A 75-year-old woman with a 7-year history of chronic lymphocytic leukemia (CLL), previously treated with fludarabine and cyclophosphamide, was admitted with weight loss, night sweats, and fevers. She had widespread low-volume lymphadenopathy and a palpable spleen but no new large nodal mass. The complete blood count showed hemoglobin 112 g/L, white blood cell count 11.92 × 109/L, lymphocytes 10.73 × 109/L, and platelets 67 × 109/L. Two weeks later, her white cell count had risen to 92 × 109/L, and platelet count had fallen to 22 × 109/L. Her LDH was 3859 U/L. She died shortly thereafter.
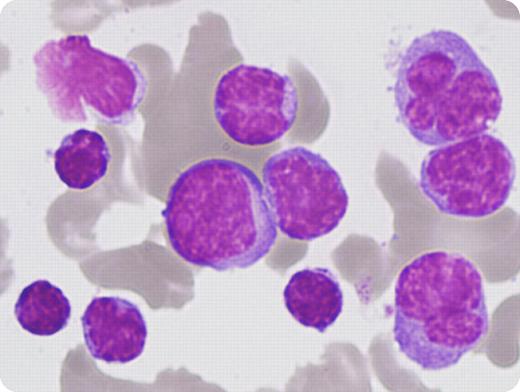
Her blood film showed 2 separate populations of lymphocytes. The first were small with clumped chromatin and scanty cytoplasm, typical of CLL cells. The second were larger pleomorphic cells with abundant, vacuolated cytoplasm and distinct nucleoli (see image). Flow cytometry affirmed the small lymphocyte population, consistent with her known CLL: coexpression of CD19, CD20, CD5, CD23, dim κ chain restriction, and negative for FMC7, CD79b, and CD22. However, the larger cell population was positive for FMC7, CD79b, and CD22 with strong expression of kappa and CD20. These findings confirmed a leukemic Richter transformation.
Richter transformation can occur in up to 10% of patients with CLL. It is heralded by a sudden clinical deterioration characterized by a rapid increase in lymphadenopathy, extranodal involvement, splenomegaly, worsening “B” symptoms, and rapid rise in LDH. The prognosis is very poor and therapeutic options are limited.
A 75-year-old woman with a 7-year history of chronic lymphocytic leukemia (CLL), previously treated with fludarabine and cyclophosphamide, was admitted with weight loss, night sweats, and fevers. She had widespread low-volume lymphadenopathy and a palpable spleen but no new large nodal mass. The complete blood count showed hemoglobin 112 g/L, white blood cell count 11.92 × 109/L, lymphocytes 10.73 × 109/L, and platelets 67 × 109/L. Two weeks later, her white cell count had risen to 92 × 109/L, and platelet count had fallen to 22 × 109/L. Her LDH was 3859 U/L. She died shortly thereafter.
Her blood film showed 2 separate populations of lymphocytes. The first were small with clumped chromatin and scanty cytoplasm, typical of CLL cells. The second were larger pleomorphic cells with abundant, vacuolated cytoplasm and distinct nucleoli (see image). Flow cytometry affirmed the small lymphocyte population, consistent with her known CLL: coexpression of CD19, CD20, CD5, CD23, dim κ chain restriction, and negative for FMC7, CD79b, and CD22. However, the larger cell population was positive for FMC7, CD79b, and CD22 with strong expression of kappa and CD20. These findings confirmed a leukemic Richter transformation.
Richter transformation can occur in up to 10% of patients with CLL. It is heralded by a sudden clinical deterioration characterized by a rapid increase in lymphadenopathy, extranodal involvement, splenomegaly, worsening “B” symptoms, and rapid rise in LDH. The prognosis is very poor and therapeutic options are limited.
Many Blood Work images are provided by the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas images and images of case studies. For more information or to contribute to the Image Bank, visit www.ashimagebank.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal