Abstract
One of the more insidious outcomes of patients who survive severe sepsis is profound immunosuppression. In this study, we addressed the hypothesis that post septic immune defects were due, in part, to the presence and/or expansion of regulatory T cells (Tregs). After recovery from severe sepsis, mice exhibited significantly higher numbers of Tregs, which exerted greater in vitro suppressive activity compared with controls. The expansion of Tregs was not limited to CD25+ cells, because Foxp3 expression was also detected in CD25− cells from post septic mice. This latter group exhibited a significant increase of chromatin remodeling at the Foxp3 promoter, because a marked increase in acetylation at H3K9 was associated with an increase in Foxp3 transcription. Post septic splenic dendritic cells promoted Treg conversion in vitro. Using a solid tumor model to explore the function of Tregs in an in vivo setting, we found post septic mice showed an increase in tumor growth compared with sham-treated mice with a syngeneic tumor model. This observation could mechanistically be related to the ability of post septic Tregs to impair the antitumor response mediated by CD8+ T cells. Together, these data show that the post septic immune system obstructs tumor immunosurveillance, in part, by augmented Treg expansion and function.
Introduction
Sepsis is a growing health concern, which is responsible for approximately 250 000 deaths a year in the United States.1 Most patients who survive life-threatening systemic inflammatory response syndrome develop a sustained immunosuppressive state, referred to as compensatory anti-inflammatory response syndrome. It is becoming clear that compensatory anti-inflammatory response syndrome is actually a protracted immunosuppressive state in post septic patients, which may last for years.2 The immunoregulation in these patients is associated with both the inability to eradicate a primary infection and the development of new secondary infections.3 The question remains: why does “immunoparalysis” persist in the post septic immune system?
Experimental polymicrobial sepsis is characterized by dysfunction of dendritic cells (DCs),3 monocytes,4 and T lymphocytes5 during both phases of the response syndrome. Recent experiments have focused on understanding the presence and function of regulatory T cells (Tregs) during experimental and clinical sepsis.6,7 An increased percentage of Tregs has been observed in the circulation of patients with septic shock, and the persistence of increased Tregs has been associated with a poor long-term prognosis.7 Thus, the role of Tregs during and after sepsis needs fuller exploration.
The transcription factor Foxp3 is a specific lineage marker for Tregs in mice, which is known to be a key regulator of Treg-cell development, survival, and function.8 Importantly, there is evidence that naive/conventional CD4+CD25−Foxp3− cells convert extrathymically into regulatory Foxp3+ T cells under certain conditions, including those associated with tumor development,9 the intestinal immune system,10 and in the allergic lung.11 The mechanisms driving the conversion of Tregs under homeostatic or pathogenic conditions has been extensively studied, and the secretion of cytokines, especially interleukin-10 (IL-10), by DCs have an important role in the differentiation of CD4+ T cells into Tregs.12 One consequence of Treg conversion involves epigenetic regulation of the Foxp3 promoter.13 In fact, the Foxp3 promoter showed a stronger association with acetylated histones in Tregs than in conventional T cells, suggesting that the Foxp3 promoter is readily accessible for activation in Tregs.14,15
The primary aim of this study was to examine Treg expansion/conversion in the post septic immune system. We observed that Tregs from mice at days 3 and 15 after sepsis exerted stronger suppressive activity compared with controls. More importantly, at day 15 after surgery the expansion of Foxp3+ Tregs was not limited to cells expressing high levels of CD25, because Foxp3 expression was present in a population of CD4+ T cells, which did not express CD25. This was mechanistically due, in part, to acetylation of H3K9 associated with the Foxp3 promoter. In vitro experiments showed that post septic splenic DCs significantly enhanced the conversion of naive CD4+Foxp3− into a Foxp3+ T-cell subset compared with controls DCs. Further, the consequences of the impaired immune response after severe sepsis was reflected by the failure of post septic mice to contain the development of an implanted carcinoma. In these mice, the tumor-draining lymph nodes (LNs) showed increased Tregs and lower perforin and interferon-γ (IFN-γ)–positive CD8+ T cells compared with controls. When either Tregs (Foxp3eGFP) from post septic or sham-treated mice were transferred into Rag−/− mice with naive CD8+ T cells, the presence of post septic but not control Tregs resulted in significantly greater tumor growth. Together, these results provide novel insights into the mechanisms by which post septic Tregs expand and contribute to the suppressive immune environment after severe sepsis.
Methods
Mice
C57BL/6 mice (6-8 weeks old) were purchased from Taconic Company. Breeding pairs of Foxp3 eGFP reporter mice (Foxp3eGFP) were purchased from The Jackson Laboratory and bred in-house. B6.129S7-Rag1tm1Mom/J (Rag1−/−) mice were obtained from The Jackson Laboratory. All animal protocols were approved by a UCUCA committee at the University of Michigan.
Polymicrobial sepsis
Severe sepsis was induced by cecal ligation and puncture (CLP) as previously described in detail.16 The survival rate in this model was 50% to 60%. Antibiotic treatment was required in the model, because 90% to 100% mortality was observed at 72 hours without antibiotic therapy. Given this mortality profile, we chose to analyze the characteristics of Tregs at days 1 (the peak of peritoneal inflammation), 3 (at the peak of systemic inflammation), and 15 (after several days of recovery).
Cell-surface and intracellular staining for T cells
Spleen and LN suspensions were incubated with anti-CD16/32 (2.4G2) and further labeled with fluorescent dye–conjugated mAb (CD4, RM4-5; CD3, 145-2C11; CD25, 7D4; GITR, DTA-1; CTLA-4, UC10-4F10-11; CD103, M290; all from BD Biosciences; CD8, 53-6.7; eBioscience). After the staining of surface markers, the cells were fixed, permeabilized, and stained for intracellular Foxp3, perforin (FJK-16s; eBioOMAK-D; eBioscience), and bromodeoxyuridine (BrdU; Chemicon International). For intracellular staining of IFN-γ, single suspensions of draining tumor LNs from either sham-treated or post septic mice were cultured in plate-bound anti-CD3 (2.5 μg/mL) and soluble anti-CD28 (1 μg/mL). After incubation with GolgiPlug, the cells were stained for surface markers (CD3 and CD8), resuspended in fixation/permeabilization solution (BD Cytofix/Cytoperm Kit; BD Biosciences PharMingen), and stained with anti–IFN-γ (XMG1.2; BD PharMingen). Samples were acquired on a LSRII machine with the use of FACSDiva software (BD Biosciences). Data were analyzed with FlowJo software (TreeStar).
Cytokine assays
Cytokines or chemokines from supernatants of in vitro culture assays and tumor homogenates were measured with the use of a Bio-Plex System and Suspension Array Technology (Bio-Rad).
RNA isolation and quantitative TaqMan analysis
CD4+CD25− splenic T cells undergoing fluorescence-activated cell sorting (FACS) from sham and CLP mice were homogenized in TRIzol (Invitrogen) or the RNeasy Mini Kit (QIAGEN) according to the manufacturer's directions. Total RNA was reverse-transcribed to yield cDNA with the use of routine techniques or SuperScript III First-Strand Synthesis System for reverse transcription–polymerase chain reaction (PCR; Invitrogen). Transcript levels of Foxp3, Kat2a (Gcn5), Kat5 (TIP60), and Kat2b (PCAF; Applied Biosystems) were determined by real-time quantitative PCR analysis with the use of a 7500 Real-Time PCR System (Applied Biosystems).
BrdU incorporation for the determination of Treg proliferation
Twenty hours before surgery, sham and CLP mice were given drinking water containing 0.8 mg/mL BrdU (Sigma-Aldrich), which was made fresh daily. At 48 hours, the animals were injected intraperitoneally with BrdU at a concentration of 1 mg per mouse. At day 3 after surgery, splenic lymphocytes from both groups of mice were stained for surface markers (CD4 and CD25), intracellular BrdU, and Foxp3 expression.
Suppression assay
A Treg suppression assay was used with FACS-sorted CD4+CD25high cells from CLP or sham mice at days 1, 3, and 15 after surgery and naive spleens cells labeled with CFDA-SE (carboxyfluorescein diacetate succinimidyl ester; 0.5mM). The naive spleen CFDA-SE–labeled cells were stimulated with 2.5 μg/mL anti-CD3 mAb (145-2C11) and 1 μg/mL soluble anti-CD28 (37.51). The purity of CD4+CD25high and CD4+CD25− T-cell fractions was always greater than 95%. After 72 hours at incubation, the suppressive capacity was assessed by measuring the CFDA-SE dilution in naive T cells with the use of FACS.
Chromatin immunoprecipitation assay
Chromatin immunoprecipitation (ChIP) assay was performed as described previously by Wen et al3 with adaptation for T cells. Specific antibodies used in these experiments were acetyl histone H3(06-599) and H3K27me(07-452) from Millipore and H3K4me (ab8580), H3acetylK9, (ab4441), and H4acetylK12 (ab1761) from Abcam or control normal rabbit immunoglobulin G (IgG). DNA was purified by standard phenol chloroform extraction and ethanol precipitation protocol17 and was analyzed by real-time PCR with the use of SYBR Green and the following primer pair (5′ to 3′ direction): Foxp3 (331 base pair) forward, GACTCAAGGGGGTCTCA, and reverse, TTGGGCTTCATCGGCAA.18
Dendritic cell, macrophage, and T-cell purification
Splenic CD11c+ cells were positively selected on an LS magnetic-activated cell sorting column; the cells that pass through the column (CD11c−) were collected and incubated with anti-CD11b microbeads (Miltenyi Biotec). CD11b+ cells were positively selected with the use of an LS magnetic-activated cell-sorting column. Positive selection of CD8α+ DCs was performed according to the manufacturer's instructions (Miltenyi Biotec).
Single-cell suspensions of spleens and LNs from Foxp3eGFP mice were enriched for CD4+ T cells by a negative selection after incubation with a mixture of specific biotin-conjugated mAbs (CD8, CD11b, CD11c, B220, NK1.1, and TER119; all from eBioscience) and antibiotin magnetic microbeads (5 μL/107 total cells; Miltenyi Biotec). The enriched fraction was further labeled with αCD4 and sorted on FACSVantage.
Naive CD8T cells used in the Rag−/− experiments were enriched for T cells by a negative selection with CD11b, CD11c, MHCII, and B220 microbeads (Miltenyi Biotec). The effluent cells were incubated with CD8 microbeads, and CD8+ T cells were positively selected according to the manufacturer's instructions. Approximately 95% of the cells were CD3+CD8+.
In vitro conversion
Conversion protocol was performed as previously described19 with T cells and DCs or macrophages obtained as described in “Dendritic cell, macrophage, and T-cell purification.” Briefly, FACS-purified CD4+ Foxp3− T cells were cocultured at a 1:2 ratio in complete medium under conditions favoring Treg generation, soluble α-CD3 (1 μg/mL; BD Biosciences) recombinant transforming growth factor-β (3 ng/mL), and 5 ng/mL IL-2 (both from R&D Systems) in cocultures every 2 days. In some experiments, 100 μg/mL blocking rabbit anti–IL-10 or control rabbit IgG was added on day 1. On day 5, cells were stained with αCD4 (RM4-5), αCD25 (PC61), and αFoxp3 and analyzed on an LSRII.
Tumor model
Lewis lung carcinoma (LLC) 0.5 × 106 cells were subcutaneously implanted into sham and post septic wild-type mice at day 15 after surgery. In experiments with Rag−/− mice, LLC cells were subcutaneously implanted at 16 hours after transfer of Foxp3eGFP T cells from sham or post septic mice. Tumor volume of each animal was measured after tumors were visible on the flanks. The formula for calculating tumor volume was V = [L × W2] × 0.52, where L is the tumor length and W is the tumor width.20
FACS-purified CD4+Foxp3eGFP cells (0.9 × 105) from spleens of sham and post septic mice were transferred intravenously into Rag−/− mice, and LLC tumor cells (0.5 × 106) were implanted subcutaneously 16 hours after transfer. Naive T CD8+ cells (2 × 105) were transferred alone or with Tregs. After T-cell reconstitution, mice were monitored for tumor volume as described earlier.
Statistical analysis
Statistical differences were calculated with the use of Prism 5 (GraphPad software), and a paired Student t test with P less than or equal to .05 was considered statistically significant.
Results
Characterization of CD4+CD25+ and CD4+CD25− T-cell populations during experimental septic peritonitis
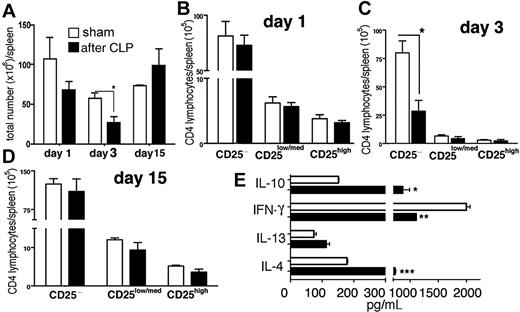
Septic peritonitis is characterized by an apoptotic response by T cells, particularly in the spleen.21,22 In this study, there was a statistically significant lower number of total spleens cells recovered from the CLP group than from the sham group at day 3 after surgery (Figure 1A). However, there was a major rebound in total spleen cell counts at day 15 after sepsis in CLP mice compared with the sham group. When CD4+ T-cell frequencies were determined according to their level of CD25 expression (ie, low, high, and negative) at day 1 (Figure 1B) and day 15 (Figure 1D), similar frequencies were noted; however, the CD4+CD25− cell numbers were significantly lower at day 3 in the septic group than in the control group (Figure 1C). These data suggest that, despite a major decline in total spleen cells after CLP and sham surgery at day 3, the CD25− T-cell numbers returned to baseline by day 15 and were identical between these groups.
Significant reduction of total spleen and CD4+CD25− T cells after sham or CLP surgery. Severe sepsis was induced in C57BL/6 mice by CLP. (A) Total spleen cell number from CLP and sham mice is shown. (B-D) With the use of flow cytometry, the lymphocytes were gated by forward (FSC) and side (SSC) scatter properties, and, then, the expression of CD4 and CD25 molecules were analyzed. CD4+ T cells are shown according to their expression level of CD25 at days 1, 3, and 15 after surgery. (E) CD4+CD25− T cells that underwent FACS from sham and CLP at day 3 after surgery were stimulated with polyclonal anti-CD3/CD28 for 72 hours, and the levels of IL-10, IFN-γ, IL-13, and IL-4 were measured in the supernatants of these cultures by Bioplex. *P ≤ .05; **P ≤ .01; ***P ≤ .001, compared with sham surgery. (A-D) Data represent mean ± SEM of 3 independent experiments (n = 3-5 mice in both groups), and (E) data show pooled results from 2 independent experiments.
Significant reduction of total spleen and CD4+CD25− T cells after sham or CLP surgery. Severe sepsis was induced in C57BL/6 mice by CLP. (A) Total spleen cell number from CLP and sham mice is shown. (B-D) With the use of flow cytometry, the lymphocytes were gated by forward (FSC) and side (SSC) scatter properties, and, then, the expression of CD4 and CD25 molecules were analyzed. CD4+ T cells are shown according to their expression level of CD25 at days 1, 3, and 15 after surgery. (E) CD4+CD25− T cells that underwent FACS from sham and CLP at day 3 after surgery were stimulated with polyclonal anti-CD3/CD28 for 72 hours, and the levels of IL-10, IFN-γ, IL-13, and IL-4 were measured in the supernatants of these cultures by Bioplex. *P ≤ .05; **P ≤ .01; ***P ≤ .001, compared with sham surgery. (A-D) Data represent mean ± SEM of 3 independent experiments (n = 3-5 mice in both groups), and (E) data show pooled results from 2 independent experiments.
Another aspect of T-cell biology that is affected after sepsis is cytokine generation. We next addressed the profile of cytokines that splenic CD4+CD25− T cells undergoing FACS generate at day 3 after sepsis, which was the time point when we observed the greatest drop in CD4+CD25− T cells in the CLP compared with the controls. Equivalent numbers of CD4+CD25− T cells from septic mice generated significantly less IFN-γ and significantly higher levels of IL-10 and IL-4 compared with CD4+CD25− T cells from controls (Figure 1E). Together these data confirmed that CD4+CD25− T cells were skewed toward T helper type 2 (Th2) and away from Th1 cytokine generation at day 3 after the induction of septic peritonitis.
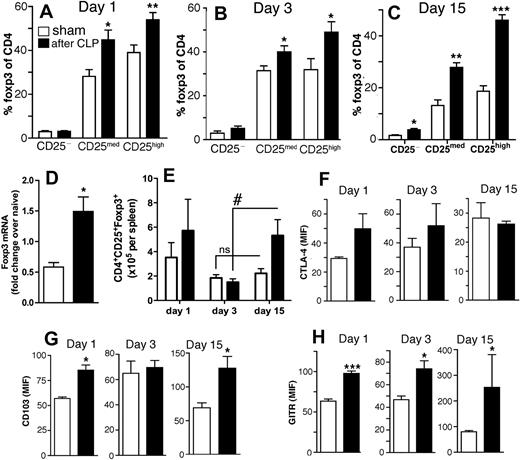
Increased frequency of Foxp3+ Tregs after the induction of severe sepsis
We next addressed the hypothesis that the immunosuppression after severe sepsis might be a consequence of altered numbers of CD4+Foxp3+ Tregs. At days 1 (Figure 2A), 3 (Figure 2B), and 15 (Figure 2C) after CLP, the percentage of splenic CD4+ cells expressing both Foxp3 and either moderate or high levels of CD25 was significantly increased in septic versus control mice. At day 15, post septic mice also exhibited an increased frequency of CD4+CD25− cells expressing Foxp3 (Figure 2C). TaqMan analysis confirmed that Foxp3 transcript expression by CD4+CD25− post septic (day 15) T cells was significantly increased above control/sham CD4+CD25− T cells when normalized to naive splenic CD4+CD25− T cells (Figure 2D). At days 1, 3, and 15, absolute numbers of splenic Tregs (CD4+CD25+Foxp3+) were evaluated. The absolute numbers of Tregs in septic mice dropped significantly at day 3 compared with baseline levels at day 1. However, by day 15 the numbers of splenic Tregs were increased significantly compared with day 3 post septic spleens, suggesting that these cells were expanded in the post septic environment. The absolute numbers of Tregs in sham mice were not significantly different at any time analyzed (Figure 2E).
Characterization of Foxp3-expressing CD4+CD25+ T cells after sham or CLP surgery. (A-C) Spleens from sham and CLP mice at days 1, 3, and 15 after surgery were stained for CD4, CD25, and Foxp3. The percentage of Foxp3-expressing CD4 T cells with various CD25 expression is shown. (D) CD4+CD25− T cells were sorted from spleens of sham and CLP mice. Foxp3 expression was assayed by quantitative PCR, normalized to GAPDH levels, and compared with naive CD4+CD25−-sorted cells. (E) Absolute numbers of CD4+CD25+Foxp3+ cells in spleens from sham and CLP mice. Combined data of 2 to 3 independent experiments and means ± SEM are shown. *P ≤ .05; **P ≤ .01; ***P ≤ .001 when CLP mice were compared with sham mice; #P ≤ .05 when CLP mice at day 3 were compared with CLP mice at day 15 after surgery. The levels (MFI) of (F) CTLA-4, (G) CD103, (H) GITR were analyzed in the population of CD4+CD25highFoxp3+ cells from spleens of sham and CLP mice at days 1, 3, and 15 after surgery. Data are representative of 2 independent experiments (n = 4-5 per group). *P ≤ .05; **P ≤ .01; ***P ≤ .001 when post septic mice were compared with sham mice.
Characterization of Foxp3-expressing CD4+CD25+ T cells after sham or CLP surgery. (A-C) Spleens from sham and CLP mice at days 1, 3, and 15 after surgery were stained for CD4, CD25, and Foxp3. The percentage of Foxp3-expressing CD4 T cells with various CD25 expression is shown. (D) CD4+CD25− T cells were sorted from spleens of sham and CLP mice. Foxp3 expression was assayed by quantitative PCR, normalized to GAPDH levels, and compared with naive CD4+CD25−-sorted cells. (E) Absolute numbers of CD4+CD25+Foxp3+ cells in spleens from sham and CLP mice. Combined data of 2 to 3 independent experiments and means ± SEM are shown. *P ≤ .05; **P ≤ .01; ***P ≤ .001 when CLP mice were compared with sham mice; #P ≤ .05 when CLP mice at day 3 were compared with CLP mice at day 15 after surgery. The levels (MFI) of (F) CTLA-4, (G) CD103, (H) GITR were analyzed in the population of CD4+CD25highFoxp3+ cells from spleens of sham and CLP mice at days 1, 3, and 15 after surgery. Data are representative of 2 independent experiments (n = 4-5 per group). *P ≤ .05; **P ≤ .01; ***P ≤ .001 when post septic mice were compared with sham mice.
Next, the expression of CTLA-4 (Figure 2F), CD103 (Figure 2G), and GITR (Figure 2H) was analyzed in CLP and sham Tregs (gated on CD4+CD25highFoxp3+) at days 1, 3, and 15 after surgery. We observed that Tregs from CLP mice expressed higher levels of characteristic costimulatory T-cell proteins regulated by Foxp3 expression (ie, CTLA-4 and GITR) and CD103, a molecule known to be associated with the retention of these cells in tissues.23-25
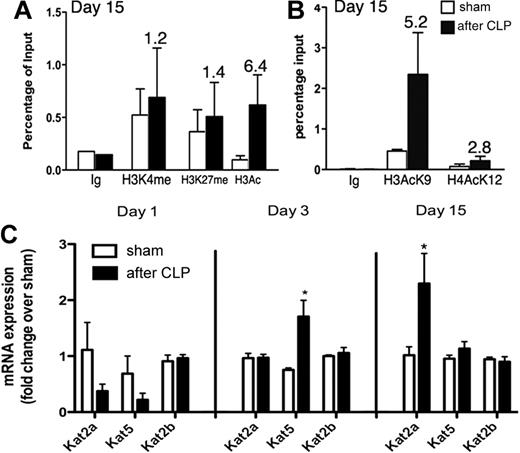
Histone acetylation has been shown to be associated with increased gene transcription in several nonimmune and immune settings.26 Given the increased expression of Foxp3 in the CD4+CD25− T-cell population, we next hypothesized that epigenetic alterations might provide a mechanism for Foxp3 expression in conventional T cells from post septic mice. Therefore, we examined the histone acetylation and methylation status of the Foxp3 promoter with the use of a ChIP assay of FACS-purified CD4+CD25− T cells from sham and post septic mice (Figure 3). As shown in Figure 3A, no differences between the groups were found in the methylation status of H3K27 (a chromatin mark that silences gene expression) and H3K4 (a chromatin mark that augments gene expression) at the Foxp3 promoter. However, histone acetylation at H3K9 (a chromatin mark that augments gene expression), but not at H4K12, associated with the Foxp3 promoter was considerably greater in post septic CD4+CD25− T cells compared with control sham mice (Figure 3B). We next analyzed the acetyltransferases that regulate H3K9 (ie, Kat2a, Kat2b) and H4 histones (Kat5). The expression of Kat2a, Kat5, and Kat2b were analyzed in FACS-puripied CD4+CD25− T cells at day 1, 3, and 15 after surgery (Figure 3C). Our data indicated an up-regulation of Kat5 at day 3 after surgery and an up-regulation of Kat2a expression at day 15 in post septic animals. Together, these results show that the Foxp3 promoter site is actively acetylated at H3K9 in CD4+CD25− T cells from mice recovered from sepsis, which could serve as a mechanism for the increased Foxp3 expression/conversion in this T-cell population.
Up-regulation of H3K9 acetylation in Foxp3 promoter CD4+CD25− T cells from post septic mice. (A) To determine histone acetylation and methylation status at the promoter region of Foxp3, ChIP assay was performed with 1.5 × 106 FACS-purified CD4+CD25− T cells from post septic and sham mice at day 15 after surgery. (B) ChIP assay was performed with 1.5 × 106 FACS-purified CD4+CD25− T cells from post septic and sham at day 15 after surgery to determine histone acetylation at H3K9 and H4K12. Numbers above bars indicate the fold change of enrichment after immunoprecipitation (IP) in post septic versus sham mice. Data are representative of 2 independent experiments (average and SEM; n = 4 mice per group). (C) mRNA expression of Kat2a, Kat5, and Kat2b in CD4+CD25− T cells from sham and post-CLP groups at day 1, 3, and 15 after surgery. Data from days 1 and 3 are the mean ± SEM from 6 mice in each group (2 spleens pooled at each time point). Data from day 15 are the mean ± SEM from 2 independent experiments (n = 6 for sham, n = 8 for post septic mice). *P ≤ .05, when post septic mice were compared with sham mice.
Up-regulation of H3K9 acetylation in Foxp3 promoter CD4+CD25− T cells from post septic mice. (A) To determine histone acetylation and methylation status at the promoter region of Foxp3, ChIP assay was performed with 1.5 × 106 FACS-purified CD4+CD25− T cells from post septic and sham mice at day 15 after surgery. (B) ChIP assay was performed with 1.5 × 106 FACS-purified CD4+CD25− T cells from post septic and sham at day 15 after surgery to determine histone acetylation at H3K9 and H4K12. Numbers above bars indicate the fold change of enrichment after immunoprecipitation (IP) in post septic versus sham mice. Data are representative of 2 independent experiments (average and SEM; n = 4 mice per group). (C) mRNA expression of Kat2a, Kat5, and Kat2b in CD4+CD25− T cells from sham and post-CLP groups at day 1, 3, and 15 after surgery. Data from days 1 and 3 are the mean ± SEM from 6 mice in each group (2 spleens pooled at each time point). Data from day 15 are the mean ± SEM from 2 independent experiments (n = 6 for sham, n = 8 for post septic mice). *P ≤ .05, when post septic mice were compared with sham mice.
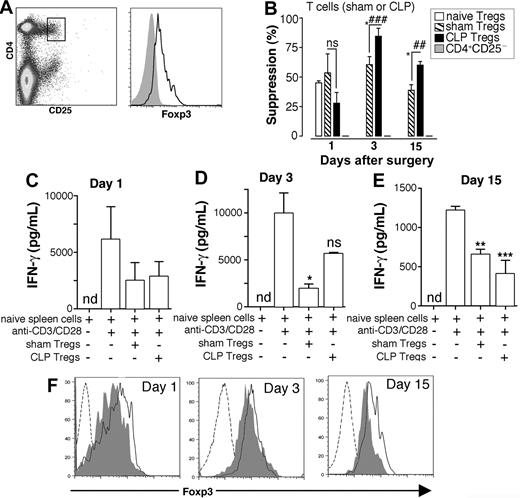
Treg function after sepsis
We next examined the capacity of FACS-purified CD4+CD25high T cells (shown in Figure 4A) from either sham or post septic mice to suppress the proliferative responses of naive CD4+ T cells after polyclonal activation.27 The magnitude of the regulatory activity of anti-CD3/CD28–stimulated naive T cells by either sham or CLP Tregs is shown in Figure 4B. At day 1 after surgery, the activity of Tregs from both groups was not statistically different, but Tregs from CLP mice at days 3 and 15 after surgery exhibited significantly greater suppressive activity compared with Tregs isolated from sham or naive mice. No suppressive effect was observed when CD4+CD25− T cells from sham and CLP were added in these cocultures (Figure 4B).
Suppressive properties of Tregs in post septic mice. (A) Representative CD4+CD25high cells used in suppression assays. Before coculture, Tregs were analyzed by FACS for intracellular Foxp3 expression (black line); isotype control (gray line). (B) CD4+CD25high T cells were isolated by FACS from the spleens of naive, sham, and CLP mice, and their suppressive capacities were tested in vitro. CD4+CD25− T cells from all groups that underwent FACS were cocultured with naive T cells as a control for the assay. CFDA-SE–labeled cells were examined by flow cytometry, and the magnitude of suppression of CFDA-SE–labeled naive T cells stimulated with anti-CD3/CD28 was calculated with the use of FlowJo software. The graphs represent mean ± SEM of the combined results from 2 to 3 experiments (for sham and CLP at 1, 3, and 15 days after surgery) and 2 independent experiments (for naive mice). #P ≤ .05; ###P ≤ .001 when the suppression activity of post septic Tregs was compared with naive Tregs. *P ≤ .05 and **P ≤ .01 when the suppression activity of post septic Tregs was compared with sham Tregs. (C-E) IFN-γ levels were analyzed in supernatants from cocultures. Data are mean ± SEM of results from 3 independent experiments at each time point. *P ≤ .05 compared with naive T-cell proliferation. (F) Cells from spleens of mice were analyzed for Foxp3 expression. Histogram plots were gated on CD4+CD25high cells, and the mean of fluorescence intensity (MFI) of Foxp3 was analyzed. Control isotype (dashed line), sham (gray area), and post septic (black line). Representative histograms are shown for 3 independent experiments with 3 to 4 mice per group.
Suppressive properties of Tregs in post septic mice. (A) Representative CD4+CD25high cells used in suppression assays. Before coculture, Tregs were analyzed by FACS for intracellular Foxp3 expression (black line); isotype control (gray line). (B) CD4+CD25high T cells were isolated by FACS from the spleens of naive, sham, and CLP mice, and their suppressive capacities were tested in vitro. CD4+CD25− T cells from all groups that underwent FACS were cocultured with naive T cells as a control for the assay. CFDA-SE–labeled cells were examined by flow cytometry, and the magnitude of suppression of CFDA-SE–labeled naive T cells stimulated with anti-CD3/CD28 was calculated with the use of FlowJo software. The graphs represent mean ± SEM of the combined results from 2 to 3 experiments (for sham and CLP at 1, 3, and 15 days after surgery) and 2 independent experiments (for naive mice). #P ≤ .05; ###P ≤ .001 when the suppression activity of post septic Tregs was compared with naive Tregs. *P ≤ .05 and **P ≤ .01 when the suppression activity of post septic Tregs was compared with sham Tregs. (C-E) IFN-γ levels were analyzed in supernatants from cocultures. Data are mean ± SEM of results from 3 independent experiments at each time point. *P ≤ .05 compared with naive T-cell proliferation. (F) Cells from spleens of mice were analyzed for Foxp3 expression. Histogram plots were gated on CD4+CD25high cells, and the mean of fluorescence intensity (MFI) of Foxp3 was analyzed. Control isotype (dashed line), sham (gray area), and post septic (black line). Representative histograms are shown for 3 independent experiments with 3 to 4 mice per group.
In cocultures of Tregs and T effectors, the presence of Tregs had a major inhibitory effect of IFN-γ levels. At day 1 after surgery, Tregs recovered from each group appeared to equally inhibit IFN-γ production (Figure 4C). At day 3, the levels of IFN-γ in cocultures of T effectors and CLP Tregs were higher than that in cocultures of T effectors and sham Tregs (Figure 4D). However, at day 15 after surgery, IFN-γ levels were reduced by 67% (compared with cultures with activated T-effector cells alone) in cocultures containing CLP Tregs and reduced by 47% (using the same comparison) in cocultures containing sham Tregs (Figure 4E). The above data suggest that long-term immunosuppression in sepsis might involve the modulation of Treg activity and/or modulation of Th1 effector cytokine production.
Finally, we observed that the expression of Foxp3 in the CD4+CD25high T cells in post septic mice (day 15) was significantly greater compared with sham mice (mean fluorescence intensity [MFI], 359.5 ± 20.5 vs 275.3 ± 10.4, respectively; Figure 4F), suggesting that the increased expression of Foxp3 in Tregs from CLP mice contributes to the increased suppressive effect of these cells.
Post septic environment permits the de novo generation of Foxp3+ T cells
To determine whether the increased frequency of Tregs in CLP mice was related to proliferation or extrathymic differentiation of this population, sham and CLP mice were treated with BrdU. At day 3 after surgery, approximately 3.4 (±0.39) × 103 and 1.2 (±0.50) × 103 of splenic Tregs (CD4+Foxp3+) from sham and CLP mice, respectively, had incorporated BrdU (Figure 5A), indicating that the expansion of Tregs in septic mice was not due to proliferation but reflected, at least in part, de novo generation of peripheral Tregs.
Splenic DCs (CD11c+) from post septic mice potently induce Treg conversion. (A) Sham and post septic mice were administrated 0.8 mg/mL BrdU in the drinking water beginning 20 hours before the surgery, and at 48 hours the mice were injected intraperitoneally with 1 mg of BrdU per mouse. At day 3 after surgery, spleen cells were stained for CD4 and Foxp3, and the absolute numbers of CD4+Foxp3+BrdU+ cells were compared between sham and post septic groups from data obtained by flow cytometry. Data represent the mean ± SEM of 3 mice per group. *P ≤ .05, when sham mice are compared with post septic mice. (B-E) Naive CD4+Foxp3− T cells isolated from Foxp3eGFP mice underwent FACS and were cultured in Treg-polarizing conditions or not (ie, no transforming growth factor-β [TGF-β] served as negative control) with post septic or sham splenic DCs (CD11c+MHCII+ or CD8α+) or macrophages (CD11b+CD11c−). The percentage of converted CD4+Foxp3+ T cells is shown (B). (C) Dot plots gated on viable CD4+GFP+ T cells show Foxp3 expression (FJK-16s) after culture in the presence of splenic DCs CD11c+ from sham or post septic mice; numbers in the upper quadrants indicate percentages of CD4+Foxp3− and CD4+Foxp3+ T-cell populations. (D) Percentage of conversion was analyzed on viable CD4+ T cells, and this panel shows the Foxp3 expression in the presence of post septic or sham splenic DCs incubated with blocking anti–IL-10 or IgG control (both 100 μg/mL). All converted Tregs expressed CD25. Data shown are representative of 2 independent experiments (n = 3-5 mice per group) with similar results. Data using DCs (CD11c+) are representative of 3 independent experiments with similar results. (E) The measurement of IFN-γ, KC, and IL-17 by Bioplex on the supernatants derived from the cell-culture conditions are shown as described in panel B.
Splenic DCs (CD11c+) from post septic mice potently induce Treg conversion. (A) Sham and post septic mice were administrated 0.8 mg/mL BrdU in the drinking water beginning 20 hours before the surgery, and at 48 hours the mice were injected intraperitoneally with 1 mg of BrdU per mouse. At day 3 after surgery, spleen cells were stained for CD4 and Foxp3, and the absolute numbers of CD4+Foxp3+BrdU+ cells were compared between sham and post septic groups from data obtained by flow cytometry. Data represent the mean ± SEM of 3 mice per group. *P ≤ .05, when sham mice are compared with post septic mice. (B-E) Naive CD4+Foxp3− T cells isolated from Foxp3eGFP mice underwent FACS and were cultured in Treg-polarizing conditions or not (ie, no transforming growth factor-β [TGF-β] served as negative control) with post septic or sham splenic DCs (CD11c+MHCII+ or CD8α+) or macrophages (CD11b+CD11c−). The percentage of converted CD4+Foxp3+ T cells is shown (B). (C) Dot plots gated on viable CD4+GFP+ T cells show Foxp3 expression (FJK-16s) after culture in the presence of splenic DCs CD11c+ from sham or post septic mice; numbers in the upper quadrants indicate percentages of CD4+Foxp3− and CD4+Foxp3+ T-cell populations. (D) Percentage of conversion was analyzed on viable CD4+ T cells, and this panel shows the Foxp3 expression in the presence of post septic or sham splenic DCs incubated with blocking anti–IL-10 or IgG control (both 100 μg/mL). All converted Tregs expressed CD25. Data shown are representative of 2 independent experiments (n = 3-5 mice per group) with similar results. Data using DCs (CD11c+) are representative of 3 independent experiments with similar results. (E) The measurement of IFN-γ, KC, and IL-17 by Bioplex on the supernatants derived from the cell-culture conditions are shown as described in panel B.
Splenic DCs from the post septic animals generate high levels of IL-10 but low levels of IL-12 in response to Toll-like receptor agonists.3 Differential cytokine generation by DCs can promote the unique differentiation of Th1, Th2, Treg, or Th17 T-cell phenotypes, and this led us to explore whether an altered DC phenotype in the post septic host was responsible for the higher frequency of Tregs after sepsis. Splenic DCs (CD11c+, 70%-75% major histocompatibility complex type II–positive [MHCII+], and 40%-45% CD11b+), DCs (CD8a+), or macrophages (CD11b+CD11c−, < 4% were MHCII+) were isolated from sham and post septic mice at day 15 after surgery and cocultured with naive CD4+Foxp3−CD25− T cells for 5 days under Treg-polarizing conditions.19 As shown in Figure 5B and C, DCs (CD11c+) from sham and post septic mice converted the highest percentage of Tregs compared with other cell types in coculture. However, CD11c+ DCs from post septic mice converted significantly greater numbers of Tregs compared with CD11c+ DCs from sham surgery (Figure 5B-C). To determine whether IL-10 was involved in the increased conversion of Tregs by post septic DCs, a blocking antibody against IL-10 was added to cocultures. Immunoneutralization of IL-10 reduced the conversion of Tregs by DCs from both post septic and sham mice, only by approximately 10% (Figure 5D). Because of the greater Treg conversion, we also analyzed cytokine levels in supernatants of these T-cell/CD11c+ cocultures. Higher levels of T-effector cytokines IFN-γ, IL-17, and keratinocyte-derived cytokine (KC) were detected in the conversion assays that used DCs from sham mice than DCs from post septic mice, suggesting an antagonistic effect of Th1 development on Treg conversion28 (Figure 5E).
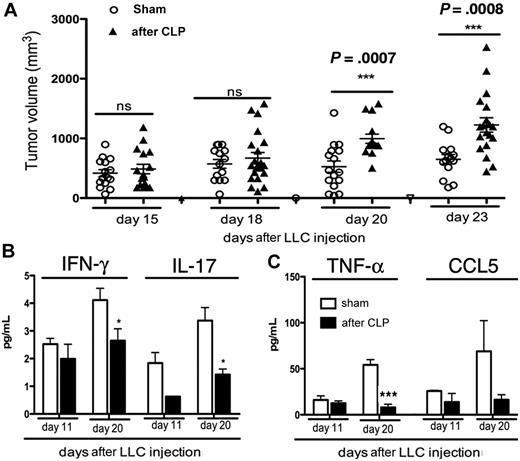
Increased tumor growth in post septic mice compared with sham surgery mice
To explore the function of Tregs from post septic mice in an in vivo setting, we next determined whether post septic mice exhibited enhanced tumor growth compared with sham mice. At day 15 after surgery, post septic and sham mice were subcutaneously implanted with syngeneic LLC cells on the dorsal flanks, and tumor growth was monitored for 23 days. As shown in Figure 6A, larger tumor volumes were observed in the post septic group at days 20 and 23 after tumor implantation. Similar findings were obtained with the use of B16F10 melanoma implantation (supplemental Figure 1A, available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
Severe sepsis impaired effective antitumor responses. (A) At day 15 post septic and sham mice were inoculated subcutaneously in the flank with 0.5 × 106 LLC cells, and tumor growth was monitored at various time points as indicated. Thus, day 15 is 30 days after CLP or sham surgery. Data shown are the results from 3 independent experiments. Horizontal lines indicate the comparison between sham and post-CLP mice at the indicated times after tumor injection. ns indicates not statistically significant. (B-C) IFN-γ, IL-17, TNF-α, and CCL5 were measured in tumor homogenates at days 11 and 20 after LLC injection with the use of Bioplex. (A) Pooled results from 3 independent experiments are shown. (B-C) Data represent the mean ± SEM from 5 to 7 individual mice per group. *P ≤ .05; ***P ≤ .001 when post septic mice were compared with sham mice bearing tumors.
Severe sepsis impaired effective antitumor responses. (A) At day 15 post septic and sham mice were inoculated subcutaneously in the flank with 0.5 × 106 LLC cells, and tumor growth was monitored at various time points as indicated. Thus, day 15 is 30 days after CLP or sham surgery. Data shown are the results from 3 independent experiments. Horizontal lines indicate the comparison between sham and post-CLP mice at the indicated times after tumor injection. ns indicates not statistically significant. (B-C) IFN-γ, IL-17, TNF-α, and CCL5 were measured in tumor homogenates at days 11 and 20 after LLC injection with the use of Bioplex. (A) Pooled results from 3 independent experiments are shown. (B-C) Data represent the mean ± SEM from 5 to 7 individual mice per group. *P ≤ .05; ***P ≤ .001 when post septic mice were compared with sham mice bearing tumors.
Examination of the immune response at the LLC tumor sites from sham and post septic mice showed marked changes in levels of IFN-γ, IL-17 (Figure 6B), tumor necrosis factor-α (TNF-α), and CCL5 (Figure 6C) at day 20 after LLC implantation. Although only IL-17 was lower at the day 11 time point after tumor implantation, all 4 factors were significantly lower at the day 20 time point when post septic groups were compared with sham groups.
To further address our hypothesis that the post septic immune system fails to contain tumor growth, mice were inoculated with LLC tumor at day 55 after CLP and sham surgeries. As shown in supplemental Figure 2, significantly larger tumor volumes were observed in the post septic group after tumor implantation.
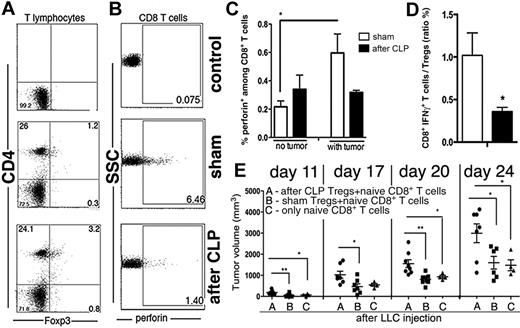
Post septic Tregs had a crucial role during tumor progression
At 23 days after carcinoma implantation, Tregs recovered from draining tumor LNs from post septic and sham surgery were analyzed. The percentage of Foxp3+ CD4 T cells was observed to be significantly higher in post septic mice compared with sham mice (P < .01) (Figure 7A). Similarly, we observed an increased expression of Foxp3 in draining LN CD4+CD25+ T cells from post septic mice implanted with melanoma compared with sham (supplemental Figure 1B). To further elucidate a mechanism that impaired the antitumor response in post septic mice, we evaluated the ability of CD8+ T cells to secrete perforin. CD8+ T cells from tumor-bearing post septic mice produced lower amounts of perforin than did those from sham mice bearing tumors (Figure 7B). However, the percentages of CD8+ T cells were similar in sham or post septic mice in the absence of tumor, suggesting that severe sepsis did not adversely affect the percentage of perforin+CD8+ T cells (Figure 7C). Finally, the ratio of CD8+T cells producing IFN-γ to Tregs was significantly decreased in post septic mice compared with sham mice (Figure 7D). These results suggested that Tregs might promote tumor growth by inhibiting antitumor responses mediated by CD8+ T cells expressing IFN-γ and perforin.
CD4+Foxp3+ Tregs from post septic mice suppress antitumor responses in vivo. The immune response in tumor-draining LNs from sham and post septic mice (at day 15 after surgery) was analyzed at day 23 after LLC injection. (A) Comparative assessment of proportion of Foxp3+ Treg cells in total viable CD4+ T-cell population. (B) Dot plots gated in viable CD8+ T cells were analyzed for the intracellular expression of perforin × side scatter (SSC) in tumor-draining LNs from post septic and sham mice bearing tumor or in LNs without tumor. (A-B) Numbers in quadrants indicate percentage of cell types. (C) CD8+ gated T cells were analyzed for the expression of perforin in peripheral LNs from post septic and sham mice without tumor implantation. (D) The ratio between tumor-draining LNs, Tregs, and CD8+T lymphocytes producing IFN-γ (analyzed after TCR stimulation with anti-CD3/28) was compared between the groups. (C-D) Data represent the mean ± SEM from 5 individual mice per group. (E) Naive CD8+ T cells (5 × 105) from C57BL/6 mice were transferred intravenously into C57BL/6 Rag−/− mice that 20 hours before were transferred with or without 0.9 × 105 CD4+ FoxP3+ from FoxP3−eGFP knock-in mice T cells isolated from post septic (A) or sham mice (B). After 16 hours, 0.5 × 106 LLC cells were subcutaneously injected, and the tumor measurements were performed at the indicated time points. Data are representative of 2 experiments with similar results. *P ≤ .05; **P ≤ .01 compared with sham Treg cells transferred in the presence of naive CD8+ T cells or only naive CD8+ T cells. No differences between the sham Tregs and CD8+ T cells or the CD8+ T-cell group alone were observed. Horizontal lines indicate comparison between panels A and B, and the comparison between panels A and C.
CD4+Foxp3+ Tregs from post septic mice suppress antitumor responses in vivo. The immune response in tumor-draining LNs from sham and post septic mice (at day 15 after surgery) was analyzed at day 23 after LLC injection. (A) Comparative assessment of proportion of Foxp3+ Treg cells in total viable CD4+ T-cell population. (B) Dot plots gated in viable CD8+ T cells were analyzed for the intracellular expression of perforin × side scatter (SSC) in tumor-draining LNs from post septic and sham mice bearing tumor or in LNs without tumor. (A-B) Numbers in quadrants indicate percentage of cell types. (C) CD8+ gated T cells were analyzed for the expression of perforin in peripheral LNs from post septic and sham mice without tumor implantation. (D) The ratio between tumor-draining LNs, Tregs, and CD8+T lymphocytes producing IFN-γ (analyzed after TCR stimulation with anti-CD3/28) was compared between the groups. (C-D) Data represent the mean ± SEM from 5 individual mice per group. (E) Naive CD8+ T cells (5 × 105) from C57BL/6 mice were transferred intravenously into C57BL/6 Rag−/− mice that 20 hours before were transferred with or without 0.9 × 105 CD4+ FoxP3+ from FoxP3−eGFP knock-in mice T cells isolated from post septic (A) or sham mice (B). After 16 hours, 0.5 × 106 LLC cells were subcutaneously injected, and the tumor measurements were performed at the indicated time points. Data are representative of 2 experiments with similar results. *P ≤ .05; **P ≤ .01 compared with sham Treg cells transferred in the presence of naive CD8+ T cells or only naive CD8+ T cells. No differences between the sham Tregs and CD8+ T cells or the CD8+ T-cell group alone were observed. Horizontal lines indicate comparison between panels A and B, and the comparison between panels A and C.
Adoptive transfer of post septic Tregs enhanced tumor growth
To further examine whether Tregs from post septic mice might be involved in the suppression of the antitumor immune response mediated by CD8+ T cells we adoptively transferred FACS-purified CD4+Foxp3+eGFP T cells isolated either from post septic or sham mice and naive magnetically sorted CD8+ T cells into Rag−/− mice. At 16 hours after Treg and CD8+ T-cell transfer, all mice were implanted subcutaneously in the flank with LLC cells. As shown in Figure 7E, adoptive transfer of post septic Tregs into Rag−/− mice impaired the antitumor response of CD8+ T cells, resulting in significantly large tumor volume compared with other Rag−/− tumor groups (Figure 7E). Transfer of sham Tregs with naive CD8+ T cells or the transfer of naive CD8+ T cells alone into Rag−/− mice resulted in similar tumor size (Figure 7E). These results again suggest that Tregs from post septic mice suppress the ability of CD8+ T cells to mount an effective antitumor response compared with control Tregs.
Discussion
Patients with severe sepsis develop a sustained immunosuppressive state, termed “immunoparalysis,” which manifests as a long-term inability to mount a fully functioning immune response.29-31 The chronic consequences linked to sepsis have also been noted in other severe human diseases, including ischemia/reperfusion after organ transplantation32 and severe burn injury.33 Although several investigators have studied the role of Tregs acutely after experimental sepsis,6,34,35 little is known about the characteristics of these cells in sepsis survivors. For this reason, we focused on the post septic immune system, particularly its efficiency in antitumor responses, with specific emphasis on the function of these cells in an in vivo setting. In the present study, we used a model of severe sepsis in which antibiotic therapy and fluid resuscitation was absolutely necessary for mouse survival. We confirmed that there was a transient but significant decrease in absolute numbers of conventional T cells and Tregs at day 3 after CLP surgery compared with sham surgery. This finding was consistent with the well-described finding that apoptosis occurs in the CD4+ T-cell population during sepsis.21 Importantly, the absolute numbers of Tregs increased significantly at day 15 compared with day 3 in post septic mice. We observed that a higher percentage of Foxp3+ cells were present in post septic mice, and this increase in Foxp3 was not limited to cells with the CD25 expression but was also found in CD25med/low and in CD4+ T cells that were CD25−. These last findings raised the possibility of the existence of a prelineage of Tregs and/or de novo generation of this population in mice that survive severe sepsis. This hypothesis was supported by 3 pieces of evidence: (1) increased histone acetylation in the Foxp3 promoter of CD4+CD25− T cells, which might be associated with increased gene transcription26 ; (2) BrdU experiments showed that the expansion of peripheral Tregs from post septic mice was not due to proliferation; and (3) CD11c+ DCs from post septic mice promoted significantly greater (∼ 40%) conversion of CD4+CD25−Foxp3− T cells into CD4+CD25+Foxp3+ T cells compared with DCs from control mice. Enhanced Treg function in the post septic host was shown by 2 major findings: (1) increased tumor growth and (2) post septic Tregs inhibited the antitumor effects of CD8+ T cells.
Previous experimental studies have shown that Tregs might contribute to survival after mild polymicrobial septic response during systemic inflammatory response syndrome.6,34-36 Heuer et al36 showed that the adoptive transfer of CD4+CD25+ T cells before or at 6 hours after the induction of CLP had a dose-dependent protective effect on survival. They showed that this protective effect was associated with increased TNF-α levels in the peritoneum.36 However, subsequent studies addressing the effect of Treg depletion by the in vivo administration of anti-CD25 have yielded mixed results about the importance of Tregs for the survival of mice experiencing polymicrobial sepsis. When anti-CD25 monoclonal–depleting antibody was administered either at 48 hours34 or 72 hours6 before CLP surgery, no effect on survival was observed. Conversely, in another sublethal model of polymicrobial sepsis because of CLP surgery, the administration of anti-CD25 antibody resulted in a significant survival advantage.35 These discrepant experimental findings might be the result of the various types of surgery models used to induce polymicrobial sepsis in mice. Several studies, including those from our laboratory, have shown that the severity (ie, the magnitude of the gut trauma and/or peritoneal infection) has a major effect on mouse survival.37
One important and unique focus of the present study was to determine the presence and function of Tregs in severe sepsis survivors. The studies to date, including ours, have indicated that changes in the percentage of Tregs after milder forms of sepsis are transient. For example, Scumpia et al6 and Wisnoski et al34 showed that at day 5 after CLP surgery, the percentage of Foxp3 cells returned to baseline. However, our data after sepsis from its early, acute stage to its later, severe stage showed that Tregs increased suppressive activity and were present at a significantly higher percentage and higher absolute numbers in post septic mice at day 15. All coculture assays in the present study involved CD4+ CD25high T cells that underwent FACS, expressing high levels of Foxp3. Furthermore, the modulation of CTLA-4, CD103, and GITR expression on these cells provided further proof that this population is markedly altered in the post septic host.23-25 We showed that Tregs from post septic mice expressed higher levels of Foxp3, and this increased Foxp3 expression has been shown to correlate with increased Treg function.11,38
In vivo and in vitro studies have shown that naive CD4+CD25−Foxp3− T cells are converted into Foxp3+ Tregs on encounter with other T cells, DCs, or type II monocytes.10,39,40 Because post septic DCs contribute to impaired host responses against infectious agents, in part, due to enhanced IL-10 production,3,16,41 we speculated that the enhanced IL-10 levels produced by these cells might affect Treg conversion. However, the present data did not support this speculation. It is not clear at present which factor(s) is involved in this Treg conversion by post septic DCs. Inflammatory cytokines have been shown to limit Foxp3 induction.28,42 In our present study, the levels of IFN-γ, IL-17, and KC were significantly lower in the cultures containing post septic DCs and T cells than in sham DCs and T cells, suggesting that the conversion with post septic DCs induced Tregs at a higher ratio than Th1 or Th17 cells.
The interaction between the immune system and a nascent tumor initiates a process termed “immunoediting,”43 which may result in one of the following outcomes: (1) elimination of the cancer, (2) cancer equilibrium, and (3) tumor escape and the growth of tumor variants that resist immune destruction.43 Immunosuppression has a clear negative effect on the incidence of cancer, which is apparent from the higher incidence of malignancies in patients who received organ transplants.44 It is evident that Tregs have a significant role in immunoediting by their ability to suppress tumor-associated immunity and to promote immune escape by the tumor.45 On T-cell receptor (TCR) stimulation, Tregs can suppress the proliferation of CD8+ T cells46 and also control the magnitude of effector functions of CD8 T-cell responses particularly in the context of tumors.47 Using 2 in vivo tumor models, we observed that the post septic host failed to elicit an effective antitumor response, resulting in increased growth of both lung cancer and melanoma cells. Lower levels of IFN-γ, IL-17, and TNF-α in the tumor microenvironment from post septic mice might provide one explanation for tumor progression. Although it can promote tumor growth, TNF-α48 is essential for the activation and maturation of CD8+ cytotoxic T lymphocyte effectors.49 Tregs were significantly increased in the tumor-draining LNs from post septic mice, whereas the percentage of CD8+perforin+ T cells and the ratio between CD8+-producing IFN-γ and Tregs were significantly lower in these animals compared with sham controls. The decreased frequency of perforin+CD8+ T cells in post septic mice was not a direct consequence of severe sepsis, because LNs from sham and post septic mice without tumor contained the same percentage of perforin+CD8+ T cells. Thus, the post septic immune response failed to adequately contain tumor growth, and this defect appeared to be due to enhanced Treg function.
Our observation that an adoptive transfer of Tregs from post septic mice impaired antitumor effects of the naive CD8+ T cells in a Rag−/− model is consistent with the hypothesis that the post septic environment favored tumor growth because of Treg expansion. Although we did not address the ability of Tregs to regulate cytotoxic T lymphocyte assay in vitro, our data suggest that post septic Tregs control the cytotoxic functions of CD8+ T cells.47 The Rag−/− mouse experiments showed that the transfer of Tregs from post septic hosts impaired the CD8+ T-cell function. However, this experiment does not exclude the possibility that Tregs from post septic mice have a direct effect on other immune cells such natural killer, DC, macrophages, and other cells in Rag−/− mice bearing tumors. Other possible suppressive mechanisms mediated by post septic Tregs remain to be explored more fully, but the present study shows that Tregs from post septic mice have a crucial inhibitory effect on the antitumor immune response.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Ms Robin Kunkel for graphic artistic assistance and Dr Judith Connett for critical reading of the manuscript. We also thank the University of Michigan Flow Cytometry Core Facility for their technical expertise and assistance. We thank Patricia Rodrigues Marques de Souza for contributing to some of the experiments.
This work was supported by National Institutes of Health grants HL31237, HL31963 (S.L.K.), and CA132571 (V.G.K.).
National Institutes of Health
Authorship
Contribution: K.A.C., Y.D., C.M.H., and S.L.K. designed the experiments; K.A.C. performed the experiments and analyzed and interpreted the data; W.F.C., A.P.M., H.W., M.A.S., M.I., D.M.L., and N.W.L. analyzed and interpreted data; V.G.K. contributed with vital new reagents and analyzed and interpreted data; and K.A.C., V.G.K., C.M.H., and S.L.K. contributed to manuscript preparation.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Steven L. Kunkel, Department of Pathology, University of Michigan Medical School, 109 Zina Pitcher Pl, BSRB, Ann Arbor, MI 48109-2200; e-mail: slkunkel@med.umich.edu; or Karen A. Cavassani, Department of Pathology, University of Michigan Medical School, 109 Zina Pitcher Pl, BSRB, Ann Arbor, MI 48109-2200; e-mail: kcavassa@med.umich.edu.

![Figure 5. Splenic DCs (CD11c+) from post septic mice potently induce Treg conversion. (A) Sham and post septic mice were administrated 0.8 mg/mL BrdU in the drinking water beginning 20 hours before the surgery, and at 48 hours the mice were injected intraperitoneally with 1 mg of BrdU per mouse. At day 3 after surgery, spleen cells were stained for CD4 and Foxp3, and the absolute numbers of CD4+Foxp3+BrdU+ cells were compared between sham and post septic groups from data obtained by flow cytometry. Data represent the mean ± SEM of 3 mice per group. *P ≤ .05, when sham mice are compared with post septic mice. (B-E) Naive CD4+Foxp3− T cells isolated from Foxp3eGFP mice underwent FACS and were cultured in Treg-polarizing conditions or not (ie, no transforming growth factor-β [TGF-β] served as negative control) with post septic or sham splenic DCs (CD11c+MHCII+ or CD8α+) or macrophages (CD11b+CD11c−). The percentage of converted CD4+Foxp3+ T cells is shown (B). (C) Dot plots gated on viable CD4+GFP+ T cells show Foxp3 expression (FJK-16s) after culture in the presence of splenic DCs CD11c+ from sham or post septic mice; numbers in the upper quadrants indicate percentages of CD4+Foxp3− and CD4+Foxp3+ T-cell populations. (D) Percentage of conversion was analyzed on viable CD4+ T cells, and this panel shows the Foxp3 expression in the presence of post septic or sham splenic DCs incubated with blocking anti–IL-10 or IgG control (both 100 μg/mL). All converted Tregs expressed CD25. Data shown are representative of 2 independent experiments (n = 3-5 mice per group) with similar results. Data using DCs (CD11c+) are representative of 3 independent experiments with similar results. (E) The measurement of IFN-γ, KC, and IL-17 by Bioplex on the supernatants derived from the cell-culture conditions are shown as described in panel B.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/115/22/10.1182_blood-2009-09-241083/4/m_zh89991050840005.jpeg?Expires=1767700496&Signature=SzNqwJH-lEgqCMdsN5SzxWQI8VJVl0AUOeFd7~c95npi~6aBrEVFR0je03aeXoQHT-aB3Jhgdpz40qBLOSj2qun9CTBYd3W5qYDZF3nFc4YbI6PUeaGlbty1y2Ou8xczIri34xF5laKcqYyGpZC4ZCSBVGvQSXIjKW14CxyFDQkhZi3airUDDCBCONPyGkoaL1~AnoRczv1J9lF335kTtaA5h1lcg5ldZgNQUSXKqwMCLqu9~wT4BmgoN30wWNAIZM2kf8AH6Unhw5BpThCmL9NB2~j2aPPcUyNrwybWfUX1dWSsYs8u1Cr7jIUAWa7XvPQomsbCfC9RgDHHA6Eeug__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal