To the editor:
Drug-induced immune thrombocytopenia (DITP) may occur after exposure to many medications and is sometimes indistinguishable from idiopathic thrombocytopenic purpura (ITP).1-3 When suspected, the causative drug must be stopped and the platelet count returns to normal in less than a week. Quinine is probably the most common trigger of DITP in outpatients and vancomycin in hospitalized patients.4 Typically, thrombocytopenia and hemorrhagic symptoms occur after one week of exposure to the drug, but they may occur within one day if the patient has been exposed intermittently over a long period.
In May 2008, a 63-year-old man presented with purpura and severe thrombocytopenia a few hours after receiving a bolus of methylprednisolone (MP). In May 2006, he had been diagnosed with primary multiple sclerosis and had received eleven boluses of 1 g of MP without any side effects between December 2006 and March 2008.
On April 16, 2008, 6 hours after a twelfth bolus of MP, the patient noticed diffuse purpura, without any other symptoms. A peripheral blood examination performed 48 hours later showed platelets at 26 × 109/L. No specific treatment was given, and platelets increased spontaneously. On May 28, 4 hours after a bolus of the same MP, the patient again experienced purpura. The following morning, platelets were 7 × 109/L and the patient was hospitalized with diffuse purpura and mild hemorrhage in the buccal cavity, without fever, adenopathy, or hepatosplenomegaly. He denied taking any new medication, including herbal remedies or dietary supplements. Platelets were 19 × 109/L, hemoglobin 157 g/L, and leucocytes 12 × 109/L (80% neutrophils); reticulocytes were low and schyzocytes negative. Creatinine, hepatic tests, C-reactive protein, and lactate dehydrogenase were normal. Electrophoresis showed 10.6 g/L polyclonal gammaglobulins. Antinuclear antibodies, HIV, and hepatis B and C tests were negative.
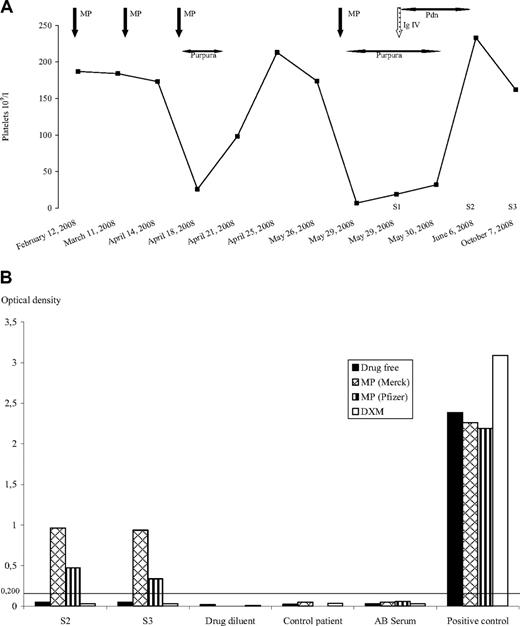
Upon the hypothesis of severe ITP, 40 g of immunoglobulins were administered with prednisolone (40 mg). Platelets increased and the patient was discharged with prednisolone (60 mg/d) and his usual medications. On June 6, platelets were 233 × 109/L and corticosteroids were stopped. No recurrence of purpura occurred (Figure 1A).
Detection of drug-dependent antibodies. (A) Platelet count evolution. (B) Monoclonal antibody-specific immobilization of platelet anti-gene (MAIPA). Platelet antibodies were characterized using CD41 antibodies to immobilize the platelet GpIIb/IIIa. Human platelet antibodies were detected by a peroxidase-conjugated goat anti–human IgG Fcγ fragment. Optical density (OD) at 492 nm was considered negative at less than 0.2 OD units. Negative controls comprised group AB serum and the drug diluent (saline serum). Human polyclonal sera containing anti–HPA-1a, anti–HPA-5b or anti-GpIb/IX activity served as positive controls. S1 volume was insufficient for MAIPA. In assays, drugs were added to incubation and wash solutions at final concentrations of 0.05, 0.1, and 0.2 mg/mL MP, and 0.002, 0.004 and 0.008 mg/mL dexamethasone (DXM). S1, S2, and S3 serum samples. DXM indicates dexamethasone; MP, methylprednisolone; IgIV, intravenous immunoglobulins; and Pdn, prednisolone.
Detection of drug-dependent antibodies. (A) Platelet count evolution. (B) Monoclonal antibody-specific immobilization of platelet anti-gene (MAIPA). Platelet antibodies were characterized using CD41 antibodies to immobilize the platelet GpIIb/IIIa. Human platelet antibodies were detected by a peroxidase-conjugated goat anti–human IgG Fcγ fragment. Optical density (OD) at 492 nm was considered negative at less than 0.2 OD units. Negative controls comprised group AB serum and the drug diluent (saline serum). Human polyclonal sera containing anti–HPA-1a, anti–HPA-5b or anti-GpIb/IX activity served as positive controls. S1 volume was insufficient for MAIPA. In assays, drugs were added to incubation and wash solutions at final concentrations of 0.05, 0.1, and 0.2 mg/mL MP, and 0.002, 0.004 and 0.008 mg/mL dexamethasone (DXM). S1, S2, and S3 serum samples. DXM indicates dexamethasone; MP, methylprednisolone; IgIV, intravenous immunoglobulins; and Pdn, prednisolone.
Serum samples were collected on day one (S1) and 14 days (S2) and 4 months (S3) after the last MP bolus. Another patient treated for multiple sclerosis with the same MP was studied as control. Platelet antibodies were tested using the platelet suspension indirect immunofluorescence test (PSIIFT) and characterized by the monoclonal antibody-specific immobilization of platelet antigens (MAIPA) assay using CD41, CD49b, and CD42a monoclonal antibodies to immobilize platelet Gp IIb/IIIa, Ia/Iia, and Ib/IX, respectively. Sera were tested with and without the drugs methylprednisolone (from Merck and Pfizer) and dexamethasone (Merck).
PSIIFT and MAIPA assays were negative in the absence of drugs, with diluent only, and for the control. In contrast, an IgG antibody was detected by PSIIFT in the presence of MP, which was characterized by MAIPA assay as an anti–Gp IIb/IIIa only in presence of MP. No anti–Gp Ib/IX or anti–Gp Ia/IIa was detected. The IgG anti–Gp IIb/IIIa was identified with both MPs, but not with dexamethasone (Figure 1B).
The patient had level I (definite) evidence for DITP,1 that is, onset of thrombocytopenia after exposure to MP, spontaneous recovery after MP withdrawal, and recurrent thrombocytopenia after reintroduction of MP. Other drugs used before the onset of thrombocytopenia were continued after MP removal with sustained normal platelet count. Multiple sclerosis or other causes for thrombocytopenia, such as infectious disease, lymphoma, or autoimmune disease, were excluded. Moreover, the resolution of the platelet count in a few hours argues against ITP.
The most frequent DITP (“quinine type”) is caused by antibodies that bind to complexes of drug (or drug metabolite) bound to platelet Gp IIb/IIIa, Gp Ib/IX, or both only in the presence of the sensitizing drug.5,6 According to a registry maintained by the University of Oklahoma Health Sciences Center (www.ouhsc.edu/platelets), DITP associated with glucocorticoids has been reported only for prednisolone.7,8 It was more likely a hematosuppressive rather than an antibody-mediated effect of the drug.
These clinical and biologic data demonstrate methylprednisolone-induced immune thrombocytopenia. This presents a paradox when one considers that steroids are part of the treatment of immune thrombocytopenia.
Authorship
Acknowledgments: We thank Dr Marie-Antoinette Sevestre of Amiens University Hospital for critical reading of the manuscript. Manuscript translation by Alison Foote PhD (Clinical Research Center, Grenoble University Hospital, France) was paid by Association pour le Progrès et la Recherche en Oncologie et Maladies Hématologiques (PROMHES).
Contribution: B.R. and K.L. contributed equally to this study. B.G. and F.R. share second authorship. B.R., K.L., B.G., F.R., A.A.K., P.B., and J.P.M. wrote the paper; K.L., A. Colson, A. Camboulives, and P.B. performed research and analyzed data; and B.R., B.G., F.R., A.A.K., and J.P.M. took care of the patient.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Jean Pierre Marolleau, Hematologie clinique, Centre Hospitalier Universitaire, Av Laennec, 80054 Amiens, France; e-mail: Marolleau.jean-pierre@chu-amiens.fr.