat IgG antibodies (original magnification, ×200). (B) WT and Sdc1−/− mice were injected with LPS, and serum levels of syndecan-1 and -4 ectodomains were determined at 0, 1, 8, 24, and 48 hours after LPS by dot immunoblotting (n = 5 at each time point). Error bars indicate SE.
Syndecan-1 ectodomains are shed from the cell surface in various organs and released into the circulation in endotoxemic WT mice. (A) WT mice were injected with or without LPS, and their lungs and livers were isolated at 24 hours after LPS. Tissue sections were immunostained with 281-2 rat anti–mouse syndecan-1 ectodomain and Alexa 594 donkey anti–rat IgG antibodies (original magnification, ×200). (B) WT and Sdc1−/− mice were injected with LPS, and serum levels of syndecan-1 and -4 ectodomains were determined at 0, 1, 8, 24, and 48 hours after LPS by dot immunoblotting (n = 5 at each time point). Error bars indicate SE.
Syndecan-1 shedding facilitates the removal of KC and MIP-2 and resolution of neutrophilic inflammation in an HS-dependent manner
Because the induction of syndecan-1 shedding associated closely with the removal of KC and MIP-2 and resolution of tissue neutrophilia, we assessed whether inhibiting syndecan-1 shedding exacerbates neutrophilic inflammation by impeding the removal of KC and MIP-2 in tissues. Syndecan-1 is shed by metalloproteinases16,32,,–35 and, to block its release, WT mice were injected intraperitoneally with GM6001, a broad-acting metalloproteinase inhibitor, or vehicle at 24 hours after LPS. GM6001 was administered in a delayed manner because pretreatment or early administration of GM6001 has been shown to be protective in mouse models of endotoxemia, in part, by inhibiting TACE (ADAM17)–mediated release of TNFα. Thus, GM6001 was administered at 24 hours after LPS, a time point when TNFα release has returned to baseline, when syndecan-1 shedding is maximal, and when tissue-associated KC and MIP-2 are actively removed.
The extent of syndecan-1 shedding was assessed by immunostaining tissue sections for cell surface syndecan-1 and by measuring serum levels of syndecan-1 ectodomains at 40 hours after LPS. Cell surface syndecan-1 levels were higher in the lung and liver of WT mice infused with GM6001 compared with mice that received LPS only (Figure 6A). Further, administration of GM6001 significantly reduced circulating levels of syndecan-1 ectodomains (Figure 6B), indicating that delayed administration of GM6001 inhibited syndecan-1 shedding when neutrophilic inflammation was actively resolved. Importantly, infusion of GM6001 inhibited the removal of KC and MIP-2 and significantly increased chemokine levels in both the lung and liver (Figure 6C). Consistent with these data, GR1-positive neutrophils were also markedly increased in endotoxemic mice that received GM6001 compared with mice that were administered LPS only (Figure 6D). Moreover, whereas only 1 of 10 WT mice that received LPS died, 5 of 9 WT mice that received GM6001 died by 3 days after LPS. Injection of GM6001 without LPS did not increase tissue chemokine mRNA or protein levels, neutrophil accumulation, or mortality (not shown). These results suggest that inhibition of syndecan-1 shedding inhibits the removal of tissue-associated KC and MIP-2 and resolution of neutrophilic inflammation in multiple organs, and it exacerbates disease.
Delayed GM6001 infusion inhibits syndecan-1 shedding, removal of CXC chemokines in tissues, and resolution of neutrophilic inflammation. WT mice were injected intraperitoneally with or without 150 mg GM6001/kg at 24 hours after LPS, and tissue samples were analyzed at 40 hours after LPS. Syndecan-1 shedding was assessed by (A) immunostaining lung and liver sections (original magnification, ×200) and (B) measuring serum levels of syndecan-1 ectodomains (n = 4). (C) Tissue levels of KC and MIP-2 were determined by ELISA (n = 4). (D) Neutrophil accumulation was assessed by immunostaining with anti-GR1 and Alexa 594 anti–rat antibodies (original magnification, ×200). Error bars indicate SE.
Delayed GM6001 infusion inhibits syndecan-1 shedding, removal of CXC chemokines in tissues, and resolution of neutrophilic inflammation. WT mice were injected intraperitoneally with or without 150 mg GM6001/kg at 24 hours after LPS, and tissue samples were analyzed at 40 hours after LPS. Syndecan-1 shedding was assessed by (A) immunostaining lung and liver sections (original magnification, ×200) and (B) measuring serum levels of syndecan-1 ectodomains (n = 4). (C) Tissue levels of KC and MIP-2 were determined by ELISA (n = 4). (D) Neutrophil accumulation was assessed by immunostaining with anti-GR1 and Alexa 594 anti–rat antibodies (original magnification, ×200). Error bars indicate SE.
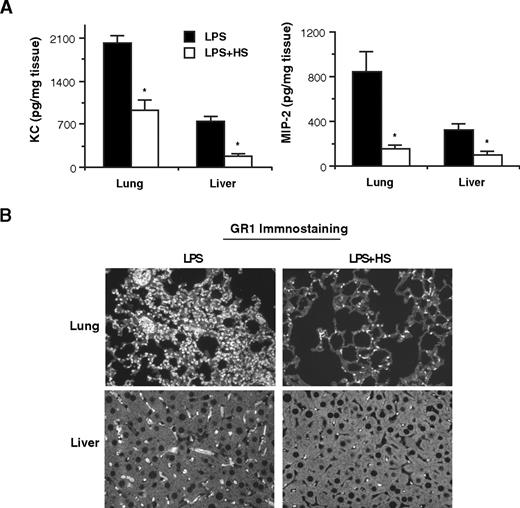
To further define how syndecan-1 resolves neutrophilic inflammation, we examined if administration of HS, the ligand-binding moiety of syndecan-1, will facilitate the removal of tissue-associated KC and MIP-2 and accumulated neutrophils. Sdc1−/− mice were injected with or without HS at 10 hours after LPS, and tissue levels of KC and MIP-2 were measured at 30 hours after LPS. Delayed HS infusion significantly reduced KC and MIP-2 levels in both the lung and liver in endotoxemic Sdc1−/− mice (Figure 7A). Tissue levels of IL-6 and TNFα were not significantly affected (not shown). Consistent with these findings, GR1-positive neutrophils were also markedly reduced in Sdc1−/− mice injected with HS relative to mice injected with LPS only (Figure 7B). Further, all Sdc1−/− mice that were administered LPS only or LPS and syndecan-1 core protein or chondroitin sulfate died by 5 days after LPS, whereas only 10% of mice that received HS died during the course of the experiment (n = 10 in each group). Altogether, these data indicate that syndecan-1 shedding is a critical endogenous mechanism that facilitates the resolution of neutrophilic inflammation by removing tissue-associated KC and MIP-2 in an HS-dependent manner.
Delayed HS administration facilitates the removal of tissue-associated CXC chemokines and resolution of neutrophilic inflammation. (A) Sdc1−/− mice were injected intraperitoneally with or without 50 μg HS/mouse at 10 hours after LPS, and tissue samples were analyzed at 40 hours after LPS. Tissues levels of KC and MIP-2 were determined by ELISA (n = 5). (B) Neutrophil accumulation was assessed by immunostaining with anti-GR1 and Alexa 594 anti–rat antibodies (original magnification, ×200). Error bars indicate SE.
Delayed HS administration facilitates the removal of tissue-associated CXC chemokines and resolution of neutrophilic inflammation. (A) Sdc1−/− mice were injected intraperitoneally with or without 50 μg HS/mouse at 10 hours after LPS, and tissue samples were analyzed at 40 hours after LPS. Tissues levels of KC and MIP-2 were determined by ELISA (n = 5). (B) Neutrophil accumulation was assessed by immunostaining with anti-GR1 and Alexa 594 anti–rat antibodies (original magnification, ×200). Error bars indicate SE.
Discussion
In this study, we report that syndecan-1 attenuates inflammatory tissue injury in endotoxemia by facilitating the removal of KC and MIP-2 and the resolution of neutrophilic inflammation. Our results showed that in mice lacking syndecan-1, LPS infusion leads to sustained high levels of KC, MIP-2, and neutrophils in various organs, overwhelming multiorgan injury and dysfunction, and significantly increased mortality. Because other cell surface HSPGs, including other syndecans, are intact in Sdc1−/− mice, our data show that syndecan-1 specifically functions to control the tissue levels of KC and MIP-2, in turn, preventing continued accumulation of neutrophils. Our data also indicated that syndecan-1 functions more in governing the resolution than in the initial inductive phase of inflammation. In support of this idea, tissue levels of KC, MIP-2, and infiltrated neutrophils were all increased in Sdc1−/− mice relative to WT mice at later times after LPS, but these and other inflammatory parameters were not affected by syndecan-1 deficiency at earlier time points. Although both WT and Sdc1−/− mice showed similar signs of distress soon after LPS infusion, most WT mice recovered, whereas Sdc1−/− mice continued to show signs of distress until their death. Thus, syndecan-1 attenuates the progression or sustainment of inflammatory responses in endotoxemia by facilitating the clearance of tissue-associated KC and MIP-2 and, in turn, accumulated neutrophils.
We also conclude that syndecan-1 shedding facilitates the resolution of neutrophilic inflammation. Whereas systemic inflammation was evident by 1 hour after LPS, elevated levels of syndecan-1 ectodomains were not detected in serum until more than 8 hours after LPS. Importantly, inhibition of shedding by GM6001 at later times after LPS impeded the removal of KC and MIP-2 from various organs and resolution of neutrophilic inflammation in endotoxemic WT mice. GM6001 was administered at 24 hours after LPS because our results indicated that KC and MIP-2 in tissues are removed between 7 and 30 hours after LPS and also because pretreatment or earlier infusion of GM6001 inhibits the shedding of TNFα at earlier times and protects mice from lethal endotoxemia.36 Thus, although metalloproteinase inhibitors of ectodomain shedding may be beneficial if given before the onset of disease or very early, our data indicate that these agents may be detrimental if given at later stages of disease progression. In contrast to delayed GM6001 administration, delayed HS infusion facilitated the removal of KC and MIP-2 and accumulated neutrophils in various organs, attenuated multiorgan injury and dysfunction, and protected mice from lethal endotoxemia. Taken together, these data define the unique manner in which syndecan-1 shedding facilitates the resolution of neutrophilic inflammation by removing sequestered KC and MIP-2 in an HS-dependent manner.
The precise manner in which syndecan-1 shedding facilitates the removal of KC and MIP-2 is not known. This mechanism, however, does not involve an effect on gene expression of KC and MIP-2, suggesting that LPS signaling events through TLR4 are not affected. All chemokines, including KC and MIP-2, bind to cell surface HSPGs through basic amino acid motifs, and this tethering mechanism is essential in preventing dispersion of locally produced soluble chemokines and forming a chemokine gradient to direct leukocyte infiltration to specific sites of tissue injury in vivo.37,38 The specific HSPG(s) that tethers KC and MIP-2 to the cell surface has not been identified, but our results showed that syndecan-1 is abundantly expressed in the liver. We also showed that high levels of syndecan-1 are expressed by type II epithelial cells in the lung, and Walker et al39 showed that neutrophils prefer to extravasate between type II and type I cells. Further, we previously showed that KC binds to syndecan-1 in vivo16 and Marshall et al10 showed that IL-8 binds to cell surface syndecan-1 of endothelial cells to form a chemotactic gradient for neutrophil transendothelial migration in vitro. These observations suggest that cell surface syndecan-1 is the primary docking site for KC and MIP-2, and this tethering mechanism generates a chemotactic gradient for neutrophil infiltration. Thus, when syndecan-1 ectodomains are shed, KC and MIP-2 tethered to cell surface syndecan-1 are displaced, the chemokine gradient dissipates, and neutrophil infiltration is halted, facilitating the resolution of inflammation. Further, because syndecan-1 is expressed in excess of KC and MIP-2, activation of syndecan-1 shedding will also release unbound syndecan-1 ectodomains that can potentially displace KC and MIP-2 tethered to other HSPGs and dissipate the chemokine gradient. Consistent with this mechanism, soluble HS40 and syndecan-1 ectodomains10 have been shown to inhibit IL-8–induced neutrophil migration in vitro. These observations suggest that syndecan-1 shedding facilitates the resolution of neutrophilic inflammation by releasing KC and MIP-2 tethered to cell surface syndecan-1 and by displacing KC and MIP-2 tethered to other cell surface HSPGs through the scavenging activities of syndecan-1 ectodomains.
Alternatively or concurrently, syndecan-1 shedding may also facilitate the resolution of inflammation by removing other sequestered CXC chemokines, such as macrophage migration inhibitory factor and LPS-induced CXC chemokine. Both LPS-induced CXC chemokine and migration inhibitory factor can bind to CXCR2 on neutrophils and have been implicated in neutrophil recruitment in LPS-induced acute lung injury and endotoxic shock.41,–43 Further, syndecan-1 shedding may facilitate neutrophilic inflammation by inhibiting selectin-mediated neutrophil adhesion and migration. Heparin inhibits neutrophil migration by interfering with P- and L-selectin–mediated cell adhesion,6 and endothelial HS is a key ligand for L-selectin–mediated neutrophil adhesion and migration in mouse models of acute peritonitis, contact dermatitis, and cutaneous air-pouch inflammation.44 Thus, syndecan-1 shedding may also inhibit neutrophil infiltration by both rapidly removing the cell surface HS ligand for L-selectin and generating syndecan-1 ectodomains that can inhibit L-selectin–mediated adhesion. Future investigation of the potential functions of syndecan-1 shedding in selectin-mediated neutrophil adhesion and migration may show additional mechanisms of syndecan-1 in the resolution of neutrophilic inflammation.
The pro-resolving activity of exogenous HS suggests that HSPGs other than syndecan-1 can also protect the host from dysregulated neutrophilic inflammation. Indeed, Sdc4−/− mice are also susceptible to lethal endotoxemia compared with WT mice.45 However, several lines of evidence indicate that syndecan-1 and -4 attenuate endotoxemia through distinct mechanisms. First, Sdc4−/− mice are thought to be prone to lethal endotoxemia because of elevated circulating levels of IL-1β. However, our studies showed that circulating levels of IL-1β are similar between endotoxemic Sdc1−/− and WT mice. Second, expression of syndecan-4 was induced in the liver on LPS injection,45 but syndecan-1 mRNA levels were unaffected, and cell surface levels of syndecan-1 were significantly decreased by ectodomain shedding in all tissues examined. Third, the key phenotype we saw in endotoxemic Sdc1−/− mice (sustained high levels of CXC chemokines and neutrophils in multiple organs) was not seen in endotoxemic Sdc4−/− mice. Further, and potentially quite relevant, the kinetics and magnitude of ectodomain shedding of syndecan-1 and syndecan-4 were quite different in WT mice. Whereas syndecan-4 shedding was minimal and transient, syndecan-1 shedding was prominent, and high levels of circulating syndecan-1 ectodomains were sustained even at 48 hours after LPS. Moreover, although syndecan-4 shedding is increased in Sdc1−/− mice, it does not compensate for the loss of syndecan-1 to facilitate the resolution of neutrophilic inflammation in endotoxemic Sdc1−/− mice. Thus, syndecan-1 and syndecan-4 control distinct processes of the inflammatory response in endotoxemia.
Syndecan-1 has also been shown to play a critical modulatory role in several mouse models of inflammatory disorders, such as protein losing enteropathy,46 allergic lung inflammation,18 acute lung injury,16,22 and Gram-positive toxic shock.20 These observations suggest that syndecan-1 shedding is an important process that protects the host from a wide variety of inflammatory disorders. However, how syndecan-1 shedding is induced in vivo is not understood. Several inflammatory factors stimulate syndecan-1 shedding in vitro, including TNFα,47 the primary effector cytokine in endotoxic shock and several other inflammatory diseases. Further, uncontrolled TNFα results in the loss of cell surface syndecan-1 in protein-losing enteropathy,46 and an inverse correlation of TNFα and syndecan-1 expression is observed in the colonic mucosa of patients with Crohn disease,48 suggesting that TNFα may enhance syndecan-1 shedding under pathologic conditions in vivo. In addition, TNFα is a potent inducer of matrix metalloproteinase-7,49 and matrix metalloproteinase-7 is so far the only metalloproteinase that has been shown to shed syndecan-1 ectodomains both in vitro34 and in vivo from the surface of an activated airway epithelium.16 Altogether, these findings suggest that host cells attempt to protect itself from inflammatory tissue damage by sensing proinflammatory factors, such as TNFα, and mobilizing syndecan-1 shedding to facilitate the resolution of inflammation. The capacity of syndecan-1 shedding to facilitate the removal of CXC chemokines and to deactivate neutrophil influx suggests that this is an important mechanism that modulates the progression and outcome of a broad spectrum of acute inflammatory disorders. In addition, because HS can regulate the activity of neutrophil granule proteins that can cause tissue damage,1,50 syndecan-1 may also modulate neutrophil-mediated tissue injury through these HS-dependent activities.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Dr Paul Kincade (Oklahoma Medical Research Foundation, Oklahoma City, OK) for providing the Ky8.2 rat anti–mouse syndecan-4 ectodomain monoclonal antibody.
This work was supported by the National Institutes of Health (grant R01 HL81474; P.W.P.).
National Institutes of Health
Authorship
Contribution: K.H. designed and performed research and wrote the paper; W.C.P. designed experiments and contributed to the writing of the paper; and P.W.P. designed the overall project, performed research, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Pyong Woo Park, Children's Hospital, Harvard Medical School, 320 Longwood Ave, Enders-144, Boston, MA 02115; e-mail: pyong.park@childrens.harvard.edu.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal