High-dose chemotherapy followed by autologous stem cell transplantation is the treatment of choice for HIV-negative patients with relapsed/refractory aggressive lymphoma. However, this paradigm has not been universally applied to patients with AIDS-related lymphoma, at least until recently.
Early in the AIDS epidemic, low-dose chemotherapy was used in patients with lymphoma, resulting in median survival of approximately 6 months. With the widespread use of highly active antiretroviral therapy (HAART) beginning in 1996, prognosis for these patients changed dramatically. Regimens such as EPOCH1 led to complete remission in 75% with 5-year survival achieved in approximately 70% of treated patients, confirmed in multi-institutional settings.
The outcome of HIV-infected patients with relapsed/refractory lymphoma has been less clear. Nonetheless, several studies have demonstrated that HAART-treated patients may achieve long-term, disease-free survival after high-dose chemotherapy and stem cell rescue, suggesting that similar management paradigms should be considered in both HIV-positive and HIV-negative patients. Krishnan and colleagues demonstrated the efficacy of this approach, reporting that 84% of 19 HIV-infected patients experienced continuous complete remission at a median follow-up of 27 months after aggressive chemotherapy and stem cell rescue.2 Similar results were reported by others.3 A recent retrospective study from City of Hope compared the outcome of stem cell transplantation in 29 HIV-infected patients with relapsed/refractory lymphoma to that of 29 HIV-negative controls, matched for sex, time from lymphoma to transplantation, age, disease status, number of prior regimens, conditioning regimen, and histology.4 Two-year progression-free survival (PFS) for the HIV-positive cohort was 76%, versus 56% for controls. At a median follow-up of 44 months, overall survival was 75% in both groups.
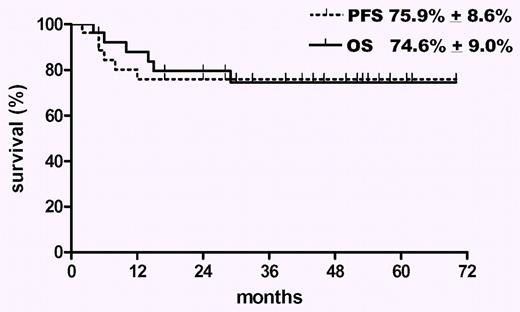
Whereas stem cell transplantation is thus feasible among HIV-infected patients with relapsed/refractory lymphoma, previous studies have not addressed the issues of patient selection and overall applicability of the procedure. The study in this issue by Re et al helps to resolve these issues.5 In a prospective, intent-to-treat analysis of 50 patients with chemo-sensitive relapse who were HAART responders at the time of initial lymphoma diagnosis, 27 (54%) actually met predesignated criteria to proceed to debulking chemotherapy, followed by stem cell collection (successful in 84%), BEAM therapy, and then peripheral blood stem cell transplantation. Factors associated with failure to proceed to transplantation included stage IV lymphoma and low CD4 cell count. The only factor associated with survival after transplantation was achievement of complete remission. Among the 27 patients who underwent transplantation, the median overall survival was 74.6% at 44 months, while the median PFS was 75.9% (see figure). No patient died from transplantation-related complications. This study demonstrates that approximately 50% of HIV-infected patients with relapsed/refractory lymphoma may actually make it to transplantation, while 75% of these may experience long-term, disease-free survival. Although the full scope of patient selection (in terms of patients excluded due to lack of HAART response, or chemotherapy insensitivity) has not been provided, the majority of these patients who undergo transplantation still appear to do very well. Additional progress, including novel use of anti-HIV gene-modified CD34+ peripheral blood progenitor cells has already been reported,6 and the prognosis of such patients continues to improve.
Overall survival and progression-free survival of 27 patients with AIDS-related lymphoma after peripheral blood stem cell transplantation (PBSCT). See the complete figure in the article beginning on page 1306.
Overall survival and progression-free survival of 27 patients with AIDS-related lymphoma after peripheral blood stem cell transplantation (PBSCT). See the complete figure in the article beginning on page 1306.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal