Abstract
Abstract 4685
Hypoalbuminemia (HA) is a strong predictor of poor clinical outcomes in many medical conditions. Low serum albumin levels has been shown to be an adverse prognostic factor in patients with neoplastic diseases such as multiple myeloma, melanoma, and colon cancer. Severe hypoalbuminemia (<3.0 g/dl) at day +90 post allogeneic hematopoietic cell transplant (AHCT) was recently reported as an independent predictive variable for non-relapse mortality and overall survival (Kharfan-Dabaja, et al Biol Blood Marrow Transplant 2009;15). In this retrospective analysis we examined the prognostic value of serum albumin level at baseline, day 14 and day 30 of treatment with salvage chemotherapy regimens for relapsed or refractory AML (RR-AML).
Data were collected retrospectively in a cohort of patients with RR-AML patients who received CLAG (cladribine, cytarabine, and filgrastim) or MEC (mitoxantrone, etoposide, and cytarabine) regimens as salvage chemotherapy. The primary objective was to examine the relationship between serum albumin at baseline, day 14 and day 30 of salvage chemotherapy and probability for achieving complete remission (CR) and overall survival (OS). Patients were divided into two groups; the first group with serum albumin < 3.5 g/dl and the second group patients with serum albumin ≥3.5 g/dl. International Working Group criteria were used to define CR. Primary refractory AML (PR-AML) in this study was defined as failure to achieve CR1 and less than 50% reduction in myeloblasts after first line of induction. All analyses were conducted using SPSS version 15.0. (SPSS Inc, Chicago, IL). The Kaplan–Meier method was used to estimate median overall survival; chi-square test was used for comparison of categorical variables and t-test for continuous variables. Log rank test was used to compare Kaplan–Meier survival estimates between two groups and Cox regression for multivariable analysis.
Between January 2005 and June 2008, 162 patients were treated with CLAG or MEC for RR-AML. Patient baseline characteristics were similar between patients with baseline serum albumin < 3.5 g/dl (HA) and those with serum albumin ≥ 3.5 g/dl (no HA) with respect to sex, FAB subtype, salvage chemotherapy, prior therapy and cytogenetics. Patients with HA were older, mean age 57 years compared to 52 years in non HA group (p=0.039). More patients with HA had prior history of MDS (35.6% versus 19.2%) (p=0.021). Based on baseline serum albumin obtained prior to start of salvage chemotherapy for RR-AML; overall CR rates were HA, 23.8% (19/80) vs. no HA, 41.2% (28/68) (p= 0.033). Median OS was 4.3 months for HA group vs. 8.07 months for no HA, p=0.028.
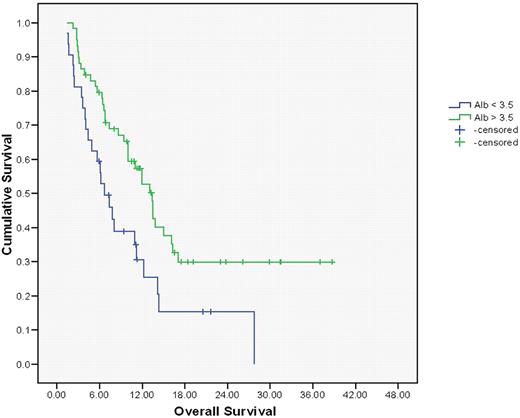
Serum albumin at day 14 of salvage chemotherapy also correlated with OS. The CR was 38.5% for no HA and 27.1% for HA (p=0.12), median OS was 10.0 mo for no HA group versus 4.8 month (p=0.046). Serum albumin at day 30 of salvage chemotherapy was significantly correlated with survival as well with a median OS for HA group was 6.7 month compared to 13.44 month for no HA group (p=0.008).(figure-1) CR was 58% in no HA and 38% in HA group (p=0.072). In a multivariable Cox regression analysis including age, history of MDS, CR rates and serum albumin level at day 30; only CR rates and serum albumin were independent predictors of OS. (Table-1)
In this retrospective analysis of a cohort of patients with RR-AML; we demonstrated that serum albumin < 3.5 g/dl prior to start of salvage chemotherapy, at day 14 and at day 30 correlated with lower CR rates and worse OS. Serum albumin is a surrogate marker of general health, co- morbidities, and performance status. The prognostic value of low serum albumin need to be examined in newly diagnosed AML patients in context of known other prognostic factors; and validated in a prospective fashion.
KM estimates of OS in RR-AML patients with serum albumin day 30 < 3.5 g/dl vs ≥ 3.5 g/dl
KM estimates of OS in RR-AML patients with serum albumin day 30 < 3.5 g/dl vs ≥ 3.5 g/dl
Multivariable analysis for OS
| . | P value . | HR . |
|---|---|---|
| age | 0.122 | 0.986 |
| Albumin day 30 | 0.035 | 0.540 |
| CR rate | <0.001 | 3.535 |
| History of MDS | 0.149 | 0.649 |
| . | P value . | HR . |
|---|---|---|
| age | 0.122 | 0.986 |
| Albumin day 30 | 0.035 | 0.540 |
| CR rate | <0.001 | 3.535 |
| History of MDS | 0.149 | 0.649 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal