Abstract
Abstract 443
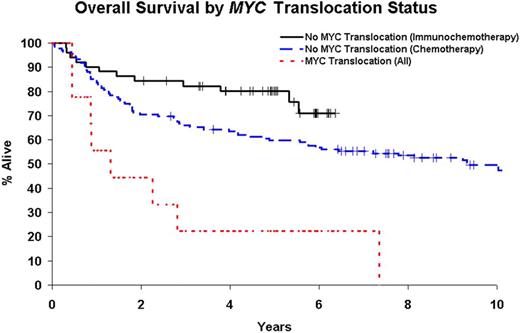
MYC translocations have been reported to have inferior outcome in aggressive non-Hodgkin lymphomas. Here we present MYC translocation prevalence and outcome from two cohorts of newly diagnosed diffuse large B-cell lymphoma (DLBCL) patients treated in the chemotherapy (C) and immunochemotherapy (IC) eras.
Tissue microarrays were created from 302 newly diagnosed DLBCL patients evaluated at the Mayo Clinic with availabel paraffin tissue. 233 DLBCL patients first diagnosed from March 1986-July 2001 were retrospectively identified based on a diagnosis of DLBCL and treatment with anthracycline-based chemotherapy. 69 DLBCL patients diagnosed from March 2002-October 2005 and treated with immunochemotherapy were prospectively enrolled in the University of Iowa / Mayo Clinic Lymphoma SPORE Molecular Epidemiology Resource. Central pathology review was performed on all samples to confirm the diagnosis of DLBCL. Interphase FISH was performed using a breakapart strategy for MYC and BCL6 gene regions and a dual fusion strategy for t(14;18)(IGH&/BCL2).
Chemotherapy (C) era patients were primarily treated with CHOP (88%); immunochemotherapy (IC) era patients were all treated with an R-CHOP based regimen. The median age at diagnosis was 65 years (range, 22-92) for C patients and 65 years (range, 20-82) for IC patients. Median follow-up for C patients was 11.3 years (range, 2.7-21.3) with 145 (62%) deaths; for IC patients, the median follow-up was 5.0 years (range, 2.1-6.4) with 17 deaths (25%). FISH was successful in 195 of 302 patients (65%). MYC translocations were identified in 6 of 141 C patients (4%) and 3 of 54 IC patients (6%). MYC translocations were associated with inferior overall survival in the C patients (p=0.001), the IC patients (p=0.04), and in the combined group (p≤0.001). Median survival of patients with MYC translocations was 19 months and 16 months for C and IC respectively, compared to 112 months (C) and unreached (IC) for DLBCL patients without MYC translocations. 4 of the 9 MYC translocation patients had a double hit (2 with both MYC and BCL2 translocations and 2 with translocations of MYC, BCL2, and BCL6). Associations of MYC and outcome remained significant in all patients after adjusting for treatment and IPI (p<0.05).
MYC translocations are present in approximately 5% of DLBCL patients and are associated with poor outcome in patients treated with C or IC. New treatment approaches are needed for DLBCL patients with MYC translocations.
| . | Chemotherapy Treated Patients (C) . | Immunochemotherapy Treated Patients (IC) . | All Patients . | |||
|---|---|---|---|---|---|---|
| . | N (%) . | OS Hazard Ratio (95% CI) . | N (%) . | OS Hazard Ratio (95% CI) . | N (%) . | OS Hazard Ratio (95% CI) . |
| No MYC translocation | 135 (96%) | 1.00 (reference) | 51 (94%) | 1.00 (reference) | 186 (95%) | 1.00 (reference) |
| MYC translocation | 6 (4%) | 3.74 (1.61, 8.69) | 3 (6%) | 4.42 (0.95, 20.5) | 9 (5%) | 3.67 (1.76, 7.66) |
| . | Chemotherapy Treated Patients (C) . | Immunochemotherapy Treated Patients (IC) . | All Patients . | |||
|---|---|---|---|---|---|---|
| . | N (%) . | OS Hazard Ratio (95% CI) . | N (%) . | OS Hazard Ratio (95% CI) . | N (%) . | OS Hazard Ratio (95% CI) . |
| No MYC translocation | 135 (96%) | 1.00 (reference) | 51 (94%) | 1.00 (reference) | 186 (95%) | 1.00 (reference) |
| MYC translocation | 6 (4%) | 3.74 (1.61, 8.69) | 3 (6%) | 4.42 (0.95, 20.5) | 9 (5%) | 3.67 (1.76, 7.66) |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal