Abstract
After the identification of discrete relapse-risk categories in patients with acute promyelocytic leukemia (APL) receiving all-trans retinoic and idarubicin (AIDA)–like therapies, the Gruppo Italiano Malattie Ematologiche dell'Adulto (GIMEMA) designed a protocol for newly diagnosed APL (AIDA-2000) in which postremission treatment was risk-adapted. Patients with low/intermediate risk received remission at 3 anthracycline-based consolidation courses, whereas high-risk patients received the same schedule as in the previous, non–risk-adapted AIDA-0493 trial including cytarabine. In addition, all patients in the AIDA-2000 received all-trans retinoic acid (ATRA) for 15 days during each consolidation. After induction, 600 of 636 (94.3%) and 420 of 445 (94.4%) patients achieved complete remission in the AIDA-0493 and AIDA-2000, respectively. The 6-year overall survival and cumulative incidence of relapse (CIR) rates were 78.1% versus 87.4% (P = .001) and 27.7% versus 10.7% (P < .0001). Significantly lower CIR rates for patients in the AIDA-2000 were most evident in the high-risk group (49.7% vs 9.3%, respectively, P < .0001). Our data confirm that anthracycline-based consolidation is at least equally effective as cytarabine-containing regimens for low-/intermediate-risk patients and suggest that a risk-adapted strategy including ATRA for consolidation improves outcome in newly diagnosed APL. Furthermore, our results highlight the role of cytarabine coupled to anthracyclines and ATRA during consolidation in the high-risk group. This trial was registered at www.clinicaltrials.gov as #NCT 001064570.
Introduction
Although the simultaneous administration of all-trans retinoic acid (ATRA) and anthracycline-based chemotherapy is currently considered the most appropriate induction treatment for newly diagnosed acute promyelocytic leukemia (APL), there is still no consensus on the optimal type and intensity of consolidation therapy.1-3 In 2000, a joint meta-analysis of the Spanish Programa para el Estudio y Tratamiento de las Hemopatias Malignas (PETHEMA) and the Italian Gruppo Italiano Malattie Ematologiche dell'Adulto (GIMEMA) groups was carried out to identify relapse risk criteria in APL patients who had received an identical AIDA (ATRA and idarubicin) induction and a similar anthracycline-containing chemotherapy consolidation. The resulting prognostic score that segregated discrete relapse risk groups based on initial leukocyte and platelet counts4 led to the design of 2 risk-adapted trials in which consolidation varied according to the risk category. Using increased anthracycline doses in the high-risk group, the PETHEMA reported an improved antileukemic efficacy in this category as well as an overall improvement of results in all groups.5,6
The GIMEMA risk-adapted trial was designed with the aim of investigating the effects on patient outcome of 2 main modifications from the original AIDA-0493 protocol: the omission of cytarabine in the low-/intermediate-risk group and the addition of ATRA during consolidation for all risk categories. We report here the results in adult patients 18 to ≤ 61 years of age of the GIMEMA risk-adapted AIDA-2000 study compared with the previously adopted AIDA-0493 trial.
Methods
The AIDA-0493 trial for newly diagnosed APL was started in April 1993 and closed in May 2000; it was opened to all ages and involved 81 institutions. The preliminary results of the AIDA-0493 in adults and children have been published in 2 separate reports.7,8 The successive AIDA-2000 study was designed for patients 1 to ≤ 61 years of age, was initiated in June 2000, and closed for the majority of GIMEMA centers in October 2006, when a new phase 3 (still ongoing) trial was activated. A total of 68 institutions participated in the trial (see the supplemental Appendix, available on the Blood Web site; see the Supplemental Materials link at the top of the online article). The AIDA-2000 study, however, is still open to registration for few institutions experiencing delays in local institutional review board approval for the phase 3 trial and for all patients in the high-risk category. The present report is a comparative study of adult patients 18 to ≤ 61 years of age entered in the 2 studies, whereas the results in the pediatric series as well as those in the elderly cohort of the AIDA 4093 will be reported separately.
Eligibility
Patients 1 to ≤ 61 years of age with newly diagnosed APL were initially enrolled in the study and could start treatment based on the sole morphologic diagnosis of APL based on French-American-British criteria. Confirmation of the presence of t(15;17) by karyotyping and/or of the PML/RARA fusion by reverse-transcribed polymerase chain reaction (RT-PCR) in leukemic cells was, however, a mandatory requirement for eligibility, and patients lacking genetic confirmation of diagnosis were considered ineligible and subsequently excluded from the study. Diagnostic samples were sent as per protocol to the central laboratory at the Department of Cellular Biotechnologies and Hematology of the University La Sapienza in Rome, for confirmation of genetic diagnosis and identification of the PML/RARA fusion type. Other eligibility criteria were normal hepatic and renal function, Eastern Cooperative Oncology Group performance status less than 3, no cardiac contraindication for intensive chemotherapy, and left ventricle ejection fraction greater than 50%. Informed consent was obtained from all patients according to the Declaration of Helsinki. The protocol was approved by the institutional review board of each participating institution.
Study design
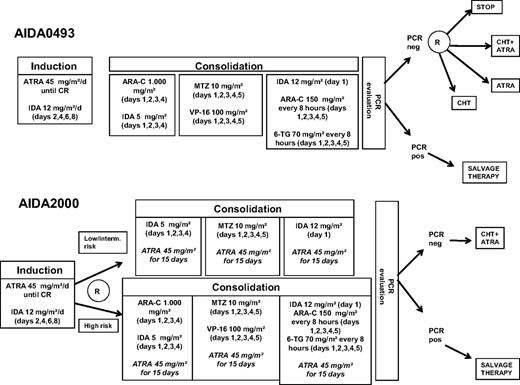
The detailed schedule of the 2 successive AIDA-0493 and AIDA-2000 protocols is shown in Figure 1.
AIDA-0493 and AIDA-2000 protocol design. IDA indicates idarubicin; MTZ, mitoxantrone; VP-16, etoposide; ARA-C, cytarabine; 6-TG, 6-thioguanine; and CHT, chemotherapy (6-mercaptopurine + methotrexate).
AIDA-0493 and AIDA-2000 protocol design. IDA indicates idarubicin; MTZ, mitoxantrone; VP-16, etoposide; ARA-C, cytarabine; 6-TG, 6-thioguanine; and CHT, chemotherapy (6-mercaptopurine + methotrexate).
Induction.
The induction schedule of the AIDA-2000 protocol was identical to that of the AIDA-0493, which combined oral ATRA (45 mg/m2 per day) until complete remission (CR) or for a maximum of 45 days and 4 doses of intravenous idarubicin 12 mg/m2 on days 2, 4, 6, and 8.
Consolidation.
Consolidation therapy in the AIDA-0493 trial consisted of 3 chemotherapy courses without ATRA as reported.7 After the initial report of the PETHEMA LPA96 trial5 and the joint PETHEMA-GIMEMA study defining relapse risk categories,4 consolidation treatment in the AIDA-2000 was given according to a risk-adapted strategy as follows: patients with low-/intermediate-risk (initial white blood cell [WBC] < 10 × 109/L) received the same 3 consolidation courses as in the AIDA-0493 but with omission of cytarabine from courses 1 and 3 and omission of etoposide from course 2; patients in the high-risk group (ie, WBC > 10 × 109/L) received the identical 3 cycles as in the AIDA-0493. In addition, distinct from the AIDA-0493, oral ATRA at 45 mg/m2 per day for 15 days was added in the AIDA-2000 at the start of each consolidation course for all risk groups (Figure 1).
CNS prophylaxis.
Before the initiation of each consolidation cycle, patients in the high-risk group of the AIDA-2000 trial received intracranial prophylaxis with methotrexate (12 mg) and 6-methylprednisolone (40 mg) for a total of 3 courses.
Maintenance.
Patients in the AIDA-0493 who tested PCR-negative after consolidation were initially (up to January 1997) randomized into 4 maintenance arms (ie, low-dose chemotherapy vs low-dose chemotherapy plus ATRA vs ATRA alone vs observation) as reported.7 Based on an interim analysis showing better results in the 2 ATRA-containing arms, starting from February 1997, the AIDA-0493 was amended by closing the 2 maintenance options not containing ATRA (G.A. et al, manuscript submitted, August 2010), and patients were randomly assigned to ATRA alone versus low-dose chemotherapy plus ATRA.
Patients in the AIDA-2000 who tested RT-PCR negative for PML/RARA at the end of consolidation were given maintenance with low-dose chemotherapy with oral 6-mercaptopurine (50 mg/m2) and intramuscular methotrexate (15 mg/m2) alternating with oral ATRA for 15 days every 3 months for a total of 2 years, as in arm 3 of the AIDA-0493. The reason for keeping this maintenance in the AIDA-2000 was because a higher number of relapses were initially observed in the AIDA-0493 for patients not receiving ATRA-containing maintenance. Doses of chemotherapy were decreased by 50% if WBC count was less than 3.5 × 109/L and discontinued if less than 2.5 × 109/L. Patients in either study who tested PCR-positive after the completion of third consolidation course were considered as having resistant disease and given salvage therapy.
Supportive measures.
During the entire duration of induction therapy, prednisone at the dose of 0.5 mg/kg per day was administered to prevent APL differentiation syndrome. Tranexamic acid was given in the AIDA-0493 at the dose of 100 mg/kg per day as continuous intravenous infusion if the platelet count was less than 50 × 109/L and discontinued when the platelet count was more than 50 × 109/L. Because antifibrinolytic therapy did not apparently attenuate the hemorrhagic risk, this policy was no longer followed in the AIDA-2000. Platelets and fresh frozen plasma were transfused to maintain platelet count more than 30 × 109/L and fibrinogen more than 150 mg/dL. Packed red cell concentrates were given to maintain hemoglobin level more than 8 g/dL. Prophylactic heparin was not recommended. At the earliest manifestations of suspected APL differentiation syndrome and before development of a full-blown syndrome, ATRA treatment was temporarily discontinued and dexamethasone given intravenously at 10 mg/12 hours for 4 days or until disappearance of symptoms and signs of the syndrome. Pseudotumor cerebri, defined as the presence of severe headache with nausea, vomiting, papilloedema, and visual disorders was treated by analgesics, osmotic diuretics, and temporarily discontinuation of ATRA.
Laboratory monitoring during treatment.
Complete blood and platelet counts were performed daily. Coagulation analyses (prothrombin time, activated thromboplastin time, fibrinogen, fibrinolytic degradation products, or cross-linked fibrin) were performed daily until normalization of the coagulopathy and then twice a week. Kidney and liver function analyses were obtained twice a week. Bone marrow samples for morphologic and RT-PCR evaluation were obtained at the time of hematologic CR after induction and at the end of consolidation.
RT-PCR of PML/RARA.
RT-PCR experiments to detect the PML/RARA fusion and characterize the transcript type were carried out in bone marrow or (when appropriate, in limited cases with significant blast infiltration) in peripheral blood samples. Studies at remission were always performed in bone marrow samples. Mononuclear cells, obtained by centrifuging specimens on a Ficoll-Hypaque density gradient, were washed twice in sterile phosphate-buffered saline, suspended in a 4M guanidium thiocyanate (GTC) solution, and stored at −20°C. These procedures were performed in each GIMEMA center using RNAase-free disposable materials and a GTC solution prepared by the referral molecular biology laboratories and distributed to all GIMEMA peripheral centers. Samples cryopreserved in GTC were then sent in dry ice to the reference molecular biology laboratory for RT-PCR studies. Total RNA was extracted by the method of Chomczynski and Sacchi.9 The integrity of RNAs was assessed in all diagnostic and remission samples by electrophoretic run through a formaldehyde minigel. The protocol and the primers used to amplify the PML/RARA hybrid gene have been reported elsewhere. To assess the efficiency of the RT step and to further verify RNA integrity, the ABL gene was simultaneously amplified as an internal control in each case. A positive control (amplification of RNA extracted from the promyelocytic cell line NB4 or from a patient with PML/RARA short type isoform) and a negative control (all reagents plus water with no RNA) were included in each experiment. To assess the sensitivity of our RT-PCR method, total RNA isolated from a diagnostic sample with 100% blastic infiltration was serially diluted by mixing it with the t(15;17) negative myeloid cell line GF-D8 RNA. Our assay allowed us to detect the PML/RARA transcript in the presence of 0.1 ng of total RNA, which is a final dilution of 10−4.
Outcome definitions and statistical analysis
Hematologic CR (HCR) was defined as the reconstitution of normal marrow cellularity with less than 5% leukemic promyelocytes, together with peripheral blood cell counts of polymorphonuclear leukocytes more than 1500/μL and platelets more than 100 000/μL. Molecular remission (mCR) was defined as the disappearance, on an ethidium bromide-stained electrophoresis gel, of the specific PML/RARA amplification band identified at diagnosis, in the presence of RNA integrity as evaluated by minigel visualization and successful amplification of the ABL gene used as internal control. Molecular relapse was defined as reappearance of RT-PCR positivity (test sensitivity 10−4) at any time after achievement of mCR at the end of consolidation, confirmed in 2 successive BM samples collected 2 to 4 weeks apart. Overall survival (OS) was defined as the time from the diagnosis to death from any cause. Disease-free survival (DFS) was defined as the time from HCR achievement to relapse (either hematologic or molecular), persistence of PCR positivity after consolidation, death, or date of last follow-up for patients alive in first mCR. Cumulative incidence of relapse (CIR) was calculated from the time of HCR achievement to relapse (hematologic or molecular), persistence of PCR positivity after consolidation, or date of last follow-up for patients alive in first mCR, using the cumulative incidence method and considering death in mCR and death in HCR (during consolidation therapy) as competing risk. The log-rank test was used to compare risk factor categories for the Kaplan-Meier curves and the Gray test for the incidence curves. Median follow-up time was estimated by reversing the codes for the censoring indicator in a Kaplan-Meier analysis. Multivariate analysis for HCR achievement after induction was performed by the logistic regression; results were expressed as odds ratios (± 95% confidence intervals [CIs]). Differences in the distribution of prognostic factors in subgroups were analyzed by c2 or Fisher exact test, and by the Kruskal-Wallis test. All tests were 2-sided, accepting P ≤ .05 as indicating a statistically significant difference. Analyses were performed by SAS Version 9.1.3 statistical software.
Results
A total of 1095 patients with genetically proven APL diagnosis were included in the present comparative analysis. Of these, 642 and 453 patients (age, > 18 ≤ 61 years) were enrolled in the AIDA-0493 trial and the AIDA-2000, respectively. The median follow-up of the 2 cohorts at the time of the analysis was 7.8 years and 4.9 years, respectively. Demographic and baseline characteristics of patients included in the 2 studies are shown in Table 1. The 2 series were comparable in terms of sex, presenting WBC and platelet counts, PML/RARA transcript type, and Sanz risk score.4 A significant difference was found in age distribution, with younger median age being recorded in the AIDA-0493 compared with the AIDA-2000 (38.2 vs 40.9 years, respectively, P = .02).
Demographic and baseline features of patients enrolled in the AIDA-0493 and AIDA-2000 trials
| Characteristic . | Median (range) . | AIDA-0493 (n = 642) . | Median (range) . | AIDA-2000 (n = 453) . | P . |
|---|---|---|---|---|---|
| Sex | |||||
| Male | — | 349 (54.4%) | — | 229 (50.5%) | .1089 |
| Female | — | 293 (45.6%) | — | 224 (49.5%) | |
| Age, y | 38.2 (18.0-60.7) | — | 40.9 (18.0-61.0) | — | .0193 |
| WBC count, ×109/L | 2.8 (0.3-570.0) | — | 2.3 (0.3-770.0) | — | .3494 |
| Platelet count, ×109/L | 24.0 (1.0-241.0) | — | 24.0 (0.5-264.0) | — | .8165 |
| PML/RARA isoform | |||||
| Bcr1 | — | 321 (56.4%) | — | 191 (54.2%) | |
| Bcr2 | — | 43 (7.6%) | — | 33 (9.4%) | |
| Bcr3 | — | 205 (36.0%) | — | 128 (36.4%) | |
| Unknown | — | 73 | — | 101 | .5889 |
| Relapse risk | |||||
| Low | — | 130 (20.4%) | — | 116 (25.6%) | |
| Intermediate | — | 331 (52.0%) | — | 208 (45.9%) | |
| High | — | 176 (27.6%) | — | 129 (28.5%) | |
| Unknown | — | 5 | — | 0 | .0744 |
| Characteristic . | Median (range) . | AIDA-0493 (n = 642) . | Median (range) . | AIDA-2000 (n = 453) . | P . |
|---|---|---|---|---|---|
| Sex | |||||
| Male | — | 349 (54.4%) | — | 229 (50.5%) | .1089 |
| Female | — | 293 (45.6%) | — | 224 (49.5%) | |
| Age, y | 38.2 (18.0-60.7) | — | 40.9 (18.0-61.0) | — | .0193 |
| WBC count, ×109/L | 2.8 (0.3-570.0) | — | 2.3 (0.3-770.0) | — | .3494 |
| Platelet count, ×109/L | 24.0 (1.0-241.0) | — | 24.0 (0.5-264.0) | — | .8165 |
| PML/RARA isoform | |||||
| Bcr1 | — | 321 (56.4%) | — | 191 (54.2%) | |
| Bcr2 | — | 43 (7.6%) | — | 33 (9.4%) | |
| Bcr3 | — | 205 (36.0%) | — | 128 (36.4%) | |
| Unknown | — | 73 | — | 101 | .5889 |
| Relapse risk | |||||
| Low | — | 130 (20.4%) | — | 116 (25.6%) | |
| Intermediate | — | 331 (52.0%) | — | 208 (45.9%) | |
| High | — | 176 (27.6%) | — | 129 (28.5%) | |
| Unknown | — | 5 | — | 0 | .0744 |
— indicates not applicable.
Induction therapy
Table 2 shows the results of induction therapy. Of 1095 eligible patients, 1081 were evaluable for induction response. A total of 600 of 636 patients (94.3%) achieved CR in the AIDA-0493 trial compared with 420 of 445 patients (94.4%) enrolled in the AIDA-2000 trial (P = 1.00). A total of 14 patients (6 in the AIDA-0493 and 8 in the AIDA-2000) were not evaluable because of pretherapy death (2 and 1 cases, respectively), protocol violation (2 and 6 cases), and incomplete data (2 and 1 cases). Thirty-five patients (5.5%) died during induction in the AIDA-0493 compared with 25 (5.6%) in the AIDA-2000 trial. No significant differences were recorded in the causes of death during induction among the 2 protocols (Table 2). Differentiation syndrome was reported during induction in 82 (13%) and 46 (11%) cases in the AIDA-0493 and AIDA-2000 trials, respectively (P = .31), and was fatal in 1 case in each series. One patient was considered resistant in the AIDA-0493 trial and none in the new protocol. Multivariate analysis for induction response (Table 3) showed presenting WBC count at diagnosis (P = .003) and age (P = .024) as unfavorable factors for HCR achievement and platelet count at diagnosis as a favorable factor (P = .049).
Induction results and causes of induction death
| . | AIDA-0493 . | AIDA-2000 . | P . |
|---|---|---|---|
| CR | 600 (94.3%) | 420 (94.4%) | |
| Induction death | 35 (5.5%) | 25 (5.6%) | |
| Resistance | 1 (0.2%) | 0 | 1.0000 |
| Causes of induction death | Hemorrhage (13) | Hemorrhage (8) | |
| Infection (5) | Infection (5) | ||
| Other (9) | Other (5) | ||
| Thromboembolism (3) | Thromboembolism (1) | ||
| Myocardial infarction (1) | Myocardial infarction (2) | ||
| Renal failure (2) | Renal failure (1) | ||
| Differentiation syndrome (1) | Differentiation syndrome (1) | ||
| Unknown (1) | Unknown (2) |
| . | AIDA-0493 . | AIDA-2000 . | P . |
|---|---|---|---|
| CR | 600 (94.3%) | 420 (94.4%) | |
| Induction death | 35 (5.5%) | 25 (5.6%) | |
| Resistance | 1 (0.2%) | 0 | 1.0000 |
| Causes of induction death | Hemorrhage (13) | Hemorrhage (8) | |
| Infection (5) | Infection (5) | ||
| Other (9) | Other (5) | ||
| Thromboembolism (3) | Thromboembolism (1) | ||
| Myocardial infarction (1) | Myocardial infarction (2) | ||
| Renal failure (2) | Renal failure (1) | ||
| Differentiation syndrome (1) | Differentiation syndrome (1) | ||
| Unknown (1) | Unknown (2) |
Multivariate analysis for induction response
| . | Odds ratio (95% CI) . | P . |
|---|---|---|
| WBC at diagnosis (as continuous variable) | 0.995 (0.992-0.998) | .0030 |
| Age at diagnosis (as continuous variable) | 0.973 (0.950-0.996) | .0238 |
| Platelets at diagnosis (as continuous variable) | 1.012 (1.000-1.023) | .0491 |
| Protocol: AIDA-2000 vs AIDA-0493 | 1.039 (0.604-1.786) | .8910 |
| . | Odds ratio (95% CI) . | P . |
|---|---|---|
| WBC at diagnosis (as continuous variable) | 0.995 (0.992-0.998) | .0030 |
| Age at diagnosis (as continuous variable) | 0.973 (0.950-0.996) | .0238 |
| Platelets at diagnosis (as continuous variable) | 1.012 (1.000-1.023) | .0491 |
| Protocol: AIDA-2000 vs AIDA-0493 | 1.039 (0.604-1.786) | .8910 |
Consolidation therapy
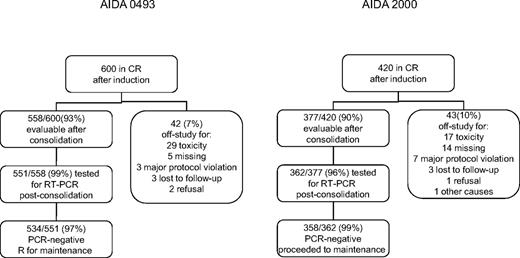
Figure 2 reports a flowchart with patients remaining on protocol after induction and after consolidation, number of cases excluded for toxicity, deaths in remission, and other causes of dropout in the 2 studies. Four and 8 patients died during consolidation in the AIDA-0493 and AIDA-2000, respectively. Two of 4 deaths in the 0493 study were the result of infection, and both were recorded in the low-/intermediate-risk group. On additional patient with intermediate-risk disease died of progressive disease during consolidation, and for 1 case the cause of death was not specified. Of 8 deaths in CR in the AIDA-2000, 4 were the result of infection; of these, 2 occurred in the low-/intermediate-risk and 2 in the high-risk group. Of the 4 remaining deaths in this study, 2 were the result of hemorrhage and occurred in high-risk patients, 1 (high-risk) to thromboembolism, and 1 (intermediate) to Guillain-Barré syndrome. During the neutropenic phase of consolidation courses, the fraction of patients with no episodes of infection or fever of unknown origin (FUO) was 116 of 573 (20.2%) and 191 of 386 (49.5%) in the AIDA-0493 and AIDA-2000, respectively (P < .0001). This statistical difference reflected a lower incidence of infection or FUO episodes in low-/intermediate-risk patients in the AIDA-2000 trial (115 of 286) compared with the AIDA-0493 (339 of 423; P < .0001), whereas in the high-risk patients, the incidence of infection or FUO was similar in the 2 cohorts (80 of 100 vs 117 of 149, P = .78); data not shown).
Flowchart of patients on- and off-study and reasons for exclusion after remission induction.
Flowchart of patients on- and off-study and reasons for exclusion after remission induction.
Toxic episodes that resulted in dropping off study were mostly (28 of 29) recorded in low-/intermediate-risk patients of the AIDA-0493 (where all patients received more intensive treatment) with toxicity attributed to prolonged neutropenia, FUO, or documented infection in the majority of cases. By contrast, in the AIDA-2000, the majority of toxicities resulting in exclusion from study during CR (10 of 17) were in the high-risk group (ie, in patients receiving more intensive treatment). Here again, for the AIDA-2000, prolonged neutropenia, FUO, or documented infection were the main cause of dropout during consolidation
RT-PCR tests for the PML/RARA fusion gene were carried out in a total of 913 patients at the end of the third consolidation course. Molecular remission was documented in 534 of 551 (96.9%) and in 358 of 362 (98.9%) tested patients in the AIDA-0493 and AIDA-2000 trials, respectively (P = .07). As per study design, 17 patients in the AIDA-0493 and 4 patients in the AIDA-2000 who showed persistence of residual disease after consolidation in 2 successive RT-PCR tests were excluded from randomization and given salvage therapy.
Outcome
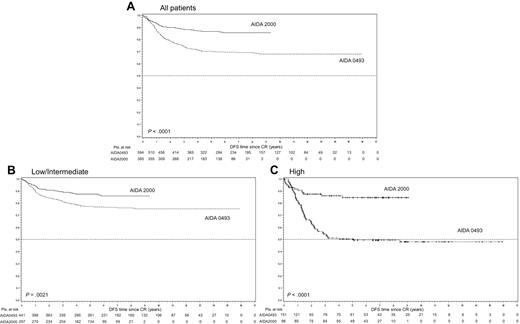
Outcome results are summarized in Table 4 and Figures 3 to 5. The probability of remaining alive after 6 years was 78.1% (95% CI, 75.6%-80.8%) in the AIDA-0493 study and 87.4% (95% CI, 84.6%-90.3%) in the AIDA-2000 (P = .0010). The 6-year estimated DFS was 69.5% (95% CI, 66.9%-72.2%) in the AIDA-0493 and 85.6% (95% CI, 82.4%-88.9%) in the AIDA-2000 (P < .0001, Figure 3A). For low-/intermediate-risk patients, the DFS at 6 years was 76.6% (95% CI, 73.5%-79.8%) versus 85.9% (95% CI, 82.1%-89.8%; P = .0021, Figure 3B); considering the high-risk patients, the DFS at 6 years was 49.6% (95% CI, 45.7%-53.8%) in the AIDA-0493 study versus 84.5% (95% CI, 78.4%-91.2%) in the AIDA-2000 trial (P < .0001, Figure 3C).
OS, DFS, and CIR estimates
| Risk group . | Protocol . | OS at 6 y (95% CI) . | P . | DFS at 6 y (95% CI) . | P . | CIR at 6 y (95% CI) . | P . |
|---|---|---|---|---|---|---|---|
| All patients | AIDA-0493 | 78.1% (75.6-80.8) | .0010 | 69.5% (66.9-72.2) | < .0001 | 27.7% (27.7-27.8) | < .0001 |
| AIDA-2000 | 87.4% (84.6-90.3) | 85.6% (82.4-88.9) | 10.7% (10.6-10.8) | ||||
| Low/intermediate | AIDA-0493 | 84.7% (81.9-87.7) | .1516 | 76.6% (73.5-79.8) | .0021 | 19.9% (19.8-19.9) | .0016 |
| AIDA-2000 | 89.1% (85.8-92.5) | 85.9% (82.1-89.8) | 11.2% (11.2-11.3) | ||||
| High | AIDA-0493 | 61.3% (56.9-66.0) | .0010 | 49.6% (45.7-53.8) | < .0001 | 49.70% (49.4-50.1) | < .0001 |
| AIDA-2000 | 83.4% (78.1-89.0) | 84.5% (78.4-91.2) | 9.3% (9.1-9.5) |
| Risk group . | Protocol . | OS at 6 y (95% CI) . | P . | DFS at 6 y (95% CI) . | P . | CIR at 6 y (95% CI) . | P . |
|---|---|---|---|---|---|---|---|
| All patients | AIDA-0493 | 78.1% (75.6-80.8) | .0010 | 69.5% (66.9-72.2) | < .0001 | 27.7% (27.7-27.8) | < .0001 |
| AIDA-2000 | 87.4% (84.6-90.3) | 85.6% (82.4-88.9) | 10.7% (10.6-10.8) | ||||
| Low/intermediate | AIDA-0493 | 84.7% (81.9-87.7) | .1516 | 76.6% (73.5-79.8) | .0021 | 19.9% (19.8-19.9) | .0016 |
| AIDA-2000 | 89.1% (85.8-92.5) | 85.9% (82.1-89.8) | 11.2% (11.2-11.3) | ||||
| High | AIDA-0493 | 61.3% (56.9-66.0) | .0010 | 49.6% (45.7-53.8) | < .0001 | 49.70% (49.4-50.1) | < .0001 |
| AIDA-2000 | 83.4% (78.1-89.0) | 84.5% (78.4-91.2) | 9.3% (9.1-9.5) |
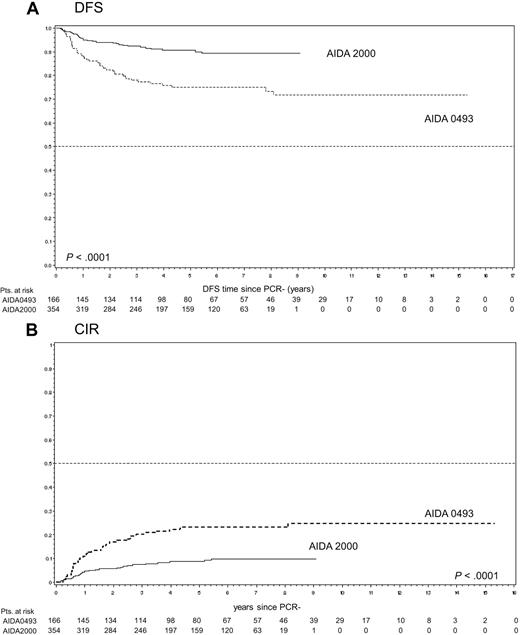
DFS and CIR (resulting from the attainment of PCR-negative postconsolidation) in patients with homogeneous maintenance treatment (ATRA + chemotherapy).
DFS and CIR (resulting from the attainment of PCR-negative postconsolidation) in patients with homogeneous maintenance treatment (ATRA + chemotherapy).
Relapse rate and patterns of relapse
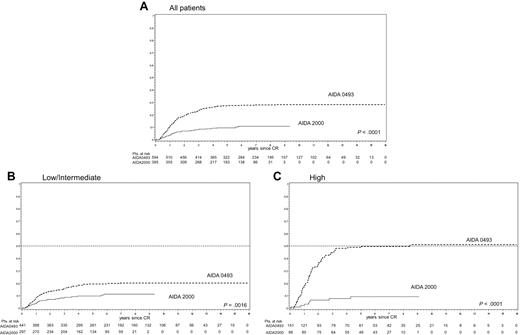
The 6-year CIR rate was 27.7% (95% CI, 27.7%-27.8%) and 10.7% (95% CI, 10.6%-10.8%; P < .0001, Figure 4A) considering all risk groups in the 2 studies. The CIR rate comparing together low-/intermediate-risk patient groups was 19.9% (95% CI, 19.8%-19.9%) for patients enrolled in the AIDA-0493 study and 11.2% (95% CI, 11.2%-11.3%) for patients in the AIDA-2000 trial (P = .0016). Finally, as to high-risk patients, the 6-year CIR rate was 49.7% (95% CI, 49.4%-50.1%) and 9.3% (95% CI, 9.1%-9.5%) for patients in the AIDA-0493 and AIDA200, respectively (P < .0001). The majority of relapses (ie, 75% and 65% in the AIDA-0493 and AIDA-2000, respectively) were recorded within 2 years from achievement of molecular remission. There were no significant differences in either protocols regarding the time to relapse (early vs late relapses) when risk categories were analyzed separately (ie, high-risk vs low-/intermediate-risk) To better analyze the impact of maintenance randomization on relapse in the AIDA-0493 study, the CIR starting from achievement of molecular remission at the end of consolidation was calculated according to maintenance type. Patients receiving no maintenance had more events compared with all other groups, although the difference was not statistically significant (data not shown). Moreover, the majority of relapses occurred at an early time (ie, within 2 years) in patients in the observation arm, although they more frequently occurred beyond 2 years in the other groups. A more detailed final analysis of the effect of maintenance randomization on relapses in the AIDA-0493, including impact on distinct risk groups, will be reported in a separate study (G.A. et al, manuscript submitted, August 2010). As to the site of relapse in the 2 protocol, data are reported in Table 5. The percentage of CNS relapses in patients in CR was 2.5% and 2.1% in the AIDA-0493 and AIDA-2000, respectively. The CIR in the CNS calculated for all patient in CR was similar in the 2 studies (2.6% vs 2.4%, P = .89).
Types of relapse by protocol
| Type of relapse . | AIDA-0493, no. (%) . | AIDA-2000, no. (%) . | Total, no. . |
|---|---|---|---|
| BM | 95 (61.69) | 14 (42.42) | 109 |
| CNS | 7 (4.55) | 3 (9.09) | 10 |
| CNS + BM | 8 (5.19) | 6 (18.18) | 14 |
| Other extramedullary | 7 (4.55) | 0 (0) | 7 |
| Molecular | 36 (23.38) | 10 (30.30) | 46 |
| Mixed (molecular and extramedullary) | 1 (0.65) | 0 (0) | 1 |
| Total | 154 | 33 | 187 |
| Type of relapse . | AIDA-0493, no. (%) . | AIDA-2000, no. (%) . | Total, no. . |
|---|---|---|---|
| BM | 95 (61.69) | 14 (42.42) | 109 |
| CNS | 7 (4.55) | 3 (9.09) | 10 |
| CNS + BM | 8 (5.19) | 6 (18.18) | 14 |
| Other extramedullary | 7 (4.55) | 0 (0) | 7 |
| Molecular | 36 (23.38) | 10 (30.30) | 46 |
| Mixed (molecular and extramedullary) | 1 (0.65) | 0 (0) | 1 |
| Total | 154 | 33 | 187 |
To compare patients receiving homogeneous maintenance treatment, we carried out a subanalysis of DFS and CIR rates (starting from the time of mCR achievement, after third consolidation) comparing AIDA-2000 patients with those in the AIDA-0493 who were randomized to the ATRA plus low-dose chemotherapy maintenance. As illustrated in Figure 5, the results showed a better outcome for AIDA-2000 patients (P < .0001). The results of longitudinal RT-PCR monitoring studies of PML/RARA, together with details on the type of relapse and data about PCR outcome prediction, and results of salvage therapies according to the type of relapse (molecular vs hematologic) will be reported in a separate study. Relapses of any type were reported in a total of 154 of 600 (25%) and 33 of 420 (8%) patients in CR in the AIDA-0493 and AIDA-2000 studies, respectively. Fifteen of 154 (9.7%) and 9 of 33 (27%) relapses occurred in the CNS in the 2 studies. Eight of 15 CNS relapses in the AIDA-0493 and 4 of 9 CNS relapses in the AIDA-2000 were reported in high-risk patients.
Discussion
This study shows that a risk-adapted postremission strategy using variable chemotherapy intensity and ATRA for consolidation results in significant outcome improvement in patients with newly diagnosed APL. The benefit hereby reported comparing the 2 successive GIMEMA studies appears to result both from reduced toxicity and from increased antileukemic efficacy in the new AIDA-2000 study, as clearly shown considering together all outcome estimates and toxicity data. The improved outcome was evident for all risk categories but was most striking in the high-risk group. Of note, although the 2 series were comparable for the main clinical variables, such as initial WBC count and Sanz risk score4 distribution, the AIDA-2000 trial included patients with significantly older median age. Apart from the comparison of the 2 series as a whole, important and most interesting differences emerged from analyzing separately the results in the distinct risk groups.
With respect to induction results, our data confirm the very high efficacy of the AIDA protocol using concomitant ATRA and single-agent chemotherapy with idarubicin. This scheme has been successfully validated in other studies,5,6 which independently showed, as in our studies, a virtual absence of resistant disease in patients with genetically proven APL. Patient characteristics associated with increased risk of induction death as resulting from our multivariate analysis were in keeping with those reported by others3 and in particular with the recent data published by de la Serna et al for patients receiving the identical AIDA regimen for induction.10
As regarding postinduction results in the low-/intermediate-risk categories, our main objective in designing the AIDA-2000 trial was to test the hypothesis that cytarabine and other nonintercalating agents, such as etoposide, could be safely omitted from consolidation without compromising therapeutic efficacy, as initially suggested by the PETHEMA LPA96 trial.5 Our data support this view and are in agreement with those from several other studies, including the successive risk-adapted LPA99 trial and the LPA2005,6 the French-Spanish meta-analysis,11 and the randomized MRC-PETHEMA trial.12 Taken together, the results of these studies indicate that cytarabine may be safely removed from the front-line treatment of non–high-risk APL patients, allowing to significantly spare toxicity in this important patient subset, which accounts for up to 70% to 75% of the entire APL population.6,11,12 However, concerning our data, it should be noted that the AIDA-2000 protocol differed from the previous AIDA study, not only for the omission of cytarabine and etoposide but also for the inclusion of ATRA during consolidation. Although the benefit apparently resulting from this modification was less striking than that observed in the high-risk group, one might speculate that the addition of ATRA compensated for the less intensive chemotherapy in this patient group and provided still significant improvements of DFS and CIR rates in the AIDA-2000 compared with AIDA-0493. However, it is important to recognize that another difference in the 2 studies consisted of the inclusion of ATRA-containing maintenance for all enrolled patients in the AIDA-2000, whereas as per study design half of the patients in the AIDA-0493 did not receive ATRA maintenance. It is conceivable that this modification might have contributed to the improved outcome seen in the new trial.
The results obtained in the high-risk category by comparing the 2 studies are most remarkable, particularly when we consider that the main modification in the AIDA-2000 with respect to the AIDA-0493 study was the addition of ATRA during each consolidation cycle. Our results provide compelling evidence that better outcome in the AIDA-2000 was mostly the result of significantly increased antileukemic efficacy, as clearly shown by the impressive improvement in CIR rate, which represents the best estimate reliably reflecting antileukemic efficacy. It should be noted that patients in this group experienced similar toxicity in the 2 successive studies with no significant differences being recorded in therapy-related deaths and side effects.
As to the patterns of relapse hereby reported, we observe that, also because of the limited numbers of events, our study does not allow to draw firm conclusions regarding CNS relapse and the effects of prophylaxis. In particular, intrathecal prophylaxis as planned in the AIDA-2000 study for high-risk patients did not apparently decrease the risk of developing CNS disease. In this respect, it may be hypothesized that the absence of CNS relapses reported in the French APL2000 trial11 reflects the higher number of intrathecal injections given as prophylaxis in that study compared with ours. However, the optimal CNS prophylaxis yet remains to be established.
After the initial report of our study,13 the PETHEMA group adopted the same schedule, including cytarabine and ATRA during consolidation for high-risk patients (LPA2005 trial). A recent analysis of this Spanish study14 reported similar results with an 11% CIR rate at 3 years in the high-risk group and improved outcome compared with their previous risk-adapted protocol using increased anthracycline doses, instead of cytarabine, in this patient category. Although the biologic reasons underlying the remarkable improvement in therapeutic efficacy brought by adding ATRA to chemotherapy are presently unclear to us, we can speculate that ATRA may synergize with cytarabine and/or etoposide, resulting in increased cytotoxicity and overall antileukemic efficacy. This view is, on the other hand, supported by in vitro observations showing increased cytotoxicity for cytarabine on pretreatment with ATRA in cell line systems.15,16
Recent approaches aimed at reducing treatment-related toxicity in APL have been attempted by several groups, including the North American Intergroup who studied the combination of arsenic trioxide with chemotherapy during consolidation in a randomized trial. The preliminary results of this study indicated a significant benefit in using this strategy.17 Based on accumulating experience on the efficacy of arsenic trioxide in front-line management of APL17-22 and the preliminary analysis of the AIDA-2000 study, the GIMEMA group designed in 2006 the new currently ongoing phase III trial for newly diagnosed patients, which compares the ATRA plus arsenic trioxide regimen originally reported by Estey et al22 versus the AIDA-2000 regimen (antracycline-based) for non–high-risk APL, whereas patients in the high-risk categories are being treated with the present AIDA-2000 schedule also including cytarabine and etoposide during consolidation. Although it will be unrealistic to demonstrate a superiority in terms of antileukemic efficacy in the current trial, the new study aims at answering the challenging question of whether at least similar efficacy results may be achieved with a no-chemotherapy approach, which holds the theoretical potential of carrying reduced treatment-related toxicity in this highly curable disease.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Mrs Sandra De Simone (GIMEMA Data Manager).
This work was supported in part by the Associazione Italiana contro le Leucemie, the Associazione Italiana per la Ricerca sul Cancro, and the Progetto Integrato Oncologia (Ministero della Salute).
Authorship
Contribution: F.L.-C., G.A., and F.M. designed the study; F.L.-C., G.A., and M.V. analyzed and interpreted the data; F.L.-C. and M.B. wrote the paper; E.G., A.R., G.F., F. Ferrara, G.S., G.C., E.B., G.M., F.D.R., E.D.B., A.P., A.B., A.M.C., F. Fabbiano, E.M.P., M.C.P., and S.A. included data of patients treated in their institutions, reviewed the manuscript, and contributed to the final draft; F.P. and P.F. carried out statistical analyses; and D.D. performed molecular tests.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
A complete list of GIMEMA participants is available in the online supplemental Appendix.
Correspondence: Francesco Lo-Coco, Department of Biopathology, University Tor Vergata, Via Montpellier 1, 00133 Rome, Italy; e-mail: francesco.lo.coco@uniroma2.it.