Abstract
Abstract 2124
Poster Board II-101
Protein S, a vitamin K-dependent plasma protein, is one of the molecules involved in down-regulation of the coagulation process. Protein S serves as a cofactor of activated protein C (APC) in the proteolytic inactivation of activated factor V and VIII. Protein S is also able to exert its anticoagulant activity independent of APC, e.g. by supporting the anticoagulant activity of tissue factor pathway inhibitor. In plasma, protein S circulates in two forms: a single chain molecule with full anticoagulant activity and a two-chain form with reduced anticoagulant activity. This two-chain variant is the result of cleavage in the protease sensitive loop, the so-called thrombin sensitive region (TSR). The enzyme responsible for the presence of cleaved protein S in the circulation is not known yet. In vitro, thrombin and factor Xa, both enzymes of the coagulation cascade, are able to cleave the TSR. In a recent study (Brinkman et al, J Thromb Haemost 2005; 3: 2712-2720), it was shown that these enzymes do not cleave protein S under physiological conditions. Instead, a platelet protease was found to cleave protein S in plasma during tissue factor induced clotting in vitro. We hypothesize that this platelet protease may be responsible for the presence of cleaved protein S in the circulation.
To correlate cleaved protein S levels in the circulation with the activity of platelet-associated protein S cleaving protease and to evaluate the impact of protein S cleavage on its anticoagulant activity in terms of total protein S activity.
Protein S cleavage was evaluated by immunological methods employing a monoclonal antibody specific for uncleaved, single chain protein S. The total anticoagulant activity of protein S (APC-independent and APC-dependent) was assessed employing thrombography.
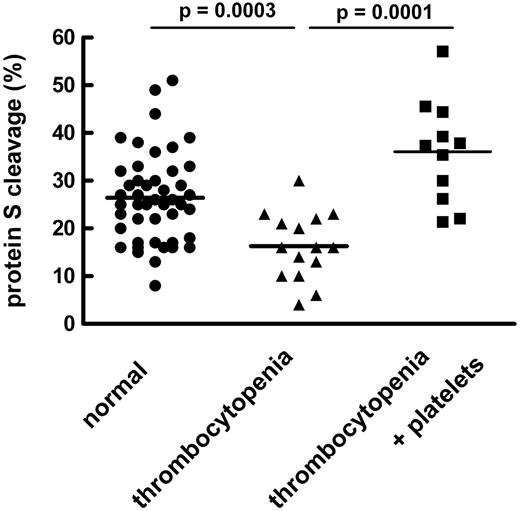
We observed in the in vitro thrombin generation test massive generation of thrombin in protein S deficient plasma that was dose-dependently inhibited by intact, single chain protein S. TSR-cleaved protein S had totally lost its anticoagulant activity. In plasma from healthy volunteers, cleaved protein S expressed as % of the total amount of protein S ranged between 8 and 51% with an average normal value of 26 ± 9% (mean ± SD, n=46). Levels of intact protein S correlated well with total protein S activity in the individual plasma samples, while this correlation was not observed for levels of TSR-cleaved protein S. These data suggest that not only in vitro but also in vivo, cleavage of protein S has an impact on its anticoagulant activity. A significant reduction of levels of cleaved protein S was observed in chemotherapy induced thrombocytopenia in hematological patients (see Figure). At a platelet count < 50, the average protein S cleavage was dropped to 16 ± 7% (mean ± SD, n=15). Upon platelet transfusion, cleavage of protein S dramatically increased to 36 ± 11% (mean ± SD, n=11). Levels of total protein S were similar in healthy volunteers and thrombocytopenic patients before and after platelet transfusion. It thus appears that platelets contribute to protein S cleavage in vivo. However, in healthy individuals showing a wide range of protein S cleavage (see Figure), no correlation was observed between platelet count (200-400 .109/l) and protein S cleavage. This suggests additional sources of protease that cleave protein S in vivo. We therefore examined lysates of a variety of cell types for protein S proteolytic activity. Protein S proteolytic activity was absent in lysates of erytrocytes, vascular smooth muscle cells and fibroblasts. Lysates of HUVEC did show protein S proteolytic activity similar to platelets.
Our results strongly suggest that platelets contribute to the proteolytic modification of protein S in vivo resulting in an abolished anticoagulant activity. An additional source of protein S proteolytic activity may be the endothelium. Cleavage of protein S provoked by platelet infusion may contribute to the beneficial effect of platelet transfusion in the treatment of bleeding episodes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal