Although red blood cell (RBC) transfusions can be lifesaving, they are not without risk. In critically ill patients, RBC transfusions are associated with increased morbidity and mortality, which may increase with prolonged RBC storage before transfusion. The mechanisms responsible remain unknown. We hypothesized that acute clearance of a subset of damaged, stored RBCs delivers large amounts of iron to the monocyte/macrophage system, inducing inflammation. To test this in a well-controlled setting, we used a murine RBC storage and transfusion model to show that the transfusion of stored RBCs, or washed stored RBCs, increases plasma nontransferrin bound iron (NTBI), produces acute tissue iron deposition, and initiates inflammation. In contrast, the transfusion of fresh RBCs, or the infusion of stored RBC-derived supernatant, ghosts, or stroma-free lysate, does not produce these effects. Furthermore, the insult induced by transfusion of stored RBC synergizes with subclinical endotoxinemia producing clinically overt signs and symptoms. The increased plasma NTBI also enhances bacterial growth in vitro. Taken together, these results suggest that, in a mouse model, the cellular component of leukoreduced, stored RBC units contributes to the harmful effects of RBC transfusion that occur after prolonged storage. Nonetheless, these findings must be confirmed by prospective human studies.
Introduction
In the United States, the Food and Drug Administration (FDA) mandates that the maximal allowable shelf life of stored human red blood cells (RBCs) requires maintaining cellular integrity (assessed as free hemoglobin < 1% of total hemoglobin) together with an average 24-hour posttransfusion RBC survival of more than 75%.1 Depending on the preservative, the current maximal storage period for human RBC units is 21 to 42 days and the mean storage time before transfusion in the United States is 17 days.2 Although the mechanisms responsible for the reduced RBC viability induced by storage have not been definitively determined, 24-hour RBC survival decreases as storage time increases. In addition, despite FDA requirements, the 24-hour posttransfusion RBC survival at outdate can be less than 75%.1,3 Moreover, although RBC survival studies for FDA licensure are typically performed in healthy volunteers, the 24-hour posttransfusion RBC survival is often lower in critically ill patients.3,4 Finally, most RBC clearance occurs within the first hour after transfusion.3 One human RBC unit contains 220 to 250 mg of iron;5 therefore, rapid RBC clearance of up to 25% of even a single unit, acutely delivers a massive load of hemoglobin iron to the monocyte/macrophage system.
Observational studies suggest that prolonged RBC storage before transfusion increases mortality,6,,–9 serious infections,6,8,,–11 and multiorgan failure8,12 in some hospitalized patients. Two lines of reasoning suggest that the acute delivery of large amounts of iron to the monocyte/macrophage system can produce these adverse effects. First, in mice and humans, there is a relationship between the level of intracellular iron in macrophages and the levels of cytokines released in response to various inflammatory stimuli.13,–15 For example, in hemochromatosis, macrophages have decreased intracellular iron levels, which results in decreased cytokine production.13,15 Conversely, increased intracellular iron can exacerbate the systemic inflammatory response syndrome, which can lead to deleterious consequences. Second, increased circulating iron, especially nontransferrin bound iron (NTBI), enhances proliferation of certain pathogens.16,17 Interestingly, RBC transfusion increases NTBI levels in neonates,18 and may increase NTBI levels in patients with thalassemia19 ; however, studies in other patient populations have not been reported.
We previously reported20 that, in C57BL/6 mice, the 24-hour posttransfusion survival of leukoreduced mouse RBCs, stored for up to 2 weeks in a standard preservative solution of citrate-phosphate-dextrose-adenine-1 (CPDA-1), approximates the FDA standards for human RBCs at outdate. Nonetheless, this mouse model is not identical to the full FDA guidance criteria for human RBCs (ie, requiring an average 24-hour posttransfusion RBC survival of > 75% with a standard deviation < 9%, and the lower bound of the 95% confidence interval for the proportion of successful survival studies of 70%, based on at least 20 studies in distinct volunteers).1 In the current report, we hypothesized that the delivery of a substantial load of hemoglobin iron to the monocyte/macrophage system by acute clearance of transfused RBCs is a major cause of the adverse effects seen after transfusion of stored RBCs. To study this issue, we used the mouse RBC storage model to examine the consequences of transfusion of stored RBCs.
Methods
Mice
Wild-type C57BL/6 and FVB/NJ mice were purchased (The Jackson Laboratory). Serum amyloid A1 (SAA1)–luciferase reporter mice were obtained from Caliper Life Sciences. Mice were used at 8 to 12 weeks of age. Procedures were approved by the Institutional Animal Care and Use Committee of Columbia University.
Mouse RBC collection, storage, and derivatives
FVB/NJ and C57BL/6 mice were bled aseptically by cardiac puncture into CPDA-1 solution obtained directly from di-(2-ethylhexyl)phthalate–plasticized polyvinyl chloride human primary collection packs (product code 4R3611; Baxter). The final CPDA-1 concentration used for storage was 14%. Whole blood collected from 30 to 50 mice was pooled and leukoreduced using a Neonatal High-Efficiency Leukocyte Reduction Filter (Purecell Neo; Pall Corporation). Blood was centrifuged at 400g for 15 minutes, and the volume reduced to a final hemoglobin level ranging from 17.0 to 17.5 g/dL, as determined by a modified Drabkin hemoglobin assay,21 at a 1:251 dilution of stored RBCs to Drabkin reagent (Ricca Chemical Company). Optical density was measured at 540 nm and compared with the Count-a-part Cyanmethemoglobin Standards Set (Diagnostic Technology). Residual leukocytes were enumerated by flow cytometry (LeucoCOUNT Kit; BD Biosciences). The stored RBCs (∼ 10 mL) were placed in 15-mL Falcon tubes, sealed with Parafilm, and stored in the dark at 4°C for up to 14 days. On the day of transfusion, a 500-μL aliquot of stored RBCs was inoculated into a Peds Plus/F blood culture bottle (BD Diagnostic Systems) and loaded into the BACTEC Fx (BD Diagnostic Systems), a continuous monitoring blood culture system, for up to 5 days or until bacterial growth was detected (this method detects at least 10 colony forming units [CFU] per milliliter with a sensitivity of 97%).22
Washed stored RBCs were prepared with 3 washes using 10 volumes of phosphate-buffered saline (PBS) and centrifugation at 400g. After the final wash, the washed stored RBCs were resuspended in PBS to a final hemoglobin concentration of 17.0 to 17.5 g/dL for transfusion. Supernatant was obtained using a 400g spin of stored RBCs and 400 μL of this solution were transfused undiluted. RBC ghosts were obtained by hypotonic lysis of twice the volume of stored RBCs (ie, for 400 μL of ghosts, 800 μL of stored RBCs were hemolyzed) with PBS to distilled water (1:15), followed by multiple washes with the same buffer and centrifugation at 30 000g until a white pellet was obtained. The white pellet of RBC ghosts was resuspended in PBS. Stroma-free RBC lysate was prepared by freeze-thaw of washed stored RBCs followed by centrifugation at 16 000g to pellet and remove the stroma.
Transfusion and short-term RBC survival
RBC suspensions (200 or 400 μL at 17.0-17.5 g/dL hemoglobin; 1 or 2 equivalent human units, respectively) were transfused through the retro-orbital plexus of isoflurane-anesthetized mice. The proportion of transfused RBCs circulating at 2 and 24 hours posttransfusion (ie, the 2- and 24-hour posttransfusion survival) was measured by either a dual- or a single-labeling method (preliminary studies confirmed that there were no significant differences in these methods for the conditions of this protocol [data not shown]). For dual labeling, an aliquot of fresh, syngeneic C57BL/6 RBCs was labeled with chloromethylbenzamido 1,1′-dioctadecyl-3,3,3′,3′-tetramethylindocarbocyanine perchlorate (DiI; Invitrogen) and an aliquot of fresh or stored, allogeneic FVB/NJ RBCs was labeled with 3,3′-dihexadecyloxacarbocyanine perchlorate (DiO; Invitrogen), as previously described.23 At defined time points after transfusion, 1 to 2 μL of blood was obtained from the tail vein and added to 500 μL of PBS for flow cytometric detection of fluorescently labeled RBCs. Percent survival was calculated by comparing the ratio of DiI- to DiO-labeled RBCs in the sample to the ratio in the transfusate itself. For single-label studies, a 10% aliquot of fresh or stored RBCs was labeled with DiO. To determine percent survival, the ratio of DiO-labeled RBCs to unlabeled RBCs, acquired using a FACSCalibur flow cytometer (BD Biosciences), was compared between a 10-minute posttransfusion sample and a sample obtained at the final end point. At a defined time point (2 or 24 hours after transfusion), mice were anesthetized with isoflurane and killed, and blood obtained by cardiac puncture using heparinized syringes was used for measuring RBC survival and plasma analytes.
For some experiments, lipopolysaccharide (LPS) isolated from Escherichia coli 0111:B4 (30 μg-100 μg per mouse; Sigma-Aldrich) dissolved in 100 μL of PBS was injected into the tail vein of mice immediately before transfusion. In some experiments, 3 mg of deferoxamine (DFO; Novartis) dissolved in 100 μL of PBS, or 3 mg of DFO preincubated for 1 hour with an equimolar concentration of ferric citrate (Sigma-Aldrich), were injected into the tail vein of mice immediately before transfusion. Finally, in some experiments, 2 mg of liposomal clodronate or PBS-liposomes (both from Encapsula NanoSciences LLC) were injected intraperitoneally into mice 48 hours before transfusion.
Histology and immunohistochemistry
At necropsy, the liver and spleen were removed, fixed overnight with 10% neutral-buffered formalin, and embedded in paraffin. Sections were stained with hematoxylin and eosin or were deparaffinized and immunostained with an anti–mouse F4/80 monoclonal antibody (eBioscience) at a 1:500 dilution, followed by biotinylated anti–rat secondary antibody (1:200 dilution), ABC reagent (1:50 dilution), and development with a 3,3′-diaminobenzidine substrate kit (all from Vector Laboratories). Images were captured using an Olympus BX40 microscope and a SPOT INSIGHT digital camera (Diagnostic Instruments).
Inflammatory protein measurements
Cytokines/chemokines, including interleukin-6 (IL-6), interleukin-10 (IL-10), monocyte chemoattractant protein-1 (MCP-1), interferon-γ (IFN-γ), tumor necrosis factor-α (TNF-α), macrophage inhibitory protein-1β (MIP-1β), and keratinocyte-derived chemokine/CXCL1 (KC/CXCL1), were quantified using the Cytometric Bead Array Mouse Flex Kit (BD Biosciences). Heparinized plasma obtained by cardiac puncture was analyzed at a 1:4 or 1:10 dilution or at both dilutions. Flow cytometric cytokine data, acquired with a FACSCalibur flow cytometer (BD Biosciences), were analyzed using FlowJo software (TreeStar). Plasma SAA levels were measured using a mouse SAA ELISA Kit (Life Diagnostics) following the manufacturer's instructions.
Iron-related measurements
Plasma NTBI was measured by a nitrilotriacetic acid (Sigma-Aldrich) ultrafiltration assay.24 In brief, heparinized plasma (90 μL) was incubated with 800mM nitrilotriacetic acid, pH 7.0, at room temperature for 30 minutes. Plasma proteins were removed by ultrafiltration (NanoSep, 30-kDa cutoff, polysulfone type; Pall Corporation) by centrifugation at 10 620g at 15°C for 45 minutes, and iron in the ultrafiltrate was measured by a ferrozine assay.25 Total organ iron was determined using a wet ashing procedure.26 In brief, the wet weight of organs obtained at necropsy was quantified; the entire spleen or portions of the liver (∼ 100 mg) or kidney (∼ 80 mg) were placed in 2-mL glass vials. After desiccation at 65°C for 24 hour, 200 μL of acid mixture (70% perchloric acid:nitric acid 2:1) were added. After drying for 5 to 6 hours at 182°C, 1 mL of 3M HCl was added and mixed. The acidified sample (50 μL) was then incubated for 30 minutes with 200 μL of chromogen (1.6mM bathophenanthroline, 2M sodium acetate, and 11.5mM thioglycolic acid). Absorbance of samples and iron standards at 535 nm was measured in duplicate and mean values used for calculating total organ iron. Hemoglobinemia was detected spectrophotometrically using a PowerWave XS spectrophotometer (BioTek).
Imaging of luciferase activity in vivo
Male SAA1-luciferase transgenic mice27 were transfused by tail-vein injection with 200 μL of fresh RBCs (< 24-hour storage) or stored RBCs. Bioluminescence imaging was performed using an In Vivo Imaging System (Caliper Life Sciences), as described.27 Mice were anesthetized with isoflurane, injected intraperitoneally with 150 mg/kg luciferin (Caliper Life Sciences), and imaged 10 minutes later for 1 to 60 seconds. Photons emitted from specific regions were quantified using LivingImage software (Caliper Life Sciences); luciferase activity is expressed as photons per second.
Bacterial growth in vitro
A pathogenic strain of E coli, obtained from an anonymous patient with a urinary tract infection, was used. For each experiment, a sample from the frozen stock of this E coli was inoculated into nutrient broth (Difco Laboratories) and grown to mid-log phase (∼ 3 hours). Bacteria were then washed twice in PBS and resuspended to approximately 200 000 CFU/μL. A total of 5 μL of bacterial suspension (1 × 106 CFU total) were then added to 100 μL of heparinized plasma in a 96-well EIA/RIA plate (Corning; Costar). Bacterial growth was measured by absorbance at 600 nm. In some experiments, specified amounts of ferric citrate, sodium citrate, bovine serum albumin, 2,2′-dipyridyl (all from Sigma-Aldrich), protoporphyrin IX (Frontier Scientific), or DFO were added to plasma before bacterial inoculation.
Statistical analysis
Significance between 2 means was calculated using a 2-tailed Mann-Whitney U test. Significance relevant to bacterial growth in vitro was determined by converting each growth curve to an area under the curve (AUC) value followed by a 2-tailed Mann-Whitney U test to compare mean AUC for each group. A value for P less than .05 was considered significant. Statistical analyses and AUC calculations were performed using Prism 5 (GraphPad Software).
Results
A subpopulation of transfused stored RBCs is rapidly cleared by macrophages, resulting in iron deposition in the liver, spleen, and kidney and production of plasma NTBI
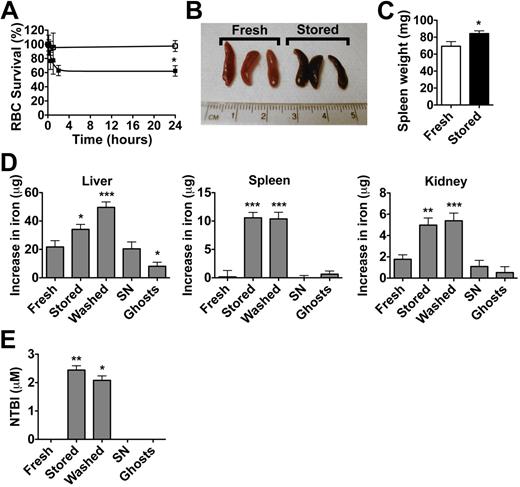
In the current study, donor FVB/NJ mouse RBCs were used to model an allogeneic transfusion in C57BL/6 recipients. RBCs were leukoreduced before storage (> 3-log10 leukocyte reduction [data not shown]) and blood cultures from poststorage aliquots had no microbial growth after incubation for 5 days. The 24-hour posttransfusion survival results for fresh (ie, < 24 hours of storage) and 2-week stored allogeneic FVB/NJ RBCs transfused into C57BL/6 mice were similar to those obtained for syngeneic transfusions (Figure 1A).20 For the experiments presented hereafter, all stored RBCs were transfused after 2 weeks of storage.
Transfusion of stored RBCs. Transfusions of stored RBCs lead to increased RBC clearance, tissue iron delivery, and circulating NTBI levels, compared with transfusions of fresh RBCs, stored RBC-derived supernatant, or ghosts prepared from stored RBCs. All transfusion recipients were male C57BL/6 mice (8-12 weeks of age). The results are presented as mean (± SEM) except where specified. (A) Leukoreduced fresh FVB/NJ mouse RBCs (< 24-hour storage; n = 3; □) and stored RBCs (2-week storage; n = 5; ■) were transfused (400 μL at 17.0-17.5 g/dL of hemoglobin), and survival of transfused RBCs was calculated by dual-label flow cytometric tracking at 10 minutes, 30 minutes, 1 hour, 2 hours (only for stored RBCs), and 24 hours after transfusion. The results are from 1 representative experiment and are presented as mean (± SD). (B) A representative image of spleens obtained from mice 2 hours after transfusion with fresh RBCs or stored RBCs. (C) Mean spleen weight of mice transfused with fresh RBCs (n = 13) and stored RBCs (n = 13). (D) Aliquots (400 μL) of fresh RBCs (n = 13), stored RBCs (n = 13), washed stored RBCs (n = 13), stored RBC-derived supernatant (SN; n = 12), and ghosts prepared from stored RBCs (n = 8) were transfused. Total iron was measured in organs obtained at necropsy 2 hours after transfusion; the increases in iron are shown compared with levels measured in control, untransfused mice (n = 12). The results are combined from 3 separate experiments. (E) Mice were transfused as labeled (n = 5 per group) and plasma NTBI levels were measured 2 hours after transfusion. Note that the absence of an error bar indicates undetectable NTBI levels. The results are representative of 2 separate experiments; *P < .05; **P < .01; ***P < .001 compared with fresh RBC transfusions.
Transfusion of stored RBCs. Transfusions of stored RBCs lead to increased RBC clearance, tissue iron delivery, and circulating NTBI levels, compared with transfusions of fresh RBCs, stored RBC-derived supernatant, or ghosts prepared from stored RBCs. All transfusion recipients were male C57BL/6 mice (8-12 weeks of age). The results are presented as mean (± SEM) except where specified. (A) Leukoreduced fresh FVB/NJ mouse RBCs (< 24-hour storage; n = 3; □) and stored RBCs (2-week storage; n = 5; ■) were transfused (400 μL at 17.0-17.5 g/dL of hemoglobin), and survival of transfused RBCs was calculated by dual-label flow cytometric tracking at 10 minutes, 30 minutes, 1 hour, 2 hours (only for stored RBCs), and 24 hours after transfusion. The results are from 1 representative experiment and are presented as mean (± SD). (B) A representative image of spleens obtained from mice 2 hours after transfusion with fresh RBCs or stored RBCs. (C) Mean spleen weight of mice transfused with fresh RBCs (n = 13) and stored RBCs (n = 13). (D) Aliquots (400 μL) of fresh RBCs (n = 13), stored RBCs (n = 13), washed stored RBCs (n = 13), stored RBC-derived supernatant (SN; n = 12), and ghosts prepared from stored RBCs (n = 8) were transfused. Total iron was measured in organs obtained at necropsy 2 hours after transfusion; the increases in iron are shown compared with levels measured in control, untransfused mice (n = 12). The results are combined from 3 separate experiments. (E) Mice were transfused as labeled (n = 5 per group) and plasma NTBI levels were measured 2 hours after transfusion. Note that the absence of an error bar indicates undetectable NTBI levels. The results are representative of 2 separate experiments; *P < .05; **P < .01; ***P < .001 compared with fresh RBC transfusions.
At 2 hours after transfusion, darkening of the spleen (Figure 1B) and increased spleen weight (Figure 1C) were observed at necropsy, but only in mice transfused with stored RBCs. No significant differences in liver or kidney weight were detected (data not shown). To determine the fate of the hemoglobin iron cleared after transfusion of stored RBCs, tissue iron levels were measured at necropsy 2 hours after transfusion with (1) fresh RBCs; (2) stored RBCs; (3) washed stored RBCs; (4) supernatant prepared from stored RBCs; and (5) ghosts derived from stored RBCs. Washed stored RBCs were resuspended in PBS so that the amount of hemoglobin transfused was similar to that of fresh RBCs and unwashed stored RBCs (ie, a 400-μL volume containing 17.0-17.5 g/dL hemoglobin per transfusion). Supernatant and stored RBC-derived ghosts contained an average hemoglobin of 1.19 g/dL (SEM 0.48) and less than 0.02 g/dL, respectively. Compared with fresh RBC transfusions, the mean total iron was significantly increased in liver (12.1 μg), spleen (10.1 μg), and kidney (2.8 μg) after stored RBC transfusion (Figure 1D). In a typical experiment, approximately 225 μg of total iron were transfused per mouse (calculated as the amount of iron in 400 μL of RBCs containing 17.5 g/dL hemoglobin). Based on the survival data in these experiments, 16.4% of stored RBCs were cleared by 2 hours after transfusion, resulting in the clearance of approximately 36 μg of iron from the circulation; thus, the excess iron recovered in spleen, kidney, and liver of these mice together accounts for approximately 70% of the total iron delivered. Bone marrow iron was not measured. Only stored RBC and washed stored RBC transfusions increased plasma NTBI levels at 2 hours after transfusion (Figure 1E). This surge in plasma NTBI was short-lived, as plasma NTBI levels were undetectable by 24 hours after transfusion of stored RBCs.
To determine whether macrophages were responsible for clearing stored RBCs in this model, mice were treated with liposomal clodronate or control PBS-liposomes 48 hours before transfusion. The 2-hour RBC survival was significantly increased in liposomal clodronate-treated mice compared with the PBS-liposomal control (Figure 2A). Liposomal clodronate treatment depleted hepatic and splenic (Figure 2B) macrophages, as assessed by immunohistochemistry for the F4/80 mouse macrophage marker. In nonclodronate-treated control animals transfused with syngeneic stored RBCs, histologic examination showed increased erythrophagocytosis by hepatic (Figure 2C) and splenic (data not shown) macrophages, which was confirmed by F4/80 staining of macrophages (Figure 2C).
Macrophages are responsible for clearing transfused stored RBCs. All transfusion recipients and donors were syngeneic male C57BL/6 mice (8-12 weeks of age). (A) Mice were infused intraperitoneally with 2 mg of liposomal clodronate (n = 9) or control PBS-liposomes (n = 10) 48 hours before transfusion with stored RBCs. The 2-hour RBC survival was then measured. The 2-hour RBC survival (■) is indicated for each mouse and the horizontal bar indicates the mean. The results are representative of 2 separate experiments; ***P < .001 compared with treatment with PBS-liposomes. (B) Representative images of histologic sections of liver and spleen from mice treated with liposomal clodronate or control PBS-liposomes 48 hours before transfusion with stored RBCs, and stained with an anti–mouse F4/80 monoclonal antibody, as labeled. Note the absence of tissue macrophages in the liposomal clodronate–treated mice, as evidenced by the absence of brown staining cells. (C) Representative images of histologic sections from the liver of mice transfused with fresh or stored RBCs. Sections were stained with hematoxylin & eosin or with an anti–mouse F4/80 monoclonal antibody, as labeled. Arrows denote tissue macrophages that ingested RBCs. Brown staining is a result of F4/80 immunoreactivity of macrophages; the cytoplasmic staining is displaced to the periphery of the cells in mice transfused with stored RBCs because of the accumulation of ingested RBCs. Original magnification was ×400. Typical representative examples derived from 5 necropsies are shown.
Macrophages are responsible for clearing transfused stored RBCs. All transfusion recipients and donors were syngeneic male C57BL/6 mice (8-12 weeks of age). (A) Mice were infused intraperitoneally with 2 mg of liposomal clodronate (n = 9) or control PBS-liposomes (n = 10) 48 hours before transfusion with stored RBCs. The 2-hour RBC survival was then measured. The 2-hour RBC survival (■) is indicated for each mouse and the horizontal bar indicates the mean. The results are representative of 2 separate experiments; ***P < .001 compared with treatment with PBS-liposomes. (B) Representative images of histologic sections of liver and spleen from mice treated with liposomal clodronate or control PBS-liposomes 48 hours before transfusion with stored RBCs, and stained with an anti–mouse F4/80 monoclonal antibody, as labeled. Note the absence of tissue macrophages in the liposomal clodronate–treated mice, as evidenced by the absence of brown staining cells. (C) Representative images of histologic sections from the liver of mice transfused with fresh or stored RBCs. Sections were stained with hematoxylin & eosin or with an anti–mouse F4/80 monoclonal antibody, as labeled. Arrows denote tissue macrophages that ingested RBCs. Brown staining is a result of F4/80 immunoreactivity of macrophages; the cytoplasmic staining is displaced to the periphery of the cells in mice transfused with stored RBCs because of the accumulation of ingested RBCs. Original magnification was ×400. Typical representative examples derived from 5 necropsies are shown.
Inflammation produced after rapid clearance of a subpopulation of transfused stored RBCs requires membrane-encapsulated hemoglobin iron
To determine whether transfusion of stored RBCs induces inflammation, and whether membrane-encapsulated hemoglobin iron is required, rather than factors accumulating in the stored RBC supernatant, recipient mice were transfused with normalized amounts of (1) fresh RBCs; (2) stored RBCs; (3) washed stored RBCs; (4) stored RBC-derived supernatant; (5) ghosts prepared from stored RBCs; or (6) stroma-free stored RBC lysate. At 2 hours after transfusion, mice transfused with stroma-free stored RBC lysate had dramatic hemoglobinemia (Figure 3A) and hemoglobinuria (data not shown), compared with mice transfused with intact RBCs. Nonetheless, a dose-responsive proinflammatory cytokine response involving increased circulating levels of IL-6, MCP-1, KC/CXCL1, MIP-1β, and TNF-α was only detected after transfusion of either stored RBCs or washed stored RBCs (Figure 3B). No significant differences were seen with IL-10 or IFN-γ. Qualitatively similar cytokine results were obtained after transfusion of stored syngeneic RBCs (ie, from C57BL/6 donors; E.A.H. and S.L.S, unpublished data, December 30, 2009). Taken together, these results suggest that the contents of RBCs, when membrane encapsulated, are required to induce a proinflammatory response.
Transfusion of stored RBCs induces dose-responsive proinflammatory cytokine responses. (A) Hemoglobinemia, as detected by absorbance, was observed in all mice (n = 8) transfused with stroma-free lysate derived from stored RBCs. Representative spectra of plasma (diluted 1:4 with PBS) obtained from mice 2 hours after transfusion with fresh RBCs (< 24-hour storage), stored RBCs (2-week storage), or stroma-free lysate derived from stored RBCs are shown. (B) Untransfused C57BL/6 mice (n = 13) or mice transfused with fresh RBCs (1u = 200 μL, n = 5; [ie, 1 human equivalent unit = 200 μL]; 2u = 400 μL, n = 17), stored RBCs (1u = 200 μL, n = 5; 2u = 400 μL, n = 17), washed stored RBCs (400 μL; n = 13), stored RBC-derived supernatant (SN, 400 μL, n = 12), ghosts prepared from stored RBCs (400 μL, n = 8), and stroma-free lysate derived from stored RBCs (400 μL, n = 8) were killed 2 hours after transfusion, and plasma cytokine levels were measured (as labeled); *P < .05; **P < .01; ***P < .001 compared with fresh RBCs.
Transfusion of stored RBCs induces dose-responsive proinflammatory cytokine responses. (A) Hemoglobinemia, as detected by absorbance, was observed in all mice (n = 8) transfused with stroma-free lysate derived from stored RBCs. Representative spectra of plasma (diluted 1:4 with PBS) obtained from mice 2 hours after transfusion with fresh RBCs (< 24-hour storage), stored RBCs (2-week storage), or stroma-free lysate derived from stored RBCs are shown. (B) Untransfused C57BL/6 mice (n = 13) or mice transfused with fresh RBCs (1u = 200 μL, n = 5; [ie, 1 human equivalent unit = 200 μL]; 2u = 400 μL, n = 17), stored RBCs (1u = 200 μL, n = 5; 2u = 400 μL, n = 17), washed stored RBCs (400 μL; n = 13), stored RBC-derived supernatant (SN, 400 μL, n = 12), ghosts prepared from stored RBCs (400 μL, n = 8), and stroma-free lysate derived from stored RBCs (400 μL, n = 8) were killed 2 hours after transfusion, and plasma cytokine levels were measured (as labeled); *P < .05; **P < .01; ***P < .001 compared with fresh RBCs.
Transfusions of stored RBCs induce an acute-phase inflammatory response
To investigate the inflammatory response after stored RBC transfusions in greater detail, male transgenic SAA1-luciferase reporter mice27 were transfused with 200 μL of fresh RBCs or stored RBCs. SAA1 is an acute phase reactant induced by elevated levels of proinflammatory cytokines.27 Only stored RBC transfusions induced a robust luciferase signal in the hepatosplenic region (> 300-fold over baseline, Figure 4A-B) as measured by noninvasive bioluminescent imaging. Expression was detectable by 4 hours after transfusion and returned to baseline by 24 hours after transfusion. Plasma SAA1 protein levels at 24 hours after transfusion were consistent with the imaging results (Figure 4C).
Transfusion of stored RBCs induces an acute phase response.(A) SAA1-luciferase reporter mice were transfused with 200 μL of either fresh RBCs (< 24-hour storage) or stored RBCs (2-week storage) and luciferase activity measured by noninvasive bioluminescence imaging at multiple times up to 24 hours after transfusion (n = 3 per group). Results are representative of 2 experiments. (B) Bioluminescence was quantified over the hepatosplenic region of SAA1-luciferase reporter mice transfused with fresh RBCs (n = 6;  ) or stored RBCs (n = 6; ■); *P < .01. (C) Circulating SAA1 protein levels in SAA1-luciferase reporter mice 24 hours after transfusion with fresh RBCs or stored RBCs (n = 6 per group); *P < .01. Results are combined from 2 separate experiments.
) or stored RBCs (n = 6; ■); *P < .01. (C) Circulating SAA1 protein levels in SAA1-luciferase reporter mice 24 hours after transfusion with fresh RBCs or stored RBCs (n = 6 per group); *P < .01. Results are combined from 2 separate experiments.
Transfusion of stored RBCs induces an acute phase response.(A) SAA1-luciferase reporter mice were transfused with 200 μL of either fresh RBCs (< 24-hour storage) or stored RBCs (2-week storage) and luciferase activity measured by noninvasive bioluminescence imaging at multiple times up to 24 hours after transfusion (n = 3 per group). Results are representative of 2 experiments. (B) Bioluminescence was quantified over the hepatosplenic region of SAA1-luciferase reporter mice transfused with fresh RBCs (n = 6;  ) or stored RBCs (n = 6; ■); *P < .01. (C) Circulating SAA1 protein levels in SAA1-luciferase reporter mice 24 hours after transfusion with fresh RBCs or stored RBCs (n = 6 per group); *P < .01. Results are combined from 2 separate experiments.
) or stored RBCs (n = 6; ■); *P < .01. (C) Circulating SAA1 protein levels in SAA1-luciferase reporter mice 24 hours after transfusion with fresh RBCs or stored RBCs (n = 6 per group); *P < .01. Results are combined from 2 separate experiments.
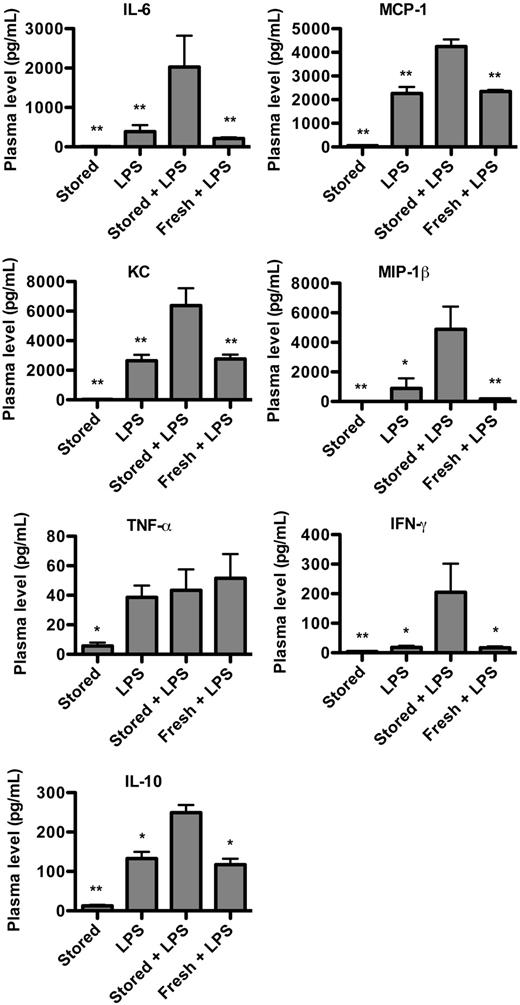
Transfusions of stored RBCs exacerbate inflammation induced by endotoxin
Although stored RBC transfusions induced a significant proinflammatory response, no mice developed clinical symptoms such as anorexia, reduced mobility, decreased alertness, or lack of grooming. Nonetheless, we hypothesized that the inflammatory response to stored RBC transfusions could exacerbate an inflammatory state induced by a separate mechanism and result in clinical symptoms, potentially explaining the relationship between critically ill patients, older stored RBC transfusions, and adverse outcomes.7,8 Thus, recipient mice were injected with a subclinical dose of LPS, with or without concurrent fresh RBC or stored RBC transfusions. After sacrifice 24-hour posttransfusion (or earlier if moribund), cytokines were measured. LPS-treated mice transfused with stored RBCs maintained markedly elevated levels of multiple cytokines, including IL-6, MCP-1, KC/CXCL1, MIP-1β, IFN-γ, and IL-10 (Figure 5). In addition, in experiments with higher LPS doses, the LPS-treated mice transfused with stored RBCs were moribund by 18 to 24 hours after transfusion, exhibiting a hunched posture and absent spontaneous movement, whereas all other groups of mice were markedly less ill and exhibited spontaneous movement and grooming (data not shown).
Transfusion of stored RBCs synergizes with the inflammatory response to LPS. C57BL/6 mice were infused with a subclinical dose of LPS (E coli 0111:B4 strain; 30 μg per mouse by tail-vein injection) immediately followed by transfusion of 400 μL of fresh RBCs or stored RBCs. Mice were killed 24 hours after transfusion, and plasma cytokines were measured (n = 5 per group). Results are representative of 2 experiments. *P < .05; **P < .01; ***P < .001 compared with mice infused with LPS plus stored RBCs.
Transfusion of stored RBCs synergizes with the inflammatory response to LPS. C57BL/6 mice were infused with a subclinical dose of LPS (E coli 0111:B4 strain; 30 μg per mouse by tail-vein injection) immediately followed by transfusion of 400 μL of fresh RBCs or stored RBCs. Mice were killed 24 hours after transfusion, and plasma cytokines were measured (n = 5 per group). Results are representative of 2 experiments. *P < .05; **P < .01; ***P < .001 compared with mice infused with LPS plus stored RBCs.
Transfusions of stored RBCs enhances pathogen growth in vitro
Heparinized plasma samples obtained from mice after transfusion were inoculated in vitro with a pathogenic strain of E coli and growth was measured by turbidity. Plasma obtained from mice 2 hours after transfusion with either stored RBCs or washed stored RBCs showed significantly increased bacterial growth compared with that from untransfused mice or mice transfused with either fresh RBCs, supernatant derived from stored RBCs, or ghosts prepared from stored RBCs (Figure 6A). This was an acute effect because plasma collected 24 hours after stored RBC transfusion did not enhance bacterial growth (Figure 6A). The total iron in pooled plasma at 2 hours after transfusion with fresh RBCs or stored RBCs was 176 μg/dL or 295 μg/dL, respectively (ie, increased by ∼ 20μM after stored RBC transfusion). When ferric citrate (20μM), but not sodium citrate (20μM), bovine serum albumin (80μM), or protoporphyrin IX (20μM), was added to pooled plasma from mice transfused with fresh RBCs, bacterial growth was promoted to a similar level as in plasma from mice transfused with stored RBCs (Figure 6B). Conversely, when 20μM of an iron chelator, DFO, was added to pooled plasma from mice transfused with stored RBCs, bacterial growth was partially inhibited (Figure 6C). This inhibition was due to the iron-binding capacity of DFO because preincubation of DFO with an equimolar amount of ferric citrate (ie, producing ferroxamine [FO]) prevented the inhibition of bacterial growth. A more dramatic inhibition of bacterial growth was probably not achieved because some types of bacteria can use FO as an iron source.28 Nonetheless, a greater inhibition of bacterial growth was achieved using higher concentrations of the bidentate ferrous iron chelator, 2,2′-dipyridyl29 (Figure 6D). This inhibitory effect was similarly abrogated when the 2,2′-dipyridyl was preincubated with a one-third molar ratio of ferric citrate.
Plasma from mice transfused with stored RBCs enhances bacterial growth in vitro. (A) Plasma (100 μL) was obtained from mice 2 hours after transfusion with 400 μL of fresh RBCs (n = 15), stored RBCs (n = 24), stored RBC-derived supernatant (SN, n = 12), washed stored RBCs (n = 13), or ghosts prepared from stored RBCs (n = 8). Plasma was also obtained from control, untransfused mice (n = 14) or 24 hours after transfusion with stored RBCs (n = 8). Samples were incubated at 37°C with shaking with ∼ 1 × 106 CFU of E coli, as labeled. Bacterial growth was monitored every 30 minutes by absorbance at 600 nm for up to 5 hours. Bacterial growth in plasma obtained from mice 2 hours after transfusion with stored RBCs or washed stored RBCs began diverging from all other groups at 2.5 hours of incubation in vitro, and AUC (in parentheses) for each group was significantly different as indicated. (B) Pooled plasma samples (100 μL) from mice 2 hours after transfusion with 400 μL of fresh RBCs or stored RBCs were supplemented with either ferric citrate (20μM), sodium citrate (20μM), bovine serum albumin (BSA; 80μM), or protoporphyrin IX (20μM), and then incubated at 37°C with shaking with ∼ 1 × 106 CFU of E coli. Bacterial growth was monitored every 30 minutes by absorbance at 600 nm for up to 5 hours in replicates of 5 per group. AUC (in parentheses) for growth in plasma from mice transfused with fresh RBCs, supplemented with or without sodium citrate, BSA, or protoporphyrin IX, differed significantly from the other 3 groups. (C) Pooled plasma (n = 4) were incubated with the iron chelator, DFO (20 μM), or with the iron-chelated form FO (20 μM) and inoculated with E coli as shown for the previous experiment. The AUC (in parentheses) for growth in plasma with DFO significantly differed from all other groups. (D) Pooled plasma (n = 5) was incubated with the iron chelator, 2,2′-dipyridyl (400μM), with or without ferric citrate (133μM) and inoculated with E coli, as shown for the previous experiment. The AUC (in parentheses) for growth in plasma with 2,2′-dipyridyl significantly differed from all other groups; *P < .05. Results are representative of at least 2 experiments and are shown as mean (± SEM). Note that the absence of an error bar is indicative of highly reproducible replicates with pooled plasma.
Plasma from mice transfused with stored RBCs enhances bacterial growth in vitro. (A) Plasma (100 μL) was obtained from mice 2 hours after transfusion with 400 μL of fresh RBCs (n = 15), stored RBCs (n = 24), stored RBC-derived supernatant (SN, n = 12), washed stored RBCs (n = 13), or ghosts prepared from stored RBCs (n = 8). Plasma was also obtained from control, untransfused mice (n = 14) or 24 hours after transfusion with stored RBCs (n = 8). Samples were incubated at 37°C with shaking with ∼ 1 × 106 CFU of E coli, as labeled. Bacterial growth was monitored every 30 minutes by absorbance at 600 nm for up to 5 hours. Bacterial growth in plasma obtained from mice 2 hours after transfusion with stored RBCs or washed stored RBCs began diverging from all other groups at 2.5 hours of incubation in vitro, and AUC (in parentheses) for each group was significantly different as indicated. (B) Pooled plasma samples (100 μL) from mice 2 hours after transfusion with 400 μL of fresh RBCs or stored RBCs were supplemented with either ferric citrate (20μM), sodium citrate (20μM), bovine serum albumin (BSA; 80μM), or protoporphyrin IX (20μM), and then incubated at 37°C with shaking with ∼ 1 × 106 CFU of E coli. Bacterial growth was monitored every 30 minutes by absorbance at 600 nm for up to 5 hours in replicates of 5 per group. AUC (in parentheses) for growth in plasma from mice transfused with fresh RBCs, supplemented with or without sodium citrate, BSA, or protoporphyrin IX, differed significantly from the other 3 groups. (C) Pooled plasma (n = 4) were incubated with the iron chelator, DFO (20 μM), or with the iron-chelated form FO (20 μM) and inoculated with E coli as shown for the previous experiment. The AUC (in parentheses) for growth in plasma with DFO significantly differed from all other groups. (D) Pooled plasma (n = 5) was incubated with the iron chelator, 2,2′-dipyridyl (400μM), with or without ferric citrate (133μM) and inoculated with E coli, as shown for the previous experiment. The AUC (in parentheses) for growth in plasma with 2,2′-dipyridyl significantly differed from all other groups; *P < .05. Results are representative of at least 2 experiments and are shown as mean (± SEM). Note that the absence of an error bar is indicative of highly reproducible replicates with pooled plasma.
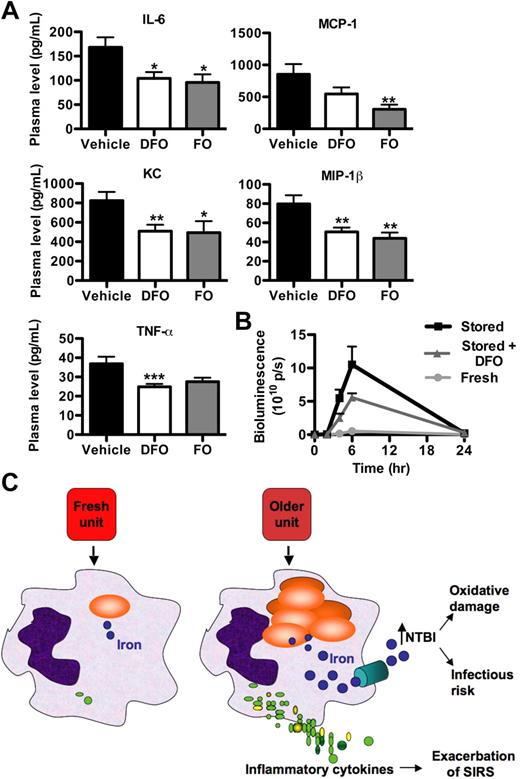
DFO and FO partly ameliorate the inflammatory response induced by transfusion of stored RBCs
To examine whether administration of an iron chelator with antioxidative properties can ameliorate the proinflammatory response induced by stored RBC transfusions, mice were infused intravenously with 3 mg (ie, ∼ 120 mg/kg) of DFO, an FDA-approved iron chelator, immediately before transfusion. DFO significantly inhibited increases in proinflammatory cytokine levels (Figure 7A) and showed a trend toward reducing the luciferase signal in SAA1-luciferase reporter mice (Figure 7B). However, SAA protein levels were not significantly different at 24 hours after transfusion (data not shown).
DFO treatment decreases the proinflammatory response induced by transfusion of stored RBCs. (A) Mice were pretreated with a PBS vehicle control (n = 28) or with 3 mg of DFO, with (n = 15) or without (n = 31) the addition of equimolar ferric citrate, immediately before transfusion with stored RBCs (400 μL). Mice were killed 2 hours after transfusion, and plasma cytokine levels were measured; *P < .05; **P < .01; ***P < .001 compared with mice infused with PBS vehicle and transfused stored RBCs. (B) Bioluminescence was quantified for 24 hours after transfusion over the hepatosplenic region of SAA1-luciferase reporter mice transfused with 200 μL of fresh RBCs (n = 3;  ), the PBS vehicle control and stored RBCs (n = 3; ■), or 3 mg of DFO and stored RBCs (n = 6;
), the PBS vehicle control and stored RBCs (n = 3; ■), or 3 mg of DFO and stored RBCs (n = 6;  ); P = .095 at 4 and 6 hours after transfusion comparing vehicle-treated and DFO-treated mice. (C) Proposed mechanistic pathway (the “iron hypothesis”) explaining how transfusion of older stored RBCs may induce adverse effects in patients. Transfusion of stored, but not fresh, RBCs delivers an acute bolus of RBCs and RBC-derived iron to the monocyte/macrophage system resulting in oxidative stress and inflammatory cytokine secretion. Some of the macrophage-ingested iron is also released back into the circulation (ie, NTBI) where it can also cause oxidative damage and enhance bacterial proliferation. SIRS indicates systemic inflammatory response syndrome.
); P = .095 at 4 and 6 hours after transfusion comparing vehicle-treated and DFO-treated mice. (C) Proposed mechanistic pathway (the “iron hypothesis”) explaining how transfusion of older stored RBCs may induce adverse effects in patients. Transfusion of stored, but not fresh, RBCs delivers an acute bolus of RBCs and RBC-derived iron to the monocyte/macrophage system resulting in oxidative stress and inflammatory cytokine secretion. Some of the macrophage-ingested iron is also released back into the circulation (ie, NTBI) where it can also cause oxidative damage and enhance bacterial proliferation. SIRS indicates systemic inflammatory response syndrome.
DFO treatment decreases the proinflammatory response induced by transfusion of stored RBCs. (A) Mice were pretreated with a PBS vehicle control (n = 28) or with 3 mg of DFO, with (n = 15) or without (n = 31) the addition of equimolar ferric citrate, immediately before transfusion with stored RBCs (400 μL). Mice were killed 2 hours after transfusion, and plasma cytokine levels were measured; *P < .05; **P < .01; ***P < .001 compared with mice infused with PBS vehicle and transfused stored RBCs. (B) Bioluminescence was quantified for 24 hours after transfusion over the hepatosplenic region of SAA1-luciferase reporter mice transfused with 200 μL of fresh RBCs (n = 3;  ), the PBS vehicle control and stored RBCs (n = 3; ■), or 3 mg of DFO and stored RBCs (n = 6;
), the PBS vehicle control and stored RBCs (n = 3; ■), or 3 mg of DFO and stored RBCs (n = 6;  ); P = .095 at 4 and 6 hours after transfusion comparing vehicle-treated and DFO-treated mice. (C) Proposed mechanistic pathway (the “iron hypothesis”) explaining how transfusion of older stored RBCs may induce adverse effects in patients. Transfusion of stored, but not fresh, RBCs delivers an acute bolus of RBCs and RBC-derived iron to the monocyte/macrophage system resulting in oxidative stress and inflammatory cytokine secretion. Some of the macrophage-ingested iron is also released back into the circulation (ie, NTBI) where it can also cause oxidative damage and enhance bacterial proliferation. SIRS indicates systemic inflammatory response syndrome.
); P = .095 at 4 and 6 hours after transfusion comparing vehicle-treated and DFO-treated mice. (C) Proposed mechanistic pathway (the “iron hypothesis”) explaining how transfusion of older stored RBCs may induce adverse effects in patients. Transfusion of stored, but not fresh, RBCs delivers an acute bolus of RBCs and RBC-derived iron to the monocyte/macrophage system resulting in oxidative stress and inflammatory cytokine secretion. Some of the macrophage-ingested iron is also released back into the circulation (ie, NTBI) where it can also cause oxidative damage and enhance bacterial proliferation. SIRS indicates systemic inflammatory response syndrome.
The effect of DFO could be attributed to either its iron chelating capacity or to other antioxidative properties it may possess, such as its ability to scavenge the hydroxyl radical,30 or to both. Thus, control experiments were performed by infusing FO (ie, FO, an equimolar combination of DFO and ferric citrate) followed by transfusion of stored RBCs (Figure 7A). In this setting, FO was as effective as DFO at ameliorating the cytokine response.
Discussion
The major conclusions derived from the current studies with mice are that transfusions of RBCs after prolonged storage induce a proinflammatory response, are associated with increased circulating NTBI levels, and lead to increased iron deposition in various tissues. The lack of a proinflammatory response to transfusions of either membrane ghosts or stroma-free lysate derived from stored RBCs suggests that membrane-encapsulated hemoglobin is required to produce inflammation. The dramatic hemoglobinemia observed with transfusion of stroma-free RBC lysate (Figure 3A) did not result in an inflammatory cytokine response, suggesting that intravascular hemolysis is not responsible for this effect; rather extravascular hemolysis by macrophage-mediated phagocytosis is implicated. In addition, intact washed stored RBCs, but not the associated supernatant, induced this cytokine response; therefore, transfusion of compounds accumulating in the supernatant during storage (eg, cytokines, RBC-derived vesicles, cell-free hemoglobin, bioactive lipids, NTBI, etc) was not responsible. The transfusion of stored RBCs also synergizes with LPS to exacerbate and prolong cytokine storm. Finally, measuring bacterial growth in vitro suggests that the increased circulating iron released by clearance of transfused stored RBCs (ie, NTBI) increases bacterial proliferation. Thus, we propose the “iron hypothesis” model (Figure 7C) to explain the mechanisms underlying these adverse effects of stored RBC transfusions.
Although all RBC units used for transfusion were cultured after storage and no bacterial growth was detected, they were not tested for LPS contamination. The possibility of low-level bacterial contamination also exists. However, infusing supernatant or stroma-free lysate derived from stored RBC did not induce a cytokine response. In addition, injection of LPS alone induces a different cytokine profile (Figure 5). Therefore, the results obtained by transfusing stored RBCs or washed stored RBCs were probably not because of inadvertent LPS or bacterial contamination during RBC collection and processing; rather, the results were due to the transfused stored RBCs themselves.
Studies from the 1960s31,32 suggest that erythrophagocytosis in mice by either antibody-mediated RBC clearance, phenylhydrazine treatment, or clearance of xenogeneic RBCs, are each associated with an increased susceptibility to sepsis induced by various bacterial species, including E coli. The mechanism for this effect was not elucidated at the time, but may now be potentially explained by the ferrophilia of these organisms33 and the dramatic rise in circulating NTBI levels after RBC clearance as seen in our model of RBC storage and transfusion.
In recent studies with another murine transfusion model, prolonged storage of RBCs before transfusion into endotoxinemic mice caused increases in lung chemokines, neutrophils, and microvascular permeability.34 Similar to our findings, this response was related to the RBCs themselves, as washing of the stored RBCs pretransfusion did not abrogate the response. It is possible that the exacerbation of the existing lung inflammation seen in this model34 may also involve increased NTBI levels after transfusion of stored RBCs. For example, when excess plasma iron is not sequestered by transferrin, the NTBI can participate in redox reactions leading to oxidative damage, cytotoxicity, and enhanced expression of endothelial adhesion molecules.35,36 Thus, NTBI may act as another pathologic factor in this lung injury model.
The finding that both DFO, a nonmembrane permeable chelator, and its iron-chelated form, FO, inhibit the cytokine response induced by transfusion of stored RBCs to a similar extent (Figure 7) may be because of the antioxidant properties of DFO.30 Indeed, a similar effect was seen when LPS-challenged mice were treated with DFO or FO; both reduced TNF-α levels to a similar extent.30 Reactive oxygen species can mediate cytokine production by activating transcription factors, such as nuclear factor–κB37,38 ; therefore, it is possible that reactive oxygen species produced after clearance of stored RBCs are responsible for the proinflammatory response and that DFO and FO ameliorate this pro-oxidant effect. The role of free intracellular iron, released by processing of the ingested RBCs, in producing these putative reactive oxygen species remains to be determined. The lack of a statistically significant effect of DFO on SAA1 levels may be a result of variation in genetic background. The SAA1-luciferase transgenic mice are on the BALB/c background, whereas all other recipients in this study are on the C57BL/6 background. Additional studies are required to assess the effect of mouse strain on the inflammatory response to transfusions of older, stored RBCs.
We previously reported that immunoglobulin G (IgG) antibody-mediated RBC clearance induces cytokine storm in a mouse model of incompatible RBC transfusion.23 The same cytokine pattern was seen after transfusion of either stored RBCs or incompatible RBCs; however, the cytokine response in the former case is not as profound. Therefore, it is possible that Fcγ receptor-mediated signaling, which is involved in clearance of IgG-coated RBCs, amplifies the cytokine response in the incompatible transfusion model.39,–41 Future studies will focus on elucidating the mechanisms involved in RBC clearance and cytokine production after transfusion of stored RBCs.
In conclusion, the current murine RBC storage and transfusion model provides evidence that transfusion of older stored RBCs produces a proinflammatory response that is associated with increased levels of tissue iron in the liver, spleen, and kidney, and increased circulating levels of NTBI. This suggests that the pro-oxidant effects of iron released after acute clearance of stored RBCs may be responsible for some of the harmful effects of RBC transfusion after prolonged storage. In addition, the presence of increased plasma NTBI levels provides a possible explanation for the increased risk of bacterial infection suggested by retrospective studies in humans after transfusion of stored RBCs.6,8,,–11 Preventing the pro-oxidant effects of iron derived by rapid clearance of transfused stored RBCs may decrease these adverse effects. Although retrospective studies suggest that there is an increased rate of morbidity and mortality associated with the transfusion of older, stored RBCs, this increase has not been definitively proven in randomized prospective studies. The findings using this mouse model of RBC storage suggest that there are adverse effects to transfusing older, stored RBC products in mice; however, differences in storage procedures and the inherent limitations of animal models do not warrant a change in human transfusion practice at this time. Nonetheless, the findings obtained using this mouse model may be explained by the iron hypothesis presented (Figure 7C), which may also be relevant for explaining the adverse effects seen in humans transfused with older, stored RBCs, if these findings are confirmed by prospective human studies.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We express our gratitude to Dr Yaacov Hod and Dr Michael Shelanski for support and encouragement and to Dr Ljiljana Vasovic for drawing the figure of the mechanistic model.
This work was supported in part by grants from the National Institutes of Health (R21 HL089164, J.C.Z.; R37 DK049108, R01 DK066251, and DK069373, G.M.B.; R21 HL087906, S.L.S.), and by a College of American Pathologists Foundation Scholar Research Fellowship (E.A.H.).
National Institutes of Health
Authorship
Contribution: E.A.H., J.E.H., J.C.Z., G.M.B., and S.L.S. conceived the underlying model and iron hypothesis, and controlled and analyzed the data; all authors participated in designing and performing the research; N.Z., D.A., and K.P.F. performed the in vivo imaging experiments; S.A.S. and B.S.W. assisted in mouse experiments and performed cytokine and iron-related assays; P.D.-L. and S.W. designed and assisted with the in vitro bacterial growth experiments; S.S. designed and assisted with the iron chelation experiments; E.A.H. and R.O.F. performed the liposome experiments; E.A.H. wrote the paper; and all authors edited drafts and reviewed the final version of the manuscript.
Conflict-of-interest disclosure: N.Z., D.A., and K.P.F. are employed by Caliper Life Sciences. The remaining authors declare no competing financial interests.
Correspondence: Eldad A. Hod, Department of Pathology and Cell Biology, College of Physicians & Surgeons, Columbia University, 630 West 168th St, New York, NY 10032; e-mail: eh2217@columbia.edu.


![Figure 3. Transfusion of stored RBCs induces dose-responsive proinflammatory cytokine responses. (A) Hemoglobinemia, as detected by absorbance, was observed in all mice (n = 8) transfused with stroma-free lysate derived from stored RBCs. Representative spectra of plasma (diluted 1:4 with PBS) obtained from mice 2 hours after transfusion with fresh RBCs (< 24-hour storage), stored RBCs (2-week storage), or stroma-free lysate derived from stored RBCs are shown. (B) Untransfused C57BL/6 mice (n = 13) or mice transfused with fresh RBCs (1u = 200 μL, n = 5; [ie, 1 human equivalent unit = 200 μL]; 2u = 400 μL, n = 17), stored RBCs (1u = 200 μL, n = 5; 2u = 400 μL, n = 17), washed stored RBCs (400 μL; n = 13), stored RBC-derived supernatant (SN, 400 μL, n = 12), ghosts prepared from stored RBCs (400 μL, n = 8), and stroma-free lysate derived from stored RBCs (400 μL, n = 8) were killed 2 hours after transfusion, and plasma cytokine levels were measured (as labeled); *P < .05; **P < .01; ***P < .001 compared with fresh RBCs.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/115/21/10.1182_blood-2009-10-245001/5/m_zh89991052940003.jpeg?Expires=1767697454&Signature=klwzrQI2UWCFvxJ0GP6Ta4203htznZE~JcW5~eMVZg3U8Wo2ke6P8m8m8E0usLQWVZauKOaxFoGh-rLcKmarSdodqt5LWbv6mSlzC7SLHMaGOg9G0QyIirYJ~kCpAx~vKVWU0nUQupppBRSuQF0MDJBbo70BWmMEg-BFV5rKM8iyO9IRNLu47W1goCgcYeGq02DzBsCqhhg34w489AMt8hTN0GyiuPEMIubW7NmhcfiNLDKVgPYCQLBBktzFFoNBH1txTlh5WOz4TQtTGuomDCVeexDuvGc~7FyLLdTMl7h8Vt~r5bMiV2VS884MqhQD~jnzYTNokhS1fLw02TiahQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal