Abstract
Abstract 2797
Poster Board II-773
Primary systemic amyloidosis (AL) is characterized by deposition of light chain derived amyloid fibrils in multiple organs leading to varying degree of dysfunction. Cardiac involvement is a common feature of AL, and when significant is highly predictive of poor outcome. The currently used prognostic classification is based on cardiac biomarkers troponin-T (cTnT) and N-terminal pro B-type Natriuretic peptide (NT-ProBNP) and is effective at predicting outcome in patients with AL. However, this is driven primarily by the degree of cardiac involvement and does not take into account the degree of plasma cell burden and its impact on the disease course. It is possible that some of the heterogeneity in outcome can be explained by the plasma cell characteristics rather than the degree of the end organ damage.
We examined the baseline clinical and laboratory data from 2119 patients with AL who were seen at our institution with in 90 days of their diagnosis. The data were collected from a prospectively maintained data base, and additional testing was done for free light chain levels (FLC) on stored sera from patients seen before the routine introduction of FLC testing. Cox proportional hazards analysis was performed to estimate the prognostic values of different variables.
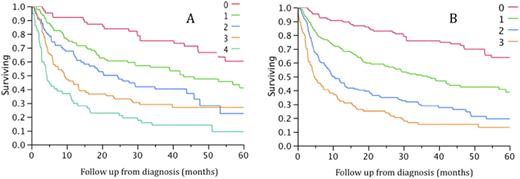
We first examined the impact of plasma cell clone related characteristics namely, difference between involved and uninvolved FLC (FLC-Diff), bone marrow plasma cell (BMPC) %, plasma cell labeling index (PCLI), beta 2 microglobulin (B2M), and presence of circulating plasma cells, on overall survival (OS) from diagnosis. All variables were dichotomized into high and low based on their median value (FLC-diff: 20 mg/dL, BMPC: 10%, PCLI as a continuous variable, B2M: 3 mg/dL and circulating cells: absent or present). While all were found to be prognostic for OS in univariate analysis; in a multivariate analysis incorporating a stepwise selection only B2M and FLC-diff were significant. We then used these two variables along with the cTnT and NT-ProBNP that are used in the current model to develop a staging system. The median values for all four variables were used for developing the scores. Patients were assigned a score of 1 for presence of each characteristic (FLC difference > 20 mg/dL, troponin-T > 0.02, NT-ProBNP > 1000, and B2M > 3) or 0 if the value was at or below the cutoff. The scores were added to obtain a composite prognostic score that grouped the 370 patients (who had all the variables available for analysis) into 5 groups with very different OS (4.4, 9.3, 24.4, 43, and not reached for stages 4, 3, 2, 1, and 0 respectively; Figure A). However, since the NT-ProBNP did not have independent impact on survival in a multivariable model incorporating all the four variables, we also examined a system that only included FLC-diff, cTnT and B2M. This system again allowed grouping of patients (n=450 with all three variables available) into four distinct groups with divergent outcome with OS of 4.6, 10.5, 36.8, and not reached for stages 3, 2, 1, and 0 respectively; (Figure B).
Incorporation of plasma cell related measurements into the existing staging system using cardiac biomarkers allows better risk stratification of patients with AL amyloidosis. The system using FLC, B2M and troponin has the advantage of easily available laboratory values and can be widely adopted. Addition of NT-ProBNP into the system allows better refinement of the intermediate risk groups. This system will allow upfront risk stratification and development of risk-adapted therapies for patients with AL.
Gertz:Genzyme: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal