We thank Dr Teng and his colleagues for their comments regarding our recent manuscript. We reported that in the MC38 model, subcutaneous tumor growth and lung colonization were enhanced in interleukin-17 (IL-17)–deficient mice; and was associated with decreased interferon γ+ natural killer cells and tumor-specific interferon γ+ T cells in the tumor-draining lymph nodes and tumors. We concluded that endogenous IL-17 or/and Th17 cells may play a protective role in tumor immunity.
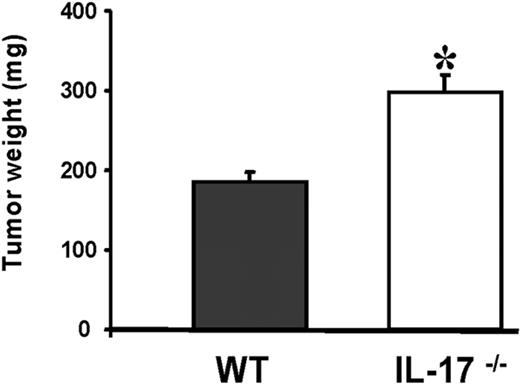
Dr Teng et al raised 3 points in their letter: (1) Our conclusion is based only on the MC38 tumor model. We agree that one tumor model may not be sufficient to make a broad conclusion. In additional experiments, we used the MCA310 sarcoma tumor and obtained similar results (Figure 1). Furthermore, by using the B16F10 melanoma model, a recent article published in Immunity reported concordant results.1 Therefore, based on the collective data, enhanced tumor growth was observed in IL-17–deficient mice bearing 3 histologically different tumors. (2) The second point is that we presented our data using tumor volume (mm3) rather than tumor area (mm2). We do not want to argue which parameter is more suitable for describing tumor growth. As an alternative, we have weighed tumors to objectively assess tumor burden. We found enhanced tumor weights in IL-17–deficient mice (Figure 1). (3) The third point is that we may have a different tumor line than the “regular” MC38. We agree that this possibility may exist as certain properties of tumor cell lines may be altered after cell culture. However, this argument would further support the observation that tumor growth is enhanced in IL-17–deficient mice.
Increased MCA310 tumor growth in IL-17–deficient mice. 3-Methylcholanthrene (MCA)–induced fibrosarcoma MCA310 tumors were maintained in vivo by serial subcutaneous transplantation in C57BL/6 mice. Tumor-cell suspensions were prepared from solid tumors by enzymatic digestion. Wild-type (WT) and IL-17–deficient (IL-17−/−) mice were subcutaneously inoculated with 1.2 × 106 tumor cells in the lower flank. Twelve days after tumor inoculation, tumors were harvested and weighed. Results were expressed as mean ± SEM; 2 independent experiments were performed with 5 animals per experiment per group. *P < .05.
Increased MCA310 tumor growth in IL-17–deficient mice. 3-Methylcholanthrene (MCA)–induced fibrosarcoma MCA310 tumors were maintained in vivo by serial subcutaneous transplantation in C57BL/6 mice. Tumor-cell suspensions were prepared from solid tumors by enzymatic digestion. Wild-type (WT) and IL-17–deficient (IL-17−/−) mice were subcutaneously inoculated with 1.2 × 106 tumor cells in the lower flank. Twelve days after tumor inoculation, tumors were harvested and weighed. Results were expressed as mean ± SEM; 2 independent experiments were performed with 5 animals per experiment per group. *P < .05.
The role of IL-17 in tumorigenesis is highly context-dependent.2 Earlier studies have shown that exogenous IL-17 promotes tumor growth by inducing tumor vascularization in tumor-bearing mice, particularly in immune-deficient mice.3,–5 The targets of IL-17 are basically tumor cells, vascular endothelial cells, and stromal cells. The overall effect of IL-17 on tumor development and growth may be different in immune-competent hosts as demonstrated by potent antitumor immunity mediated by IL-17 in immune-competent mice.6,7 Several lines of evidence further support this possibility. IL-17–deficient mice exhibit accelerated tumor growth and establishment of lung metastases.1,8 Blocking indoleamine 2,3-dioxygenase (IDO),9 dendritic cell/tumor cell fusion hybrid vaccination,10 and immune adjuvant treatments with IL-711 and hsp7012 result in improved antitumor immunity, which is associated with marked CD8+ T-cell activation and enhanced IL-17–expressing cells. These observations are consistent with experiments that show that Th17-polarized T cells induce tumor eradication in immune-competent mice.13,14
In addition to these mouse experiments, the newly generated data on patients with cancer may be directly relevant to our translational research goals. In patients with prostate cancer, a significant inverse correlation is found between Th17 skewing and tumor grade.15 Treatment with specific antibody against cytotoxic T-lymphocyte antigen 416 induces Th17 cells in patients with melanoma. Along this line, IL-17 was detected in ovarian cancer–associated ascites, and the levels of IL-17 positively predicted patient survival.17 Given that tumors develop in humans with reactive immune elements, our data provide supportive evidence that IL-17 may play a protective role in human tumor immunity.
Authorship
Acknowledgments: We thank Dr Y. Iwakura (University of Tokyo) for providing the IL-17–deficient mice. This work was partially supported by the National Cancer Institute (W.Z.).
Contribution: S.W., I.K., J.N., W.S., and L.V. performed research and analyzed data; and I.K., S.W., A.E.C., and W.Z. wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Weiping Zou, MD, PhD, University of Michigan School of Medicine, 1150 W. Medical Center, MSRB II, C560, Ann Arbor, MI 48109; e-mail: wzou@med.umich.edu.
References
National Institutes of Health